The U.S. Will Cover the Bulk of Medicines Spending in 2020
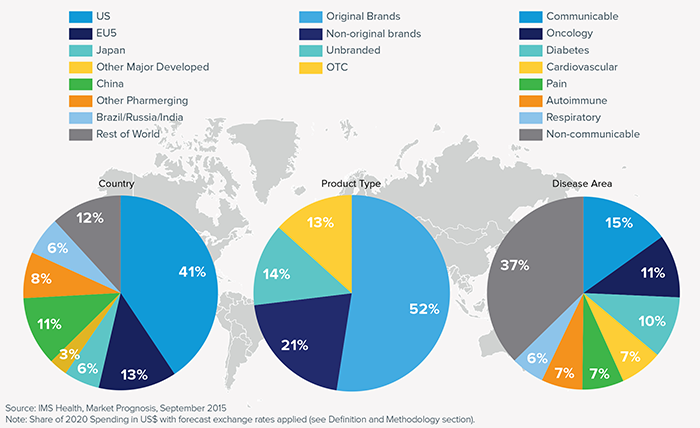
U.S. spending on medicines will approach $590 billion in 2020, increasing 34% over 2015, IMS Institute for Healthcare Informatics projects in its forecast, Global Medicines Use in 2020. Growth in spending will be attributable to innovation (new products), price increases and some patent losses of exclusivity (e.g., branded drugs going generic). The U.S. will cover the bulk of drugs spending in 2020 at 41% of the world medicines market, shown in the first pie in the first chart. U.S. medicines spending dwarfs any other country or region in the world, including China which is expected to account for 11% of
Activity Wearables on Black Friday 2015 – Doorbusters Abound

The 2015 holiday shopper can find activity trackers for gifting discounted as much as 50% and more over Thanksgiving weekend. In greater Philadelphia, the Thursday print newspaper ads were chock full of examples from Best Buy, Dick’s Sporting Goods, Kohl’s, Target, and Walmart, among others. Among the many “Doorbusters” and deep discounts were a Misfit Flash tracker for $14.99 at Best Buy (a 50% discount), a Fitbit Zip at both Kohl’s and Walmart for $39 ($20 off the manufacturers’ suggested retail price), and a Fitbit Flex at Dick’s Sporting Goods for $49.95 — 50% off full retail. That trackers are
51% of Americans Say It’s Government’s Responsibility To Provide Health Insurance
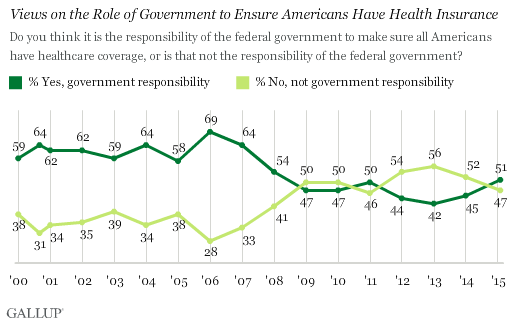
For the first time since 2008, a majority of Americans say government is responsible for ensuring that people have health insurance. The first chart shows the crossing lines between those who see government-assured health insurance in the rising dark green line in 2015, and people who see it as a private sector responsibility. The demographics and sentiments underneath the 51% are important to parse out: people who approve of the Affordable Care Act are over 3x more likely to believe in government sponsoring health insurance versus those who disapprove, 80% compared with 26%. The demographic differences are also striking, detailed
The Average Price of a New Specialty Drug Exceeds Median U.S. Annual Income; and a Tweet from Pam Anderson
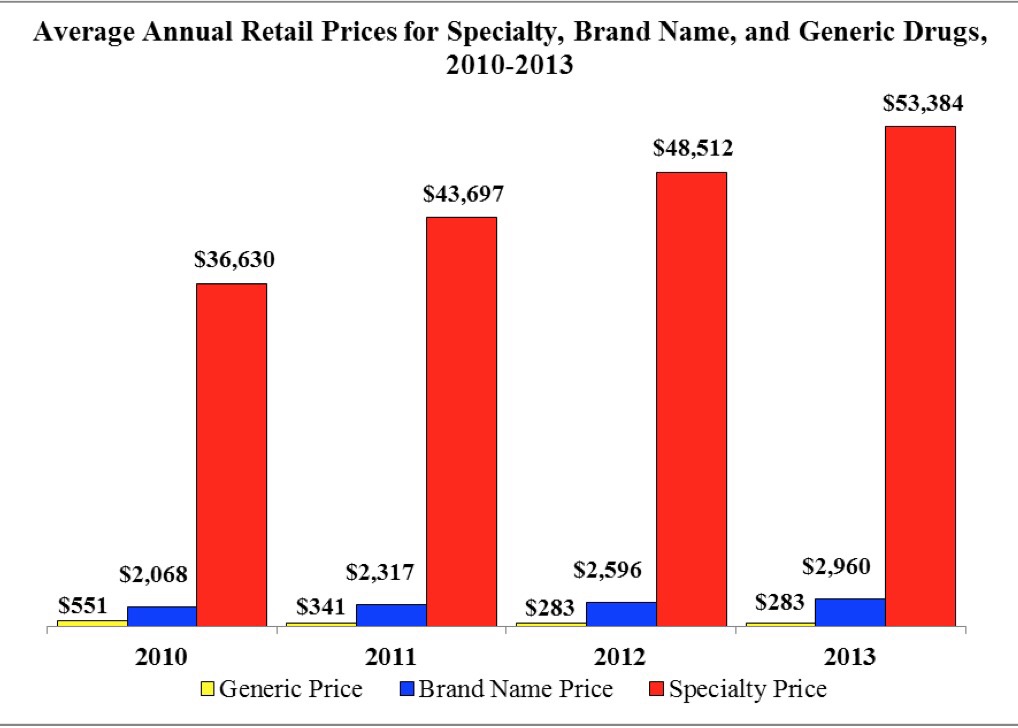
The average price for a specialty drug was $53,384 in 2013; the average household income was $52,250. Thus, even allocating 100% of a family’s annual earnings to pay for a drug wouldn’t stretch far enough to cover it in 2013, nor would it do so today in 2015. This sober health economic artifact comes from the latest Rx Price Watch Report from the AARP, detailing cost trends for prescription drugs across all segments — generics, brands and specialty drugs. Contrast, as well, the $53K for the average specialty drug with the median 2013 Social Security benefit payout of $15,526 and median Medicare
American health citizens hungry for cost controls
Most Americans support price controls on drug and medical device manufacturers, hospitals, and payments to doctors, along with allowing Medicare to negotiate drug prices. U.S. health citizens, now consumers, have been experiencing sticker-shock when it comes to prices on medical bills upon hospital discharge, leaving the doctor’s office, filling a prescription at a pharmacy or receiving a specialty drug recommended for a serious medical condition. The HealthDay/Harris Poll of 5 November 2015 quantifies their observation that Americans Want Bold Steps to Keep Health Care Costs in Check. The topline of the Poll shows that: 73 percent support price controls on
Retail Health Landscape Expanding Through Clinic Growth, Accenture Forecasts
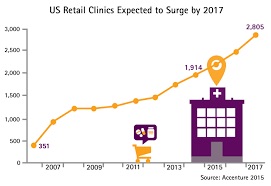
The Old School retail clinic is going beyond checking your child’s ear infection and sore throat, giving immunizations and filling out back-to-school forms just-in-time over LaborDay weekend. The new-new retail clinic is supporting patients’ chronic disease management, partnering with academic medical centers, and bolstering medication management. Accenture’s bullish forecast is titled “US Retail Health Clinics Expected to Surge by 2017,” making the case that these brick-and-mortar providers are shifting from a relatively limited retail scope to a broader and deeper clinical focus. The so-called surge in the number of retail clinics is projected to be nearly 50% growth between 2014 and 2017,
My Breakfast With Alain – On Health Consumers and the New Retail Health

My National Health Care Consumer Week, I’ll coin this, looking back on flying some 12,000 airmiles over six days, criss-crossing America from the City of Brotherly Love to Sacramento, back to Philly and then to Los Angeles. Finally, today, heading home to Philadelphia and my beloved, most necessary Tempur-Pedic bed, a loving husband and some therapeutic TV binge-watching. It’s Friday and I’m at LAX, reflecting on a week of meeting with three groups of healthcare executives and stakeholders who all wanted to hear my take on the evolution of patients, people, caregivers, all, morphing into health care consumers. The lens
Walgreens Extends Telehealth On Your Smartphone
In the U.S., if you walk 3 miles in any direction, there’s a 3 in 4 chance you’ll find yourself in front of a Walgreens pharmacy. The company often says that 75% of people in the America live within 3 miles of a Walgreens storefront. What’s a pharmacy storefront anymore? Both Walgreens and CVS are re-defining that with a dizzying pace of new announcements. The latest for Walgreens: people in 25 states will be able to use the Walgreens app on their smartphones to access physicians virtually. Consumers living in Alabama, Arizona, California, Colorado, Connecticut, Florida, Indiana, Illinois, Iowa, Maryland,
Getting to Connected Health Is A Marathon, Not A Sprint
Consumers may demand connected experiences in daily living, but there have been many barriers to health care industry stakeholders delivering on that expectation: among them, privacy and security concerns, and provider resistance. This demand-and-supply chasm is noted in Deloitte’s Center for Health Solutions’ latest look into the healthcare landscape, Accelerating the adoption of connected health. The objectives of connected health, or cHealth, are: To improve digital connectivity among consumers, providers, health plans and life sciences companies To facilitate self-managed care in a secure environment that protects privacy To deliver care outside of traditional institutional settings To enable chronic care management
Social Determinants Impact Health More Than Health Care
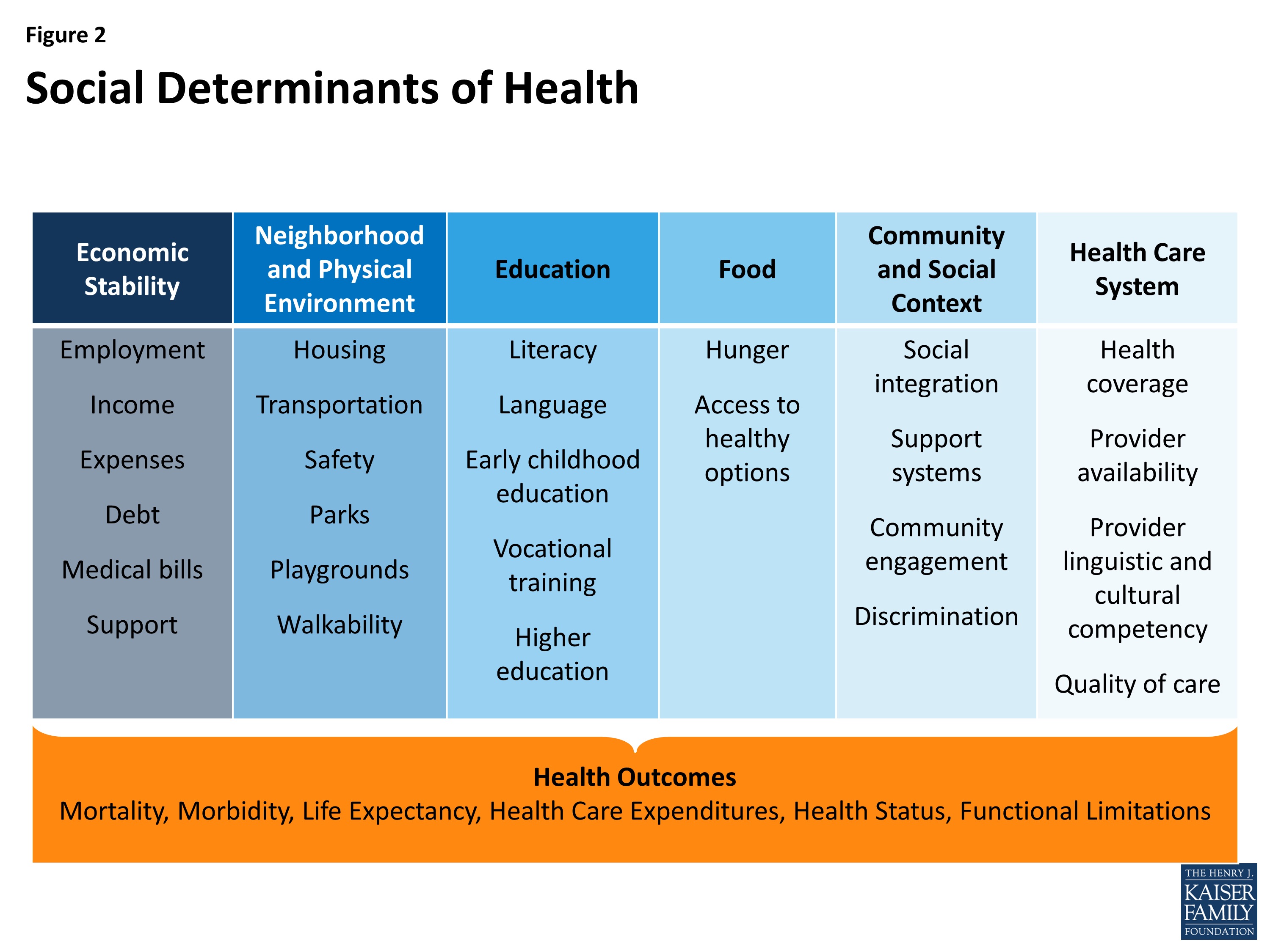
The factors of where people are born, live, work and age — social determinants — shape human health more than health care. Yet in the U.S. much more resource per capita is funneled into healthcare services than into social ones. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity was published by The Kaiser Commission on Medicaid and the Uninsured in November 2015, calling attention to the opportunity and wisdom of baking health into all public policy. The social determinants of health (SDOH) include economic stability, the physical environment and neighborhood, education, food, community and
The Telephone Is As Digital As It Gets in Mainstream U.S. Health Care
The phone continues to be the platform technology used in this digital age of health care, according to Better Together: High Tech and High Touch, a survey report sponsored by the Bipartisan Policy Center and the Council of Accountable Physician Practices. Nielsen’s Strategy Health Perspectives project polled 5,014 U.S. adults in June and July 2015 for this study. According to the study sponsors, this is the largest consumer population studied conducted to-date on the topic of digital health use and demand. The first chart illustrates the reality of digital health in the U.S. 2015: that notwithstanding the availability of telehealth,
U.S. Health At A Glance – Not So Healthy
People in the U.S. have lower life expectancy, a growing alcohol drinking problem, and relatively high hospital inpatient rates for chronic conditions compared with other OECD countries. And, the U.S. spends more on health care as a percent of GDP than any other country in the world. This isn’t new-news, but it confirms that U.S. health citizens aren’t getting a decent ROI on health spending compared with health citizens around the developed world. In the OECD’s latest global look at member countries’ health care performance, Health at a Glance 2015, released today, the U.S. comes out not-so-healthy in the context
Death Rates Rise For Middle-Age White Men: Economics and Mental Health in America
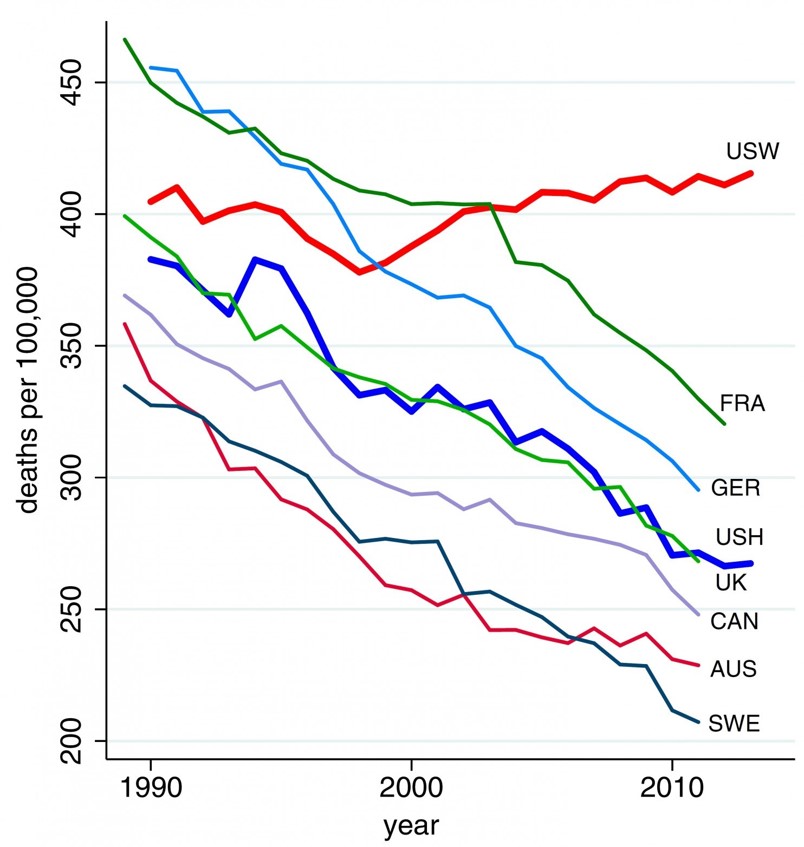
Shocking statistics were published in this week’s Proceedings of the National Academy of Sciences showing rising death rates for middle-age men. The major causes: suicide, drug and alcohol poisoning, and liver diseases. The line chart illustrates the death rates per 100,000 population of U.S. whites (“USW”), the top line on the graph, compared with 45-54 year old men in France, Germany, the United Kingdom, Canada, Australia, and Sweden — along with U.S. Hispanic males (“USH”) — for whom death rates have fallen since 1990. The authors note that the increase in midlife mortality is only partly understood. Increased availability of





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.