“Will Work For Health Care:” Americans Trading Off Wages For Healthcare (Again)
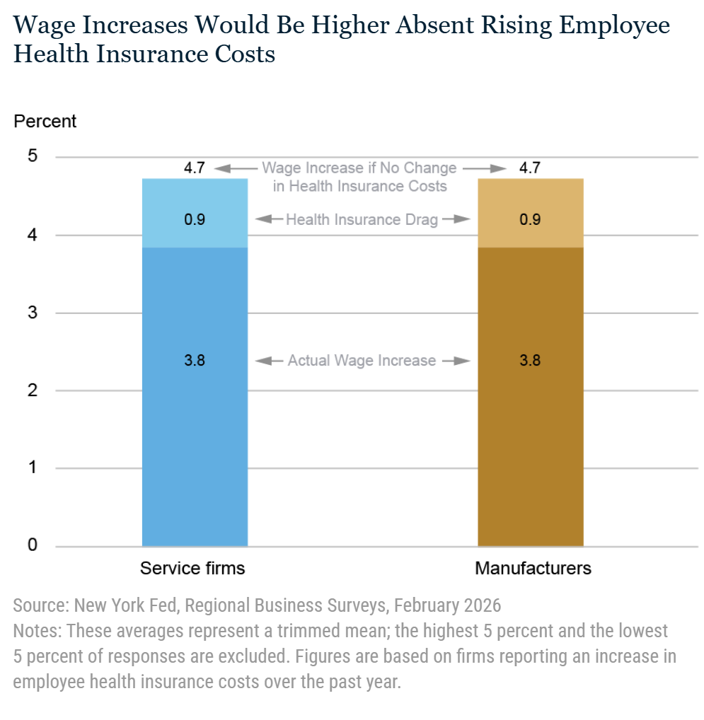
Many people living in America who receive health benefits at the workplace traded off wage growth for health insurance coverage, a report from the Federal Reserve Bank of New York published this week. For those of us working in the health economics and policy space since the 1990s, the Fed team gave me a strong sense of déjà vu. The bar graph cited in the report explains the math behind the wage/health plan trade-off. “Among those businesses experiencing an increase in employee health insurance costs, the average wage increase over
Why Clorox Talks about Hygiene at Home: Health, Wellbeing, and the Home as Health Hub

The COVID-19 pandemic was a watershed era for people re-assessing and re-imagining their homes as hubs for health, healthcare, and well-being (as well as learning, exercising, and baking sourdough bread). This graphic comes from my book, Health Citizenship: How a Virus Opened Hearts and Minds, written in the midst of the pandemic based on consumers’ newly adopted behaviors during the #workfromhome and #stayhome epoch. We experienced the digital transformation of people through life and home-based work and education, a growing sense of DIY for things we could do
Dr. Wachter Bets on A Giant Leap for AI in Health Care
“Stop worrying and let AI help save your life,” a New York Times op-ed prescribed in January. So I wanted to ask Dr. Robert Wachter, author of that essay, “why not worry?” and read his latest book, A Giant Leap, before speaking with him. I spent time with Bob on a Zoom session last week to dig into some patient/consumer-facing issues regarding AI and health care. Before I launch into our engaging conversation, I’d like to share some context about Dr. Wachter and his evolution that I believe makes him
Financial Stress and Trust in Health Care Takes Many Forms – Listening to Jarrard’s 2026 State of Play Survey
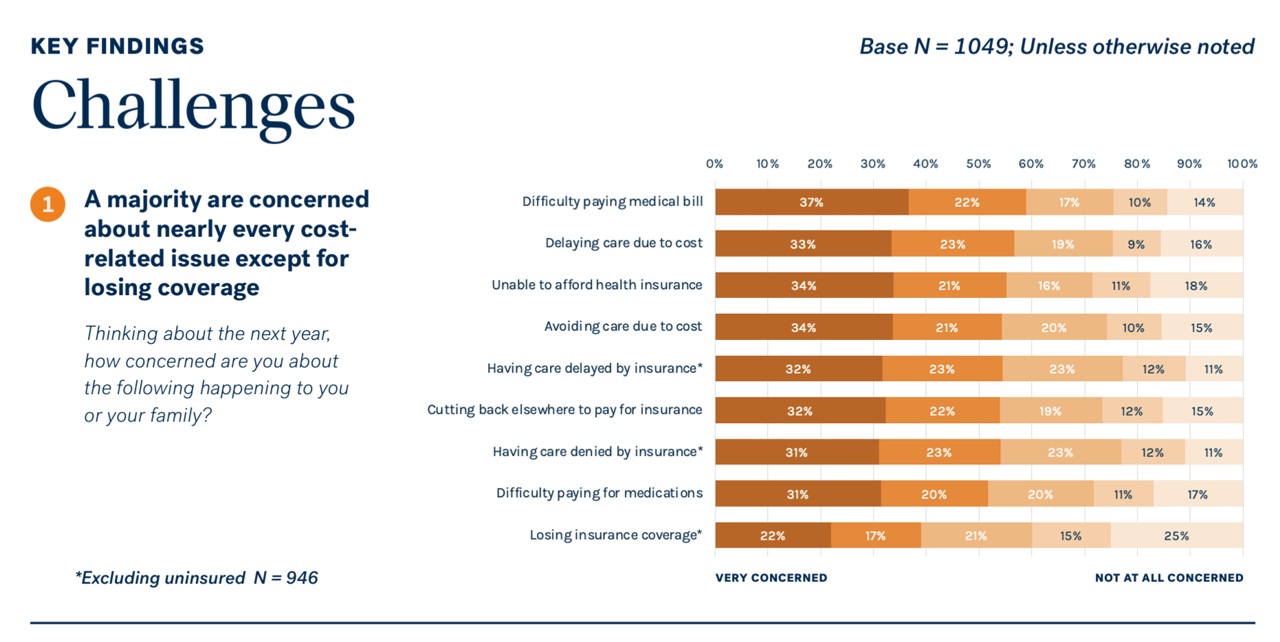
Most people in the U.S. are concerned about many cost-related aspects of health care, we learn from Jarrard’s 2026 survey report on Americans’ health care financial angst titled Navigating the Riptide: Public views on healthcare, health policy, and healthcare organizations. Jarrard fielded the consumer study among 1,049 U.S. adults 18 years of age and older in early January 2026. Here are the details, listing nine cost-related issues U.S. consumers face in their health care journeys – including, Difficulty paying medical bills (net 59% very or somewhat concerned) Delaying medical care due to cost (55%) Inability
Health Care Ads at the Big Game (Super Bowl LX) – Edgy, Entertaining, Educational

“When Weight Watchers dared to run an ad in 2015, it was likened to a record scratch,” AdAge noted in its preview of ads planned for broadcasting during Super Bowl LX. A decade+ later, healthcare and health-related promotions are part of the Big Game’s financial lifeblood, where a 30-second spot can cost $8 million according to AdMeter And on the aesthetics/design front, some of the ads this year are downright edgy — entertainment-intended, but also educational in their own way. Take “Rich People Live Longer,” this year’s ad from Hims & Hers Health. The company advertised at last year’s game
When a Hotel Becomes Your Health Partner – Learning from Novotel and Accor

“Novotel Launches ‘Longevity Everyday.'” That’s the title of the global, France-based hotel chain’s press release, announcing the Novotel brand’s initiative to serve up healthy hospitality. Check out this video… Behind this strategic positioning decision, the hotel notes, “Accor data reveals that one in three travelers is taking daily steps to improve their mental and physical wellbeing, yet most longevity programs remain out of reach for many people. This gap between demand and accessibility has created a strategic opportunity that Novotel, Accor’s founding brand, is uniquely positioned to address.” This approach will extend to over 600 hotels operating in 67 countries
The New (Old) Long-Term Care: Intergenerational, Together at Home

One in three adult children in the U.S. say that moving their parent(s) into their family’s home is the most likely living arrangement for their folks as they age, we hear from a study on the “Care Conversation” from LevLane, conducted by Talker Research. That’s twice as many consumers as those looking to assisted living (19%) or senior living or memory care facilities (16%). Talker Research conducted a survey of 2,000 U.S. adults, Gen X or younger with a living parent, to assess the current state of and future prospects for the senior living market.
The Healthcare Affordability Elections, 2026 and 2028 – Listening to the KFF Tracking Poll, January 2026
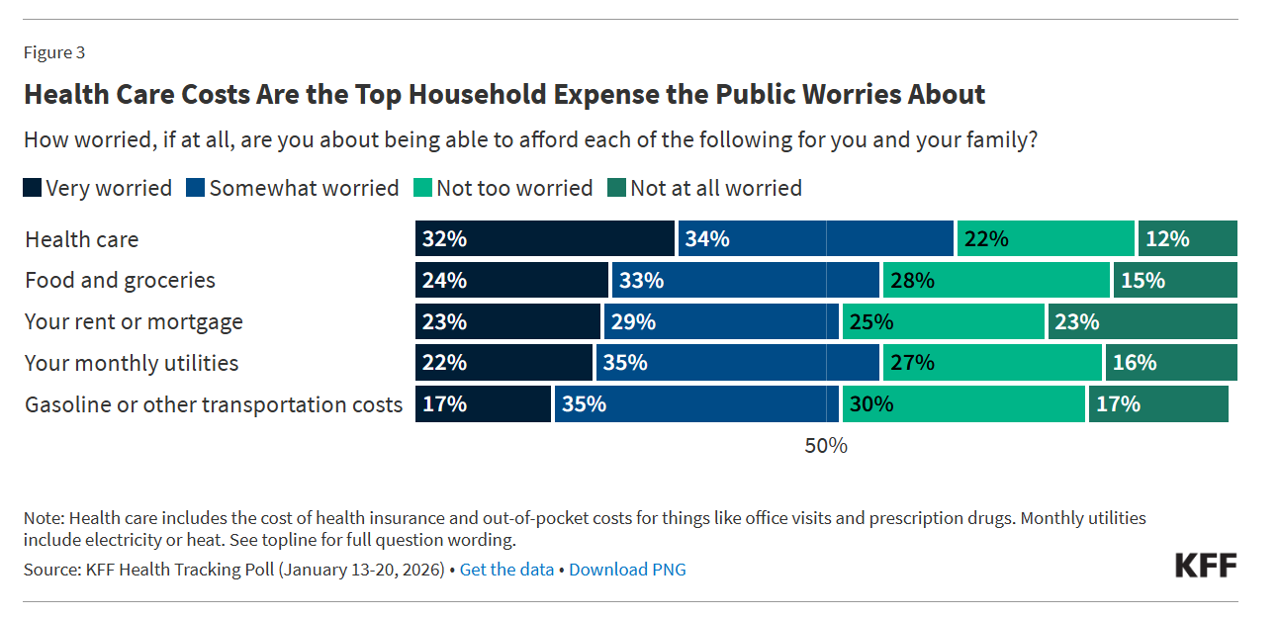
The title of KFF’s press release launching the Foundation’s January 2026 Health Tracking Poll clearly observes, “Health Care Costs Tops the Public’s Economic Worries as the Runup to the Midterms Begins.” I’ve pulled out the key details to share my lens on the 2026 midterm and 2028 Presidential election forecast, which I believe will turn out to be (in part) The Patients’ Elections. Here’s the top-line title finding — where most people in the U.S. — 2 in 3 people (66%) — are worried more about health care costs compared with other major household expenses.
Optimistic and Skeptical: How Older Americans Are Using and Seeing AI – the View from AARP
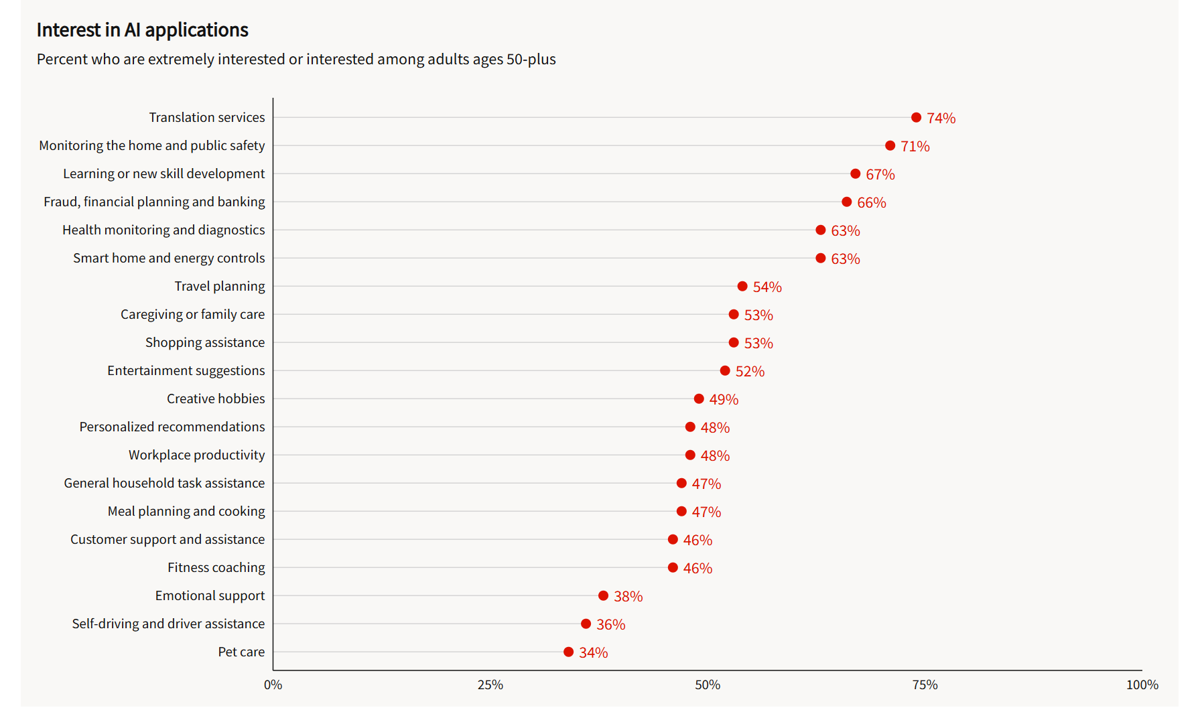
People over 50 in America typically hold two thoughts in mind at once when it comes to AI: they’re optimistic and skeptical, depending on the “job” that AI could do, according to research from AARP explained in the report, Navigating the World of AI: Awareness, Attitudes, and How People Expect to Use It. Topline, most people 50 and over have used AI in some way, with roughly 3 in 5 older Americans saying “I am a beginner” in using AI across age groups from 50 to 70+. Most older Americans are familiar with many terms in the
As Adult Vaccination Levels Fall, We Must Assert the Value of Vaccines
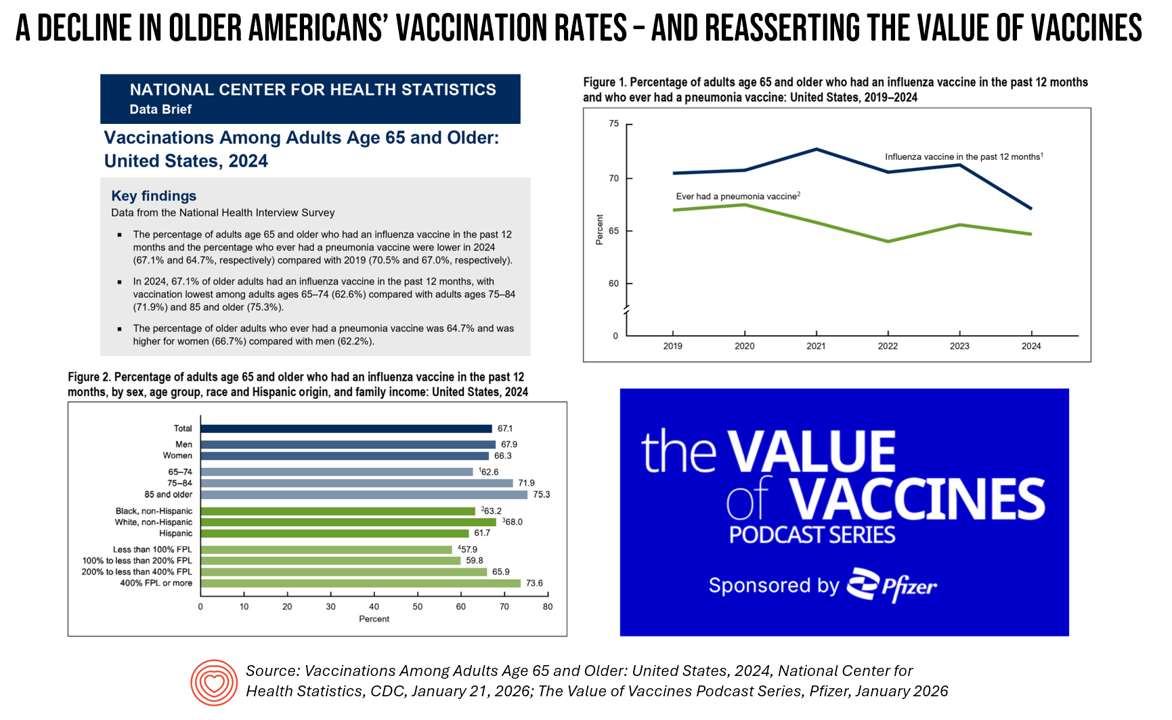
The rate of vaccinations among people 65 years of age and older has declined since 2019 — a personal health challenge for aging Americans and their caregivers and families, and a public health problem for the U.S. The Centers for Disease Control’s National Center for Health Statistics published Data Brief 547 on the situation on January 21, 2026. In the meantime, serendipity and timing are uncanny in the moment as The Value of Vaccines conversation series from Pfizer was launched this week. I am grateful to have participated in this project with several sisters-in-expertise: Elif Alyanak from Avalere, Venesa Day
Distrust is the default, insularity is our mindset: The Edelman Trust Barometer in 2026
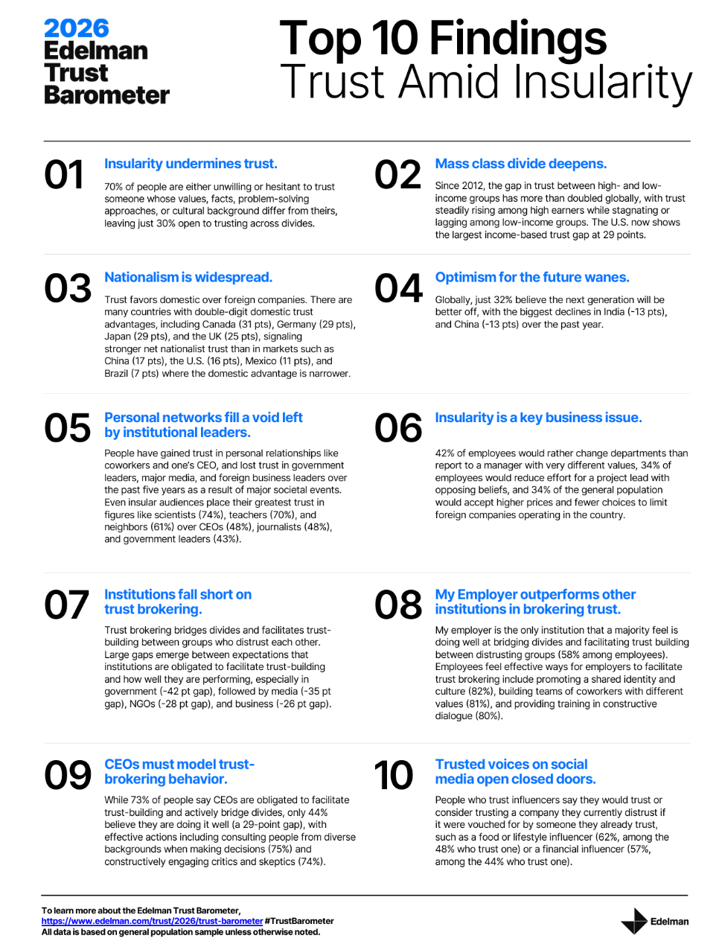
ss Last year’s “shared reality” was a culture of trust and a crisis of grievance: this year, it’s trust and insularity, we learn from the Edelman Trust Barometer for 2026, launched this week during the World Economic Forum in Davos, Switzerland. Here are the Top 10 findings from the annual study, which Edelman conducted among nearly 34,000 citizens in 28 countries in October and November 2025: Insularity undermines trust The mass class divide deepens Nationalism is widespread Optimism for the future wanes Personal networks fill a void left by
In the U.S., Belief and Trust in Science and Scientists is Tied to Political Party and Education

Most Americans believe it’s very important for the nation to lead in scientific achievements. But twice as many Democrats as Republications, 65% versus 32%, say the U.S. is losing ground in science innovations. The Pew Research Center asks and answers the Do Americans Think the Country Is Losing or Gaining Ground in Science? And the answer is, “millions of people do think so.” The Pew team polled 5,111 U.S. adults in late October 2025 for this research. There are a few political chasms related to science-trust in the U.S. that are important
Thinking About Dr. Martin Luther King and Health Citizenship in 2026
Today as we appreciate the legacy of Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would deliver two months later in Washington, DC. Wisdom from the speech: “But now more than ever before, America is forced to grapple with this problem, for the shape of the world today does not afford us the luxury of an anemic democracy. The price that this nation must pay for the continued oppression and exploitation of the
Why Progresso Soup was at CES 2026: How Food is Playing Into the Evolving Health Consumer and Retail Health Landscape
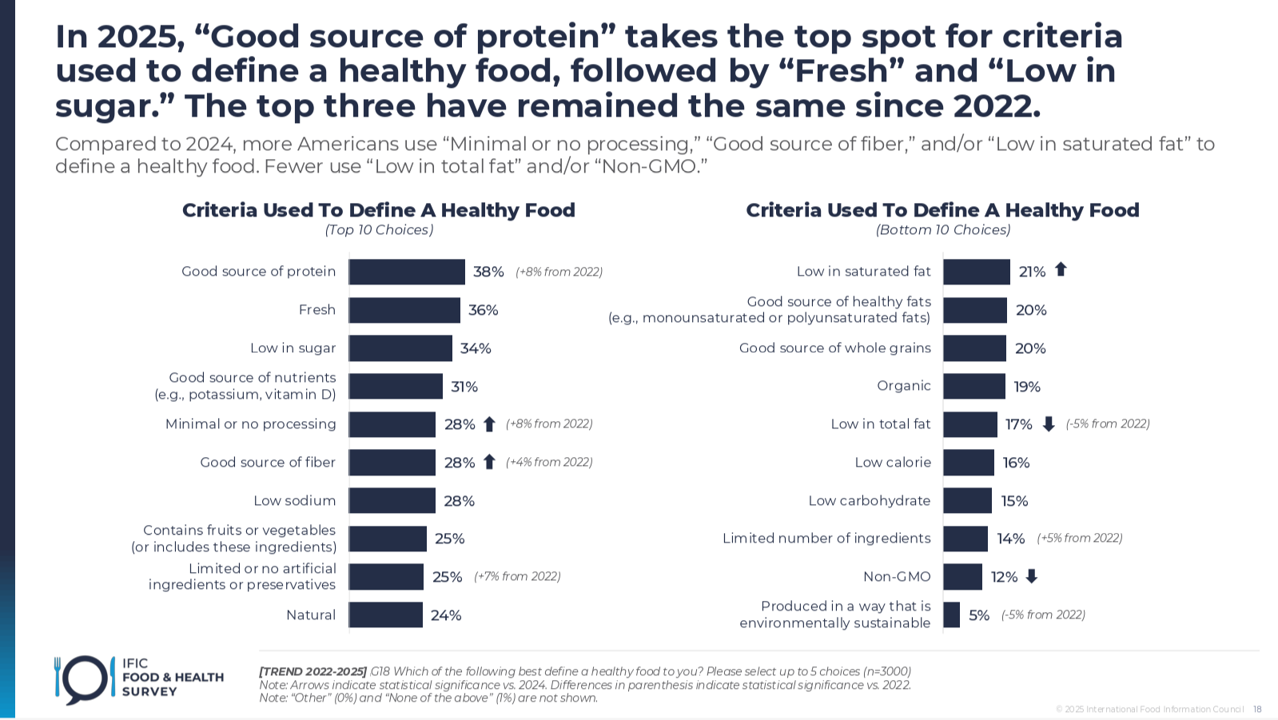
Why was Progresso Soup and its manufacturer General Mills at CES 2026? Specifically, in the AgeTech Collaborative curated by AARP? If you are part of the health/care ecosystem in any of its segments, chances are you’re attending conferences at the start of 2026 or soon to attend one. I spent last week at CES 2926 in Las Vegas getting updates on digital health, well-being, and self-care innovations. This week, hundreds of my colleagues are attending #JPM2026, the 44th annual J.P. Morgan Healthcare Conference held in San Francisco every year at this time. One conference that would not have been well-attended
While Nurses Continue to Rank Top in Honesty and Ethics, Americans’ Respect for All Professions is Tanking

While nurses continue to rank high for honesty and ethics, Americans’ trust in the nations’ professions is tanking, found in this year’s Gallup Poll update titled, Nurses Continue to Lead in Honesty and Ethics Ratings. Nurses perennially top this chart, usually followed by doctors and pharmacists. But this year, it’s military veterans who garner the second spot in the Gallup Poll, with doctors and pharmacists in positions 3 and 4. Ranking at the bottom as least-respected for honesty and ethics are Members of Congress, again garnering the low-point in this study, with telemarketers trailing the
Aging is Not a Decline, but an Awakening at CES 2026 – Learning from AARP About Consumers, Lifespan, and Technology
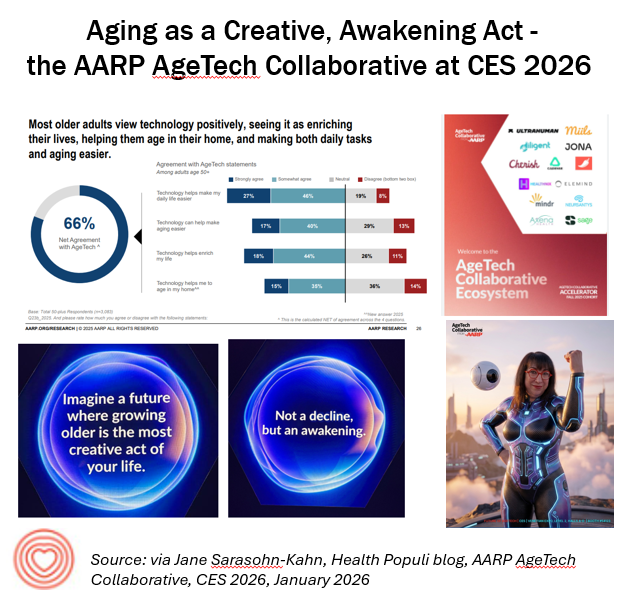
Aging and longevity are key themes driving technology innovations and markets, and walking the miles of aisles of CES 2026 demonstrates the expanding landscape of the role of tech in healthy living across the lifespan. I spent time at the AARP AgeTech Collaborative space this week as I did last year (here was my write-up of AARP and CES 2025 for historical context). In experiencing this year’s portfolio of AgeTech collab partners, from start-ups to Fortune 100 companies in the mix, was informative, inspiring, and even energizing as someone who has been a member of AARP since turning 50 some
Sleep as a Pillar of Health at CES 2026 — What Can Happen When A Lamborghini Legacy Mashes Up With Sleep Tech
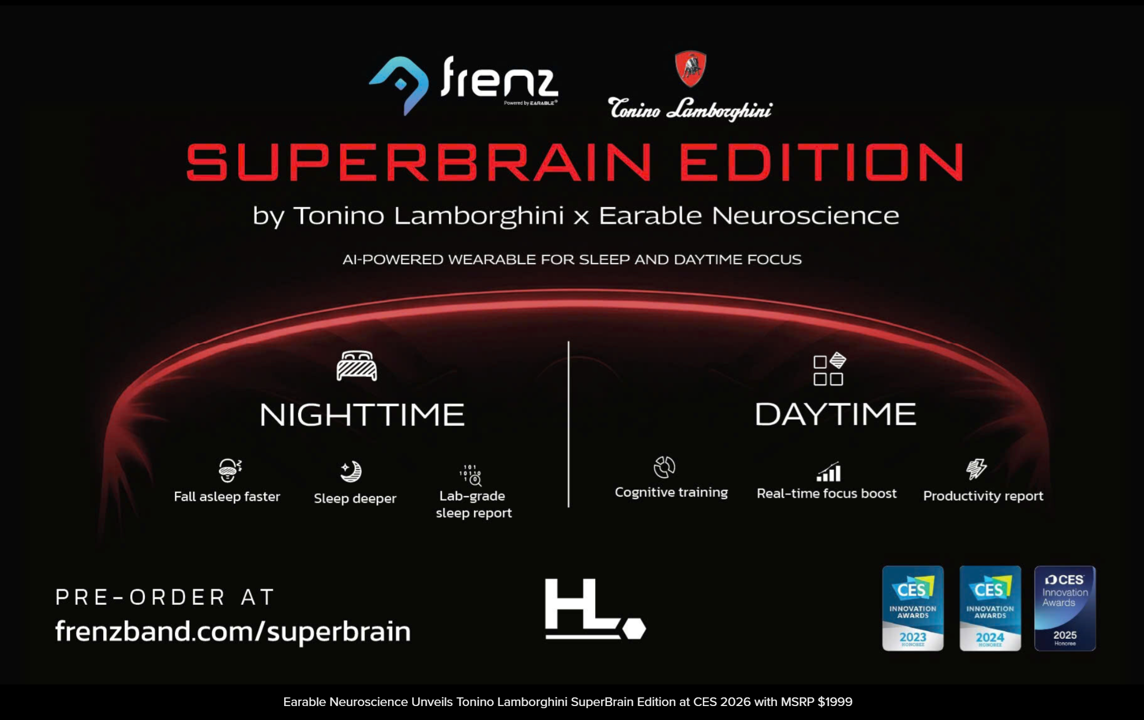
Well-being is a new form of luxury….and sleep is an inherent aspect of well-being and health, a message reinforced during a press conference hosted by the National Sleep Foundation at CES 2026. Sleep has been an ongoing theme at CES for many years: here’s a post I wrote on sleep at CES 2025 a year ago for some historical context. In today’s growing home-as-our-health-hub ethos, sleep-tech takes on a variety of forms, from new-fangled beds and sensors, smart rings, other wearable tech (like earbuds), and circadian rhythm lighting innovations. In yesterday’s Health Populi, I focused
The Bathroom’s Role in the Home as Health Hub: Catching Up with Kohler Health’s CEO at CES 2026

A key Tech Trend to Watch at CES 2026 is consumers’ re-imagining and fitting out their homes as sites for bolstering health and well-being. I’ve been tracking this concept as far back as 2011 when I wrote this post from the 2011 Consumer Electronics Show. A decade-and-a-half later, in déjà vu spirit, the concept is no longer theoretical or futures-thinking. Fast forward from 2011 to the COVID-19 pandemic, when everyone’s home spaces became re-purposed for health, for medical care, for well-being, for fitness and exercise, for cooking up nutritious food, for
Tech Trends to Watch at CES 2026 – For Health, It’s About Longer Living, Smarter Living, and Better Living
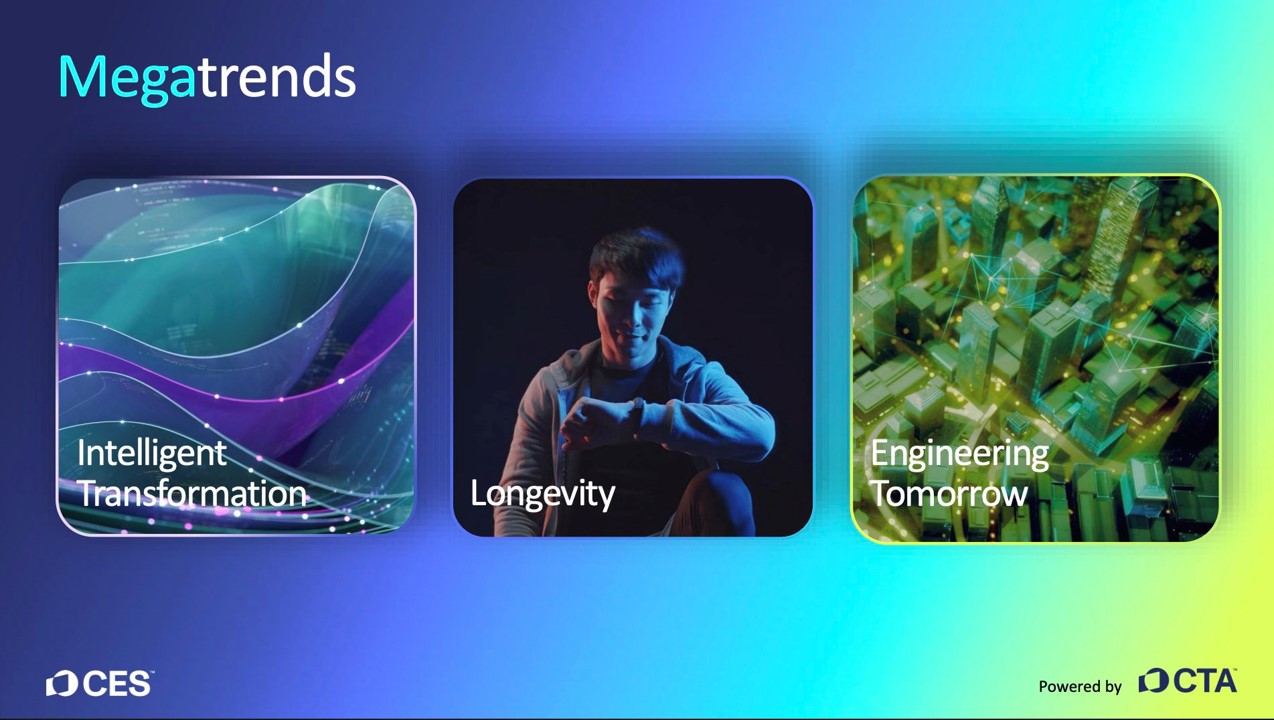
Live from CES 2026 in Las Vegas…the first day of CES Media Days preceding the big show always covers a context-setting report on Tech Trends to Watch. This is one of my annual go-to programs which helps orient media and industry analysts with a lens on CES’s key tech categories and some hard data on market size and growth expectations. While I’ll focus on the health/care specifics in the trend forecast, let me first update you on the overall technology market revenues for the U.S. which are estimated at $565 billion for 2026.
Health Tracking Wrapped Around Your Finger: All About Wearable Tech’s Growing Smart Rings Category at CES 2026
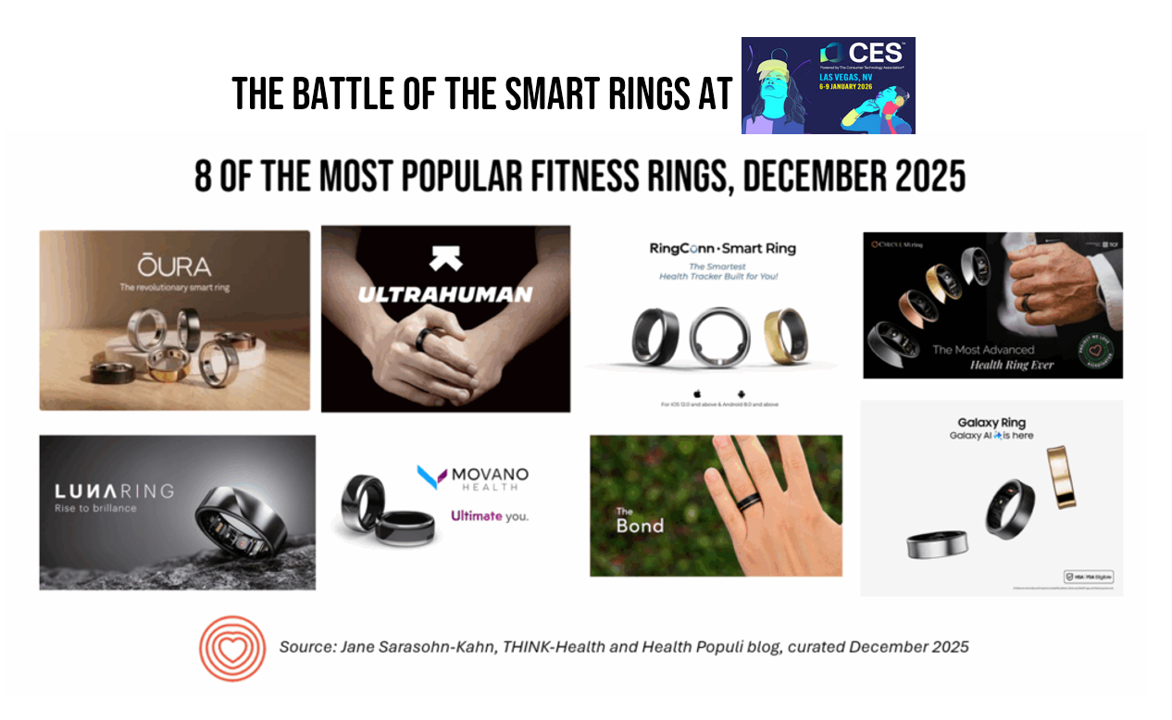
For well over a decade, wearable technologies have been developed for humans from head-to-toe — from forehead-worn bands to address stress and headaches to smart shoes with sensor-embedded soles that assess our gait and posture. In 2013, my CES coverage had a focus on “The Battle of the (Wrist)Bands.” This year, the #wearabletech category feels like a fierce competition for the human real estate of the finger — that is, a battle of the smart rings. Twelve years later, smartwatches are mainstream trackers for health embedded with sensors that are gaining clinical evidence for use in medical care well beyond





 I'm grateful to be part of the Duke Corporate Education faculty, sharing perspectives on the future of health care with health and life science companies. Once again, I'll be brainstorming the future of health care with a cohort of executives working in a global pharmaceutical company.
I'm grateful to be part of the Duke Corporate Education faculty, sharing perspectives on the future of health care with health and life science companies. Once again, I'll be brainstorming the future of health care with a cohort of executives working in a global pharmaceutical company. Thank you
Thank you  Jane joined host Dr. Geeta "Dr. G" Nayyar and colleagues to brainstorm the value of vaccines for public and individual health in this challenging environment for health literacy, health politics, and health citizen grievance.
Jane joined host Dr. Geeta "Dr. G" Nayyar and colleagues to brainstorm the value of vaccines for public and individual health in this challenging environment for health literacy, health politics, and health citizen grievance.