Two news stories this week highlight the fact that, even with a health reform bill signed and sealed by the President of the United States, and with $20 billion of ARRA stimulus funding on the books, electronic health records adoption will probably be slower than the go-go forecasts of one year ago.
The head of Accenture’s clinical transformation practice was interviewed by Information Week this week. Dr. Kip Webb explained the results of an Accenture survey of small practices that found a “substantial number” of physicians in practices smaller than 10 doctors would not begin the process of EMR adoption. On the upside, Accenture learned that about 6 in 10 physicians did intend to adopt EMRs in the next two years — especially those under the age of 55 and those not in the smallest (solo or duo) practice settings.
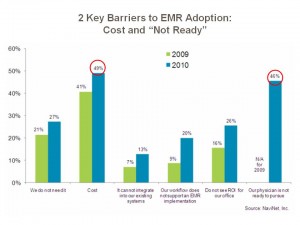
For those doctors over 55 and those who practice in solo and duo groups, it’s cost — which cuts in two ways. First, for the smallest cottage-industry practice, there’s not the scale (or perception thereof) to rationalize the cost of acquiring an EMR system. Second, for the oldest physicians, there may not be the longer-term payback/ROI to justify the cash outlay for the new system. Either way, cost is a barrier to EMR adoption — even with the promise of a $44,000 incentive payment.
Another study, by NaviNet, found that there has been an uptick in the past six months among physicians interested in implementing an EMR. The company’s survey in 2009 found that 9% of physician practices with 10 or fewer physicians planned to adopt EMRs in the next six months. In March 2010, 12% of these small practices have plans to implement EMRs.
At the same time, the percentage of physicians with no plans to implement an EMR fell: in 2009, 31% of physicians said they would not implement an EMR system; in 2010, that percentage dropped to 21%.
![]()
Free, or cheap, is in the eye of the beholder. Cost of EMR adoption should be considered through the lenses of opportunity cost as well as life-cycle cost for physicians, For those in smaller practices and those who are older, the cost may be too high vis-a-vis the scale or practice, or time horizon for achieving a desired return-on-investment.
The second obstacle to adoption — the “I’m just not ready” factor — is less quantifiable but no less justifiable or visceral to the practicing doctor. This can be the hassle factor of disrupting workflow, the cultural factor of not wanting to bring computers into the practice, or simply the unwillingness to change what appears to be working well.
By 2014, in the last year of the EMR stimulus payments, we’ll get to well over 50% of EMR adoption overall. That means that millions of patient records will be digitized, and data will be mined that measures what clinically works, and what doesn’t. Payers will be informed and enabled to pay providers for performance, and health citizens will be able to meaningfully follow their own numbers. This emerging era of data liquidity is what President Obama had in mind when he earmarked $20 billion for stimulus funding. Even if the U.S. doesn’t get to universal EMR adoption by 2014, the nation will have significantly moved toward data liquidity and informed clinical decision making and financing.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...