How AI is Shaping the Patient and Clinician Experience – My Conversation with Microsoft
For change agents in health care, one of our True North paradigms is the Quintuple Aim. The five pillars of the Quint Aim grew from 3 goals of the Triple Aim: to improve patient experience, to drive better health outcomes, and to lower per patient costs. The Quadruple Aim added the goal of bolstering clinicians’ well-being (to address burnout, stress and depression), leading to the addition of health equity as the fifth objective. That happened in 2021, in the height of the COVID-19 pandemic which shined a bright light on health disparities, inequities, and risks in peoples’ social determinants of
From Evolution to Innovation, from Health Care to Health: How Health Plans With Collaborators Are Re-Defining the Industry
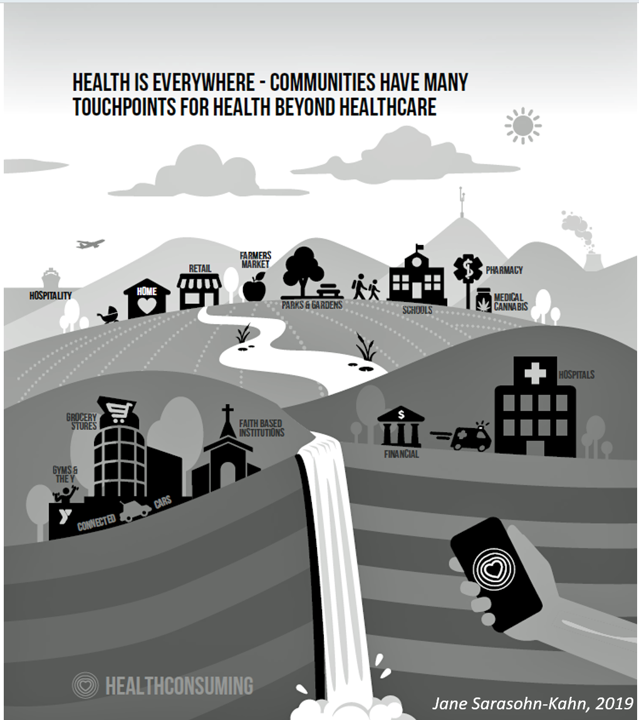
As a constant observer and advisor across the health/care ecosystem, for me the concept of a “health plan” in the U.S. is getting fuzzier by the day. Furthermore, health plan members now see themselves as medical bill payers, seeking value and consumer-level services for their health insurance premium investment. Weaving these ideas together is my mission in preparing a session to deliver at the upcoming AHIP 2024 conference in June, I’m thinking a lot about the evolving nature of health insurance, plans, and the organizations that provide them. To help me define first principles, I turned to the American father
Physicians Feeling Burnout and Depression Continues in 2024 — The Annual View From Medscape
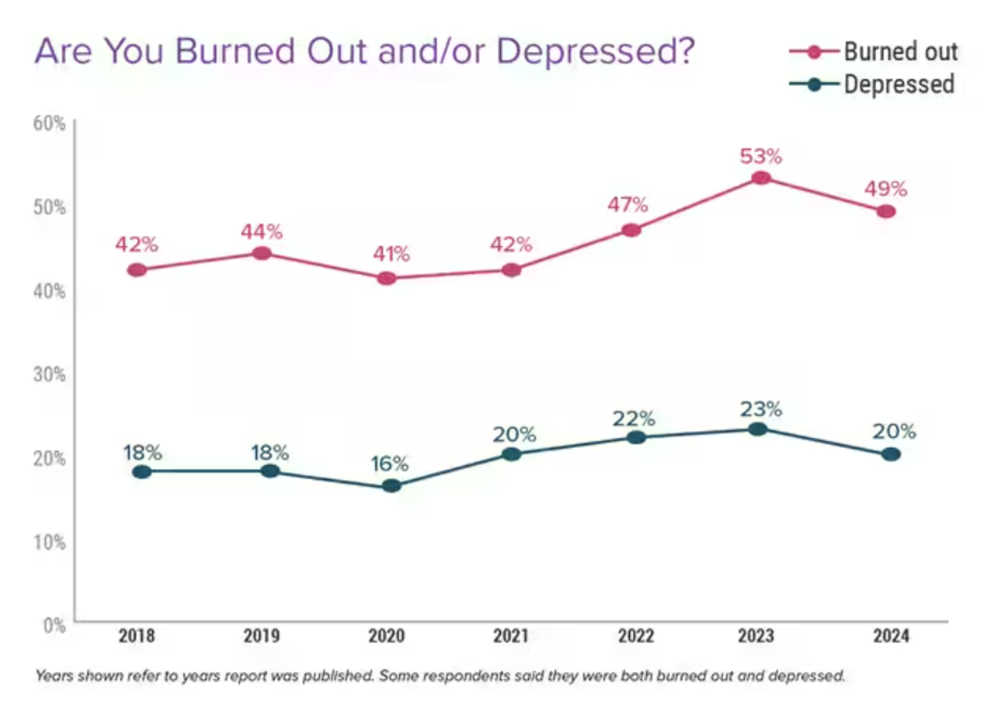
One-half of U.S. physicians report feeling burned out, and 3 in 5 of those doctors say they have felt burned out for over two years, according to the Physician Burnout & Depression Report for 2024 from Medscape. While the study’s press release asserts there may be “progress” given the percent of doctors citing burnout fell by 4 percentage points from 53% of doctors in 2022 to 49% in 2023, it is obvious the U.S. physicians need greater support and less taboo concerning their mental health which impacts both their professional and personal lives.
Ethics for AI in Health – A View From The World Health Organization
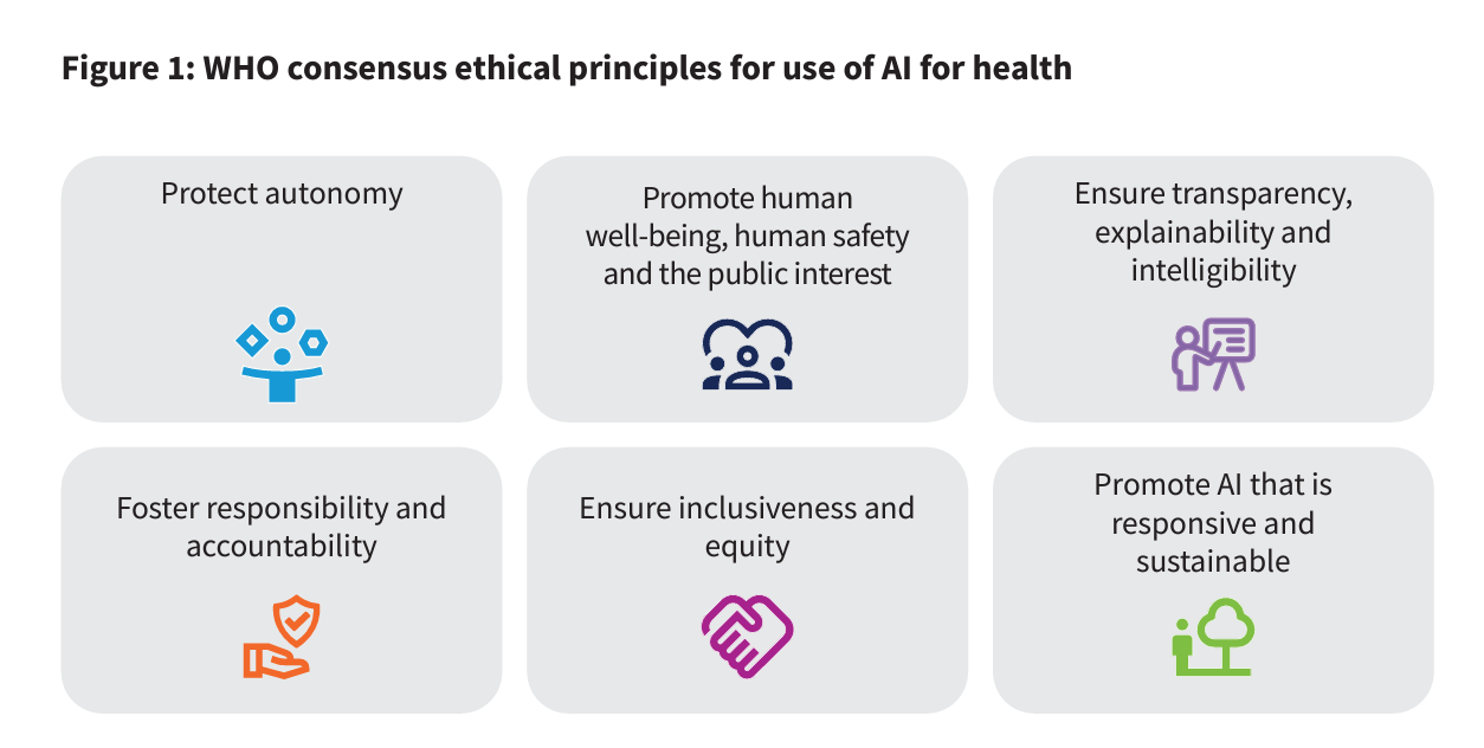
For health care, AI can benefit diagnosis and clinical care, address paperwork and bureaucratic duplication and waste, accelerate scientific research, and personalize health care direct-to-patients and -caregivers. On the downside, risks of AI in health care can involve incomplete or false diagnoses, inaccuracies and errors in cleaning up paperwork, exacerbate differential access to scientific knowledge, and exacerbate health disparities, explained in the World Health Organization’s (WHO) report, Ethics and governance of artificial intelligence for health. WHO has released guidance on the use of large multi-modal models (LMMs) in health care which detail 40+ recommendations for
Nurses Continue to Rank Highest in Ethics and Honesty for Professions in the US — But Peoples’ Opinions for All Jobs, Including Nursing, Have Eroded in Gallup’s Latest Poll
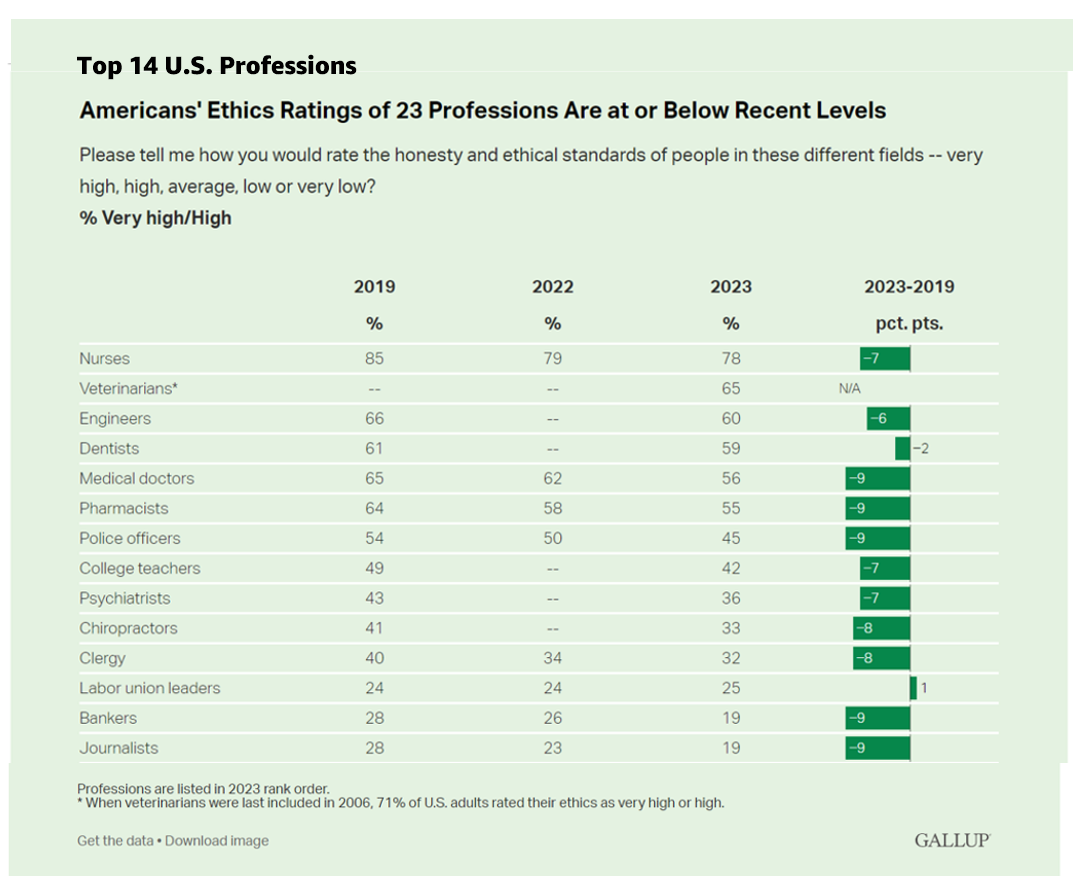
Ratings of honesty and ethics in professions have fallen down in the U.S., we find the Gallup Poll’s annual assessment of rankings for occupations that touch peoples’ lives in America. Each year for over a decade, nurses have ranked highest in this survey, representing the most-trusted profession working in America. However, even nurses’ ethic-equity has dropped in the hearts and minds of Americans over the past four years, falling 7 percentage points from a high of 85% of citizens ranking nurses at the greatest level of honesty and ethics to
Patients, Nurses and Doctors Blame Health Insurers for Increasing Costs and Barriers to Care
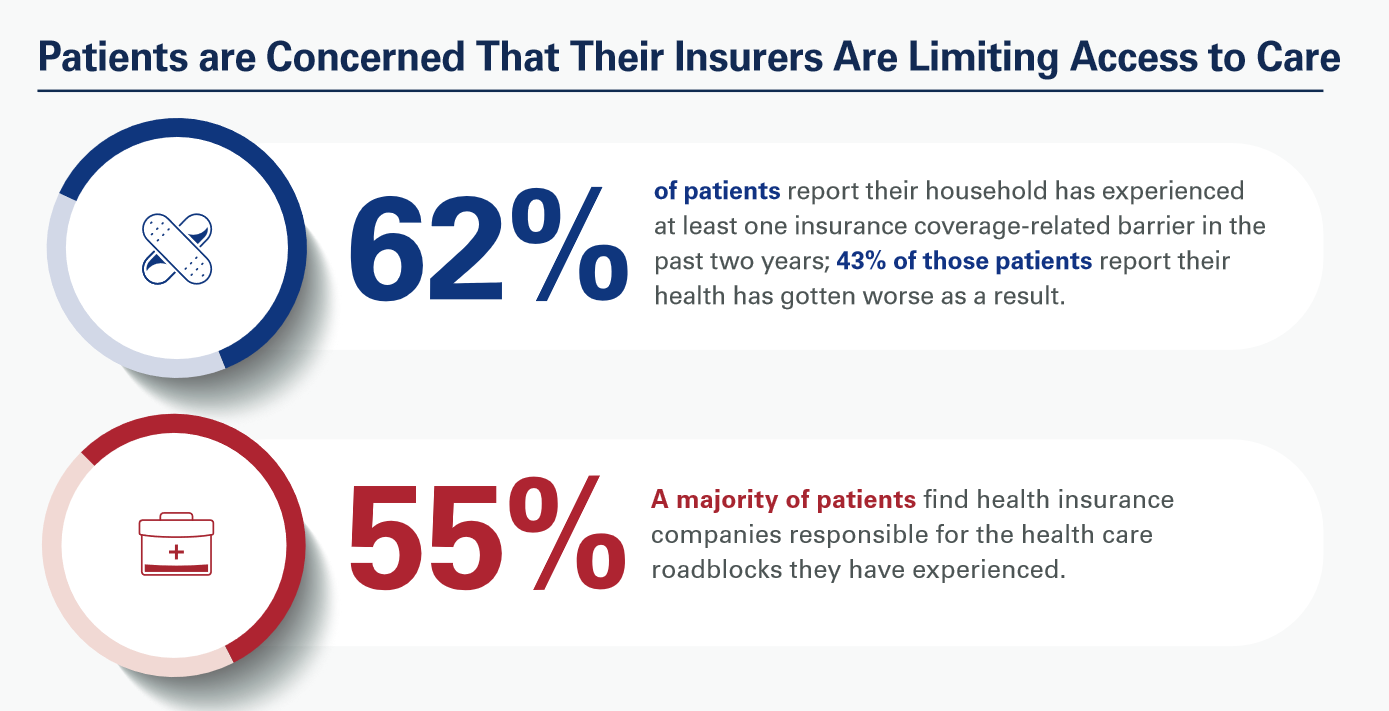
Most patients, nurses and doctors believe that health insurance plans reduce access to health care which contributes to clinician burnout and increases costs, based on three surveys conducted by Morning Consult for the American Hospital Association (AHA). Most patients have experienced at least one health insurance related barrier in the past two years, and 4 in 10 of those people said their health got worse as a result of that care-barrier. “These surveys bear out what we’ve heard for years — certain insurance companies’ policies and practices are reducing health care access and making





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.