CVS Health in Talks to Acquire Aetna – The Changing Retail Health Landscape

Just a few days since CVS Health announced the company would be working with mega-health insurer Anthem on a prescription drug management program, the pharmacy chain today is reportedly in talks to buy Aetna, the national health insurance company, according to CNBC and other credible news outlets like the Wall Street Journal. Remember that Aetna’s bid to acquire Humana was scuttled earlier this year after many months of negotiation and positioning, along with FTC scrutiny about antitrust. That insurance merger “died” on one day in February 2017 along with an Anthem-CIGNA deal, covered here by CNN. A deal between CVS
In the Post-Weinstein Era, How to Market Health to Women: Philips, Kalenji, and Libresse Getting It Right

“With Mad Men still in charge, ad campaigns miss the mark,” an editorial published this week in the Financial Times asserts. Leave it to a fiscally conservative British publication to be spot-on about a particularly, but not uniquely, American challenge, in this post-Weinstein (Miramax), -Price (Amazon), and today, -Halperin (MSNBC) moment of sexual harassment revelations. In health/care, women are key consumers, buyers and influencers, yet under-represented in the Mad Men demographic of senior advertising executives, as the data-driven FT essay points out. So it’s especially heartening to find this month a few examples of empowering, inspiring ad campaigns getting health/care marketing
Health (Healthcare, Not So Much) Abounds in Prophet’s Top 50 Brands

U.S. consumers’ most-valued brands include Apple, Google, Amazon, Netflix, Pinterest, Android, Spotify, PIXAR, Disney and Samsung, according to the 2017 Brand Relevance Index from Prophet. The top 50 are shown in the first chart. On the second chart, I’ve circled in red the brands that have reach into healthcare, health, fitness, and wellness. Arguably, I could have circled every brand in the top 50 because in one way or another, depending on the individual, people find health “everywhere” that’s relevant to them based on their own definitions and value-systems. This is Prophet’s third year conducting this study, and I was
Four Things We Want in 2017: Financial Health, Relationships, Good Food, and Sleep

THINK: money and love. To find health, working-aged people seek financial stability and good relationships, according to the Consumer Health POV Report from Welltok, meQuilibrium, and Zipongo, featured in their webinar broadcast today. The online consumer survey was conducted among 2,000 full-time working U.S. adults in August 2017, segmented roughly into thirds by Boomers (37%), Gen Xers (32%), and Millennials (31%). Much lower down the priority list for healthy living are managing food, sleep, and stress based on the poll. Feeling stress is universal across most consumers in each of the three generational cohorts, especially related to work and finance.
President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update
Last week, President Trump once again used the “M” word (“murder”) in a sentence accusing the pharmaceutical industry of too-high priced products for U.S. health citizens. The sentence included the phrase, “Drug companies are getting away with murder.” That week, USA Today published an article on a new FDA-approved specialty drug therapy that could add up to over a $1 mm price tag. There is much to report in the world of pharmaceutical innovation, pricing, and patient Rx coverage this month. The CVS Health – Epic announcement ranks high in Health Populi’s vision for the evolving health/care ecosystem, bringing together two
Income Inequality For Older Americans Among Highest in the World – What This Means for Healthcare
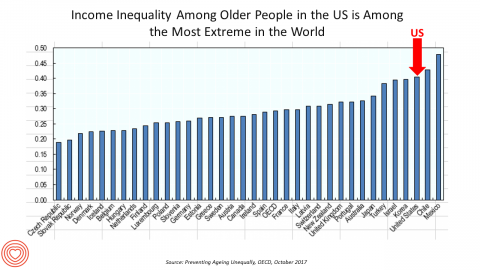
Old-age inequality among current retirees in the U.S. is already greater than in ever OECD country except Chile and Mexico, revealed in Preventing Ageing Unequally from the OECD. Key findings from the report are that: Inequalities in education, health, employment and income start building up from early ages At all ages, people in bad health work less and earn less. Over a career, bad health reduces lifetime earnings of low-educated men by 33%, while the loss is only 17% for highly-educated men Gender inequality in old age, however, is likely to remain substantial: annual pension payments to the over-65s today are
Most Consumers Would Trust a Health Info Site “Prescribed” by Their Doctor
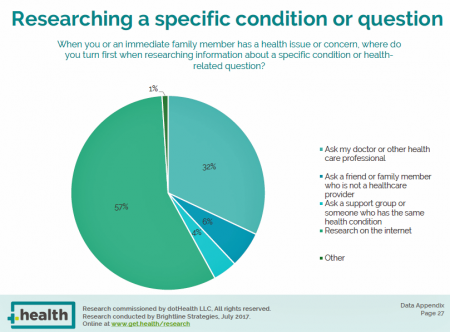
Most consumers access the Internet for health information before they ask their doctor for the same information. But virtually everyone who goes online for health information would trust a website recommended to them by their doctor, according to the dotHealth Consumer Health Online – 2017 Research Report. This survey was conducted on behalf of dotHealth, an internet registry company channeling “.health” domains to organizations in the broad health and healthcare landscape. [FYI, both Health Populi and JaneSarasohnKahn are also registered with .health domains, having availed ourselves of this service at launch]. Six in 10 consumers who have used the internet in the
Most Americans Are Concerned About Healthcare Policy, and Costs Top the List of Concerns
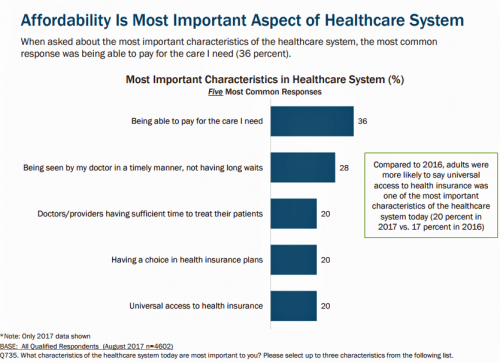
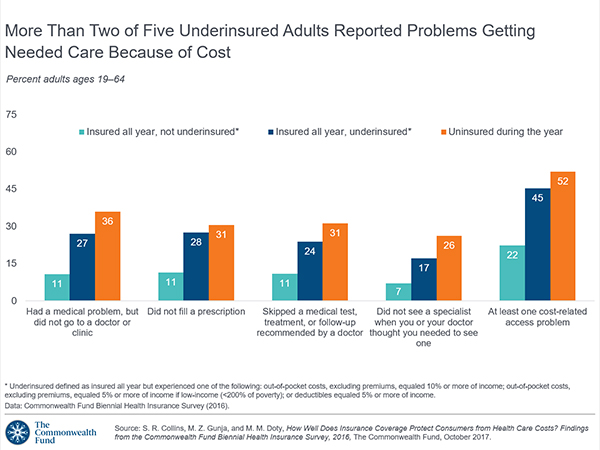
4 in 5 Americans are aware of potential changes to healthcare policy brewing in Washington, DC. 92% of them are concerned about those changes, according to Healthcare Consumers in a Time of Uncertainty, the fifth annual survey from Transamerica Center for Health Studies. Peoples’ most-shared fears are losing their coverage for pre-existing conditions, out-of-pocket spending, and a ban on lifetime limits. That boils down to one thing: cost. That is, cost, for having to spend money on services not-covered by their health insurance plan; cost for out-of-pocket items under-insured, denied, or requiring coinsurance or co-payments; and, catastrophic costs that rise beyond
What Health Plans Must Learn from Amazon
One in two U.S. consumers told Aflac that enrolling in health insurance should feel like an experience on Amazon. But health consumers still lack that high benchmark retail experience with health plans, based on new research published in HealthMine’s 2017 Health Intelligence Report focusing on communication and digital healthcare tools. “Most members believe health plan communications are impersonal and centered around bills rather than healthcare guidance,” HealthMine asserts in the introduction to the report. That’s about as un-Amazon as we can imagine. Top findings from HealthMine’s research are that: 3 in 4 consumers don’t think their health insurance plan
What Patients Feel About Technology, Healthcare Costs and Social Determinants
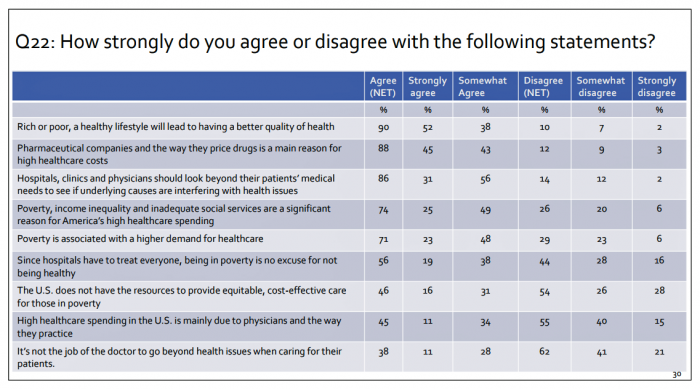
U.S. consumers feel positive about the roles of technology and social determinants in improving healthcare, but are concerned about costs, according to the 2017 Patient Survey Report conducted for The Physicians Foundation. The survey gauged patients’ perspectives across four issues: the physician-patient relationship, the cost of healthcare, social determinants of health, and lifestyle choices. Two key threads in the research explain how Americans feel about healthcare in the U.S. at this moment: the role of technology and the cost of health care. First, the vast majority of consumers view technology, broadly defined, as important for their health care. 85% of people
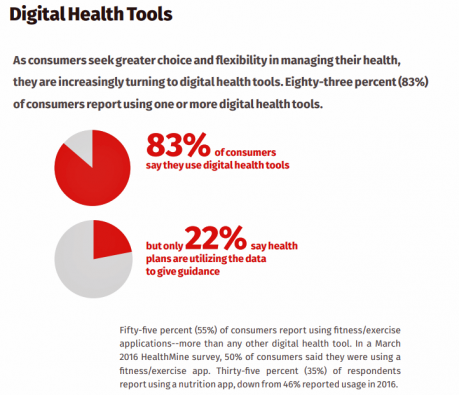
Consumers Use Digital Health Tools But Still Struggle with Health Literacy

While more U.S. patients are use digital health tools and take on more clinical and financial decision making for their health care, people also have gaps in health engagement and health literacy. Three studies published in early October 2017 provide insights into the state of healthcare consumerism in America. The 2017 UnitedHealthcare Consumer Sentiment Survey found that a plurality of Americans (45%) turn first to primary care providers (doctors or nurses) as their source for the first source of information about specific health symptoms, conditions or diseases. 28% of people also use the internet or mobile health apps as their
The Rx is UX: A Prescription for EHRs and Patient Engagement
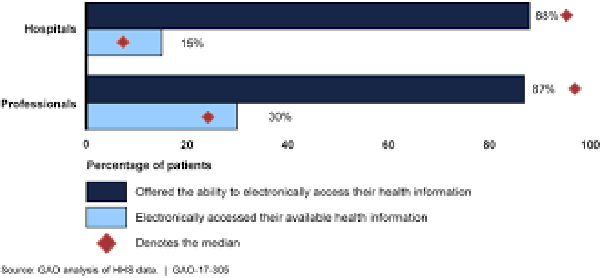
It’s National Health IT Week (#NHIT Week), and I’m revisiting research published earlier this year to connect the dots between EHR implementation (good news: it’s nearly universal in doctors’ offices and hospitals) and patients embracing their health information (not-so-much). What’s missing: UX design and respect for peoples’ life-flows. Most physician practices and hospitals in the U.S. have installed electronic health records (EHRs). But in a classic Field of Dreams scenario, we have made patients’ medical records digital, but people aren’t asking for them or accessing them en masse. “How do we make it easier for patients to request and manage their
The Patient Is The Vector: Health 2.0 – Day 2 Learnings
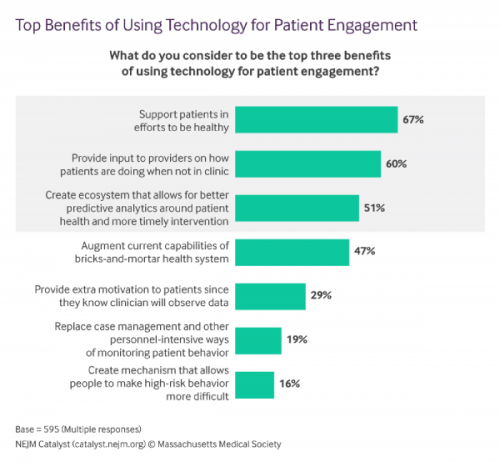
Question: “What is the opposite of ‘patient-centered care?'” asked a panelist on Day 1 of the 11th Annual Health 2.0 Conference. Answer: “‘Physician-centered care.'” Even physicians today see the merits of patient engagement, as this survey from New England Journal of Medicine found earlier this year. Since the launch of the first Health 2.0 Conference in 2007, the patient has played a growing role in session content and, increasingly, on the big stage and panel breakout sessions. A panel I attended on Day 2 convened five developers of patient engagement platforms and digital tools to help healthcare look and
Leveraging the Essential Data of Life: Health 2.0 – Day 1 Learnings

The future of effective and efficient healthcare will be underpinned by artful combinations of both digital technologies and “analog humans,” if the first day of the Health 2.0 Conference is a good predictor. Big thoughts about a decentralized future in healthcare kicked off Day 1 of the 11th annual Health 2.0 Conference in Santa Clara, CA. The co-founders of Health 2.0 (H20), Matthew Holt and Indu Subaiya, explained the five drivers of the tech-enabled health future. 1. The new interoperability, underpinned by FHIR standards and blockchain. “FHIR” stands for fast healthcare interoperability resources, which are informatics standards that enable data
The Patient As Payor – Americans Bundle Financial Wellness and Healthcare Costs
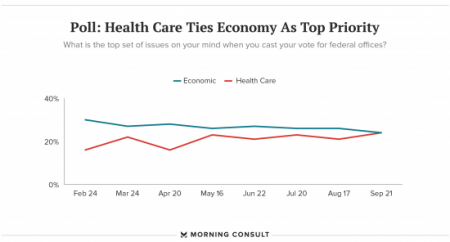
Healthcare and the economy tied for US voters’ top issue last week, as the prospects for repealing the Affordable Care Act faded by the weekend. This Morning Consult poll was published 28th September 2017, as it became clear that the Graham-Cassidy health reform bill would lose at least three key votes the legislation needed for passage: from Rand Paul, Susan Collins, and John McCain. Liz Hamel, who directs the Kaiser Family Foundation’s survey research, told Morning Consult that, “when people say ‘health care,’ they often are actually talking about the economic issue of health care.”





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.