While Virtual Care is “Table Stakes” in Health Care, Consumers Are Growing More Protective About Data-Sharing
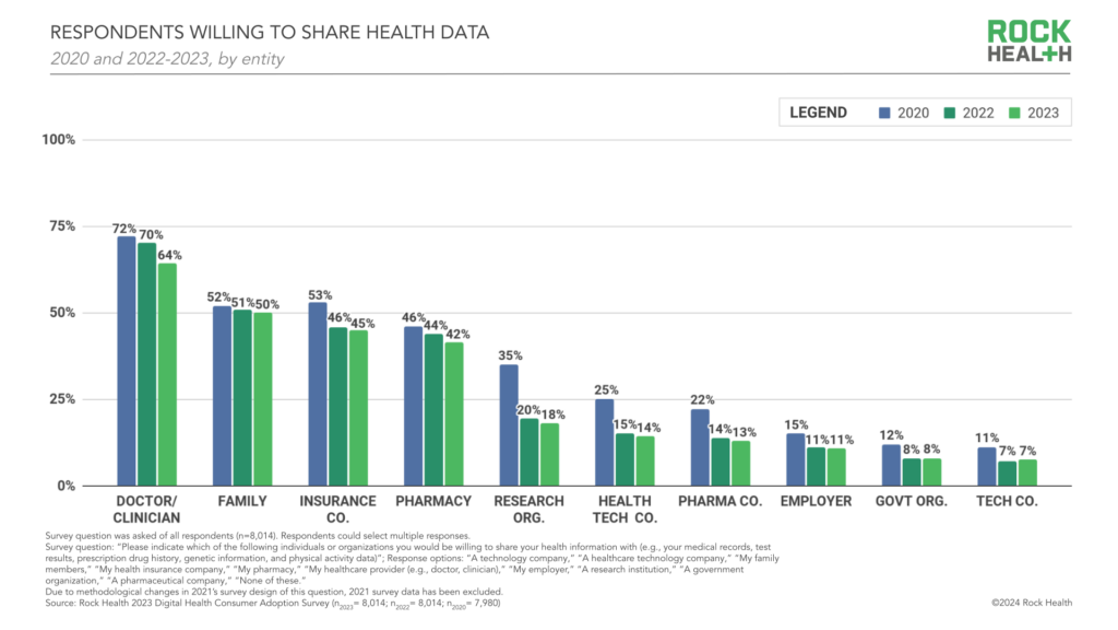
Three in four people in the U.S. have used virtual care, now, “Table-stakes…here to stay for patients and providers. However, that ubiquity comes with its own set of market pressures…shifting from pandemic-responsiveness to market- and consumer- responsiveness,” according to The new era of consumer engagement, Rock Health’s ninth annual Consumer Adoption Survey published 18 March. Convenience and waiting time are the top two reasons for choosing virtual over in-person care, Rock Health found. While virtual care is ubiquitous across the U.S. health care delivery landscape, patients-as-health care consumers are becoming more savvy and discriminating based
AI: Patients Included

“Clinical transformation with AI is easier without patients.” When Dr. Grace Cordovano heard this statement on a panel of physicians convening to share perspectives on the future of AI in health care held in early March 2024, the board-certified patient advocate felt, in her words, “insulted on behalf of the patient communities I know that are working tirelessly to advance AI that works for them.” “The healthcare ecosystem and policy landscape must formally recognize patients as end-users and co-creators of AI,” Cordovano wrote to me in an e-mail exchange. “Patients, their care partners, caregivers, and advocates are already utilizing AI
As Food-As-Medicine Gains Momentum, Watch for Dietitians and Pharmacists to Sit at The FaM Table – And A Lesson from George Washington Carver
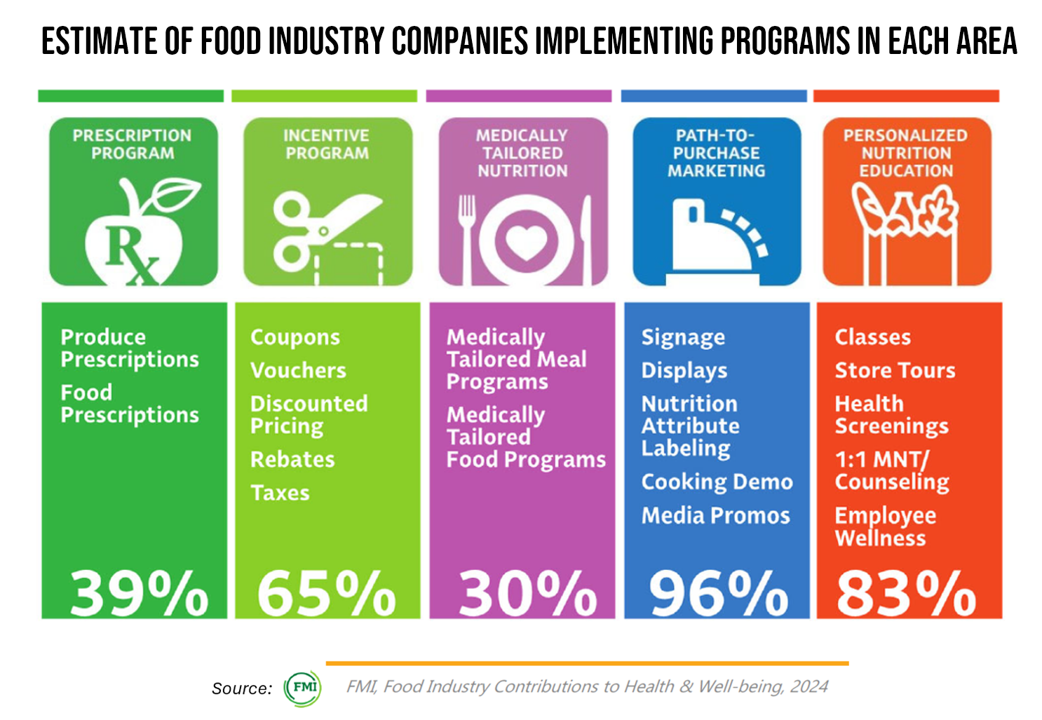
The food industry, both retail food chains and food suppliers, has found health and nutrition are having a positive impact on their businesses both for margins and for missions, we learn in the latest annual survey on Food Industry Contributions to Health & Well-being, 2024, from FMI. Most retail food channels operate pharmacies, three in five operate clinics in stores, and 2 in 5 of the clinics are health system-owned and operated. FMI, the Food Industry Association, conducted this industry poll in October 2023 among food retail and supplier members, totaling 36 organizations representing over
Rebel Health: The Personal and Professional Passion of Susannah Fox
A “rebel” is both a noun and a verb. As a noun, Merriam-Webster tells us that a rebel is a person who opposes or takes up arms against a government or a ruler. As a verb, “to rebel” is to oppose or disobey one in authority or control, or otherwise renounce and resist by force the authority of one’s government.” An additional definition of the verb is, “to feel or exhibit anger or revulsion.” If you’ve been a patient facing a diagnosis of an illness, whether rare or common, you may well have felt these various feelings stirring inside your self.
Ethics for AI in Health – A View From The World Health Organization
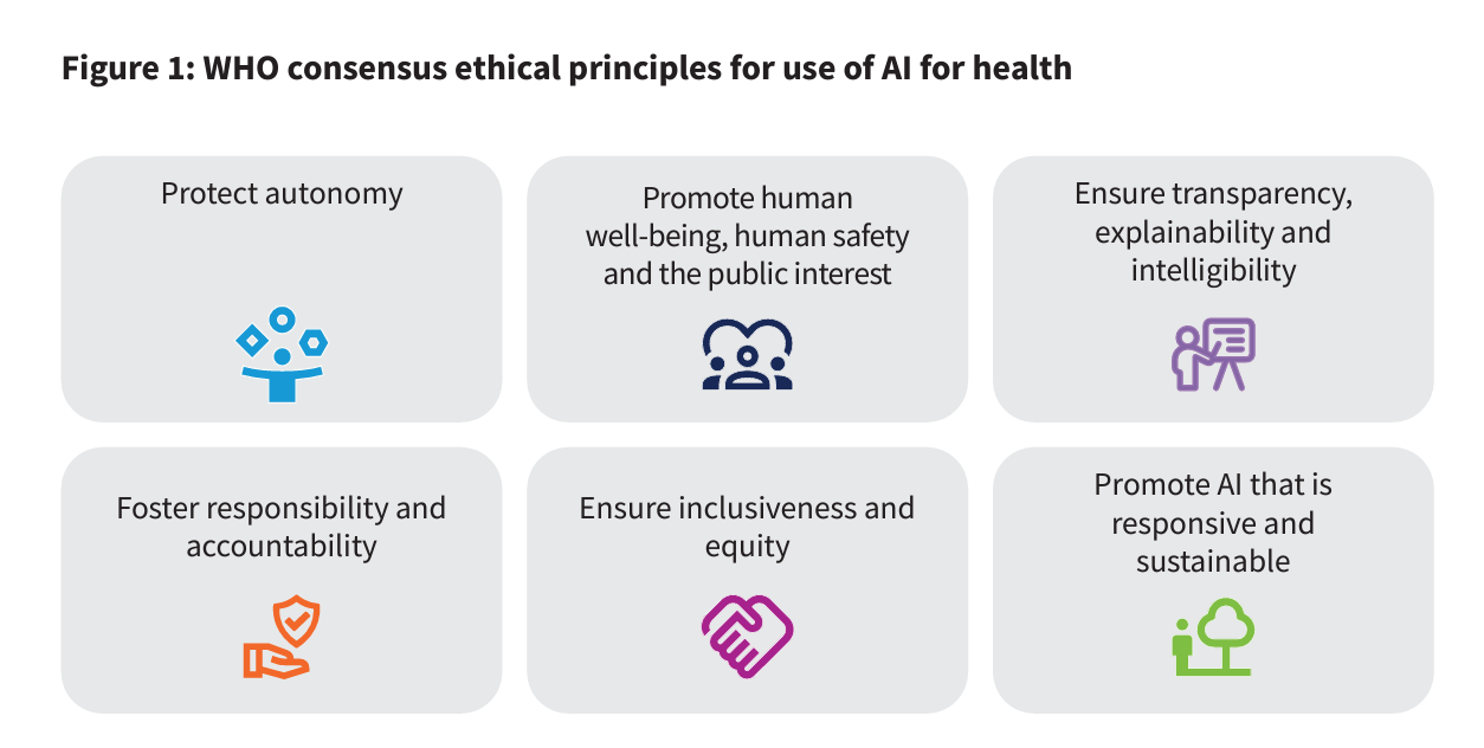
For health care, AI can benefit diagnosis and clinical care, address paperwork and bureaucratic duplication and waste, accelerate scientific research, and personalize health care direct-to-patients and -caregivers. On the downside, risks of AI in health care can involve incomplete or false diagnoses, inaccuracies and errors in cleaning up paperwork, exacerbate differential access to scientific knowledge, and exacerbate health disparities, explained in the World Health Organization’s (WHO) report, Ethics and governance of artificial intelligence for health. WHO has released guidance on the use of large multi-modal models (LMMs) in health care which detail 40+ recommendations for
Why Elevance Health is “Prescribing” Phones for Members
You’ve heard of food-as-medicine and exercise-as-medicine. Now we see the emergence of telecomms-as-medicine — or more specifically, a driver of health, access, and empowerment. Elevance Health, the health plan organization serving 117 million members, launched a program to channel mobile phones and data plans into the hands of some Medicaid plan enrollees, explained in the organization’s press release on the program. To implement this program and get connectivity into consumers’ hands and homes, Elevance Health is collaborating with several telecomms companies including Verizon, AT&T, Samsung, and T-Mobile. Funding is supported by the FCC’s Affordable Connectivity Program.
“Healthcare Isn’t Healthy:” the Global Challenge of Health Equity, and Calls-to-Action
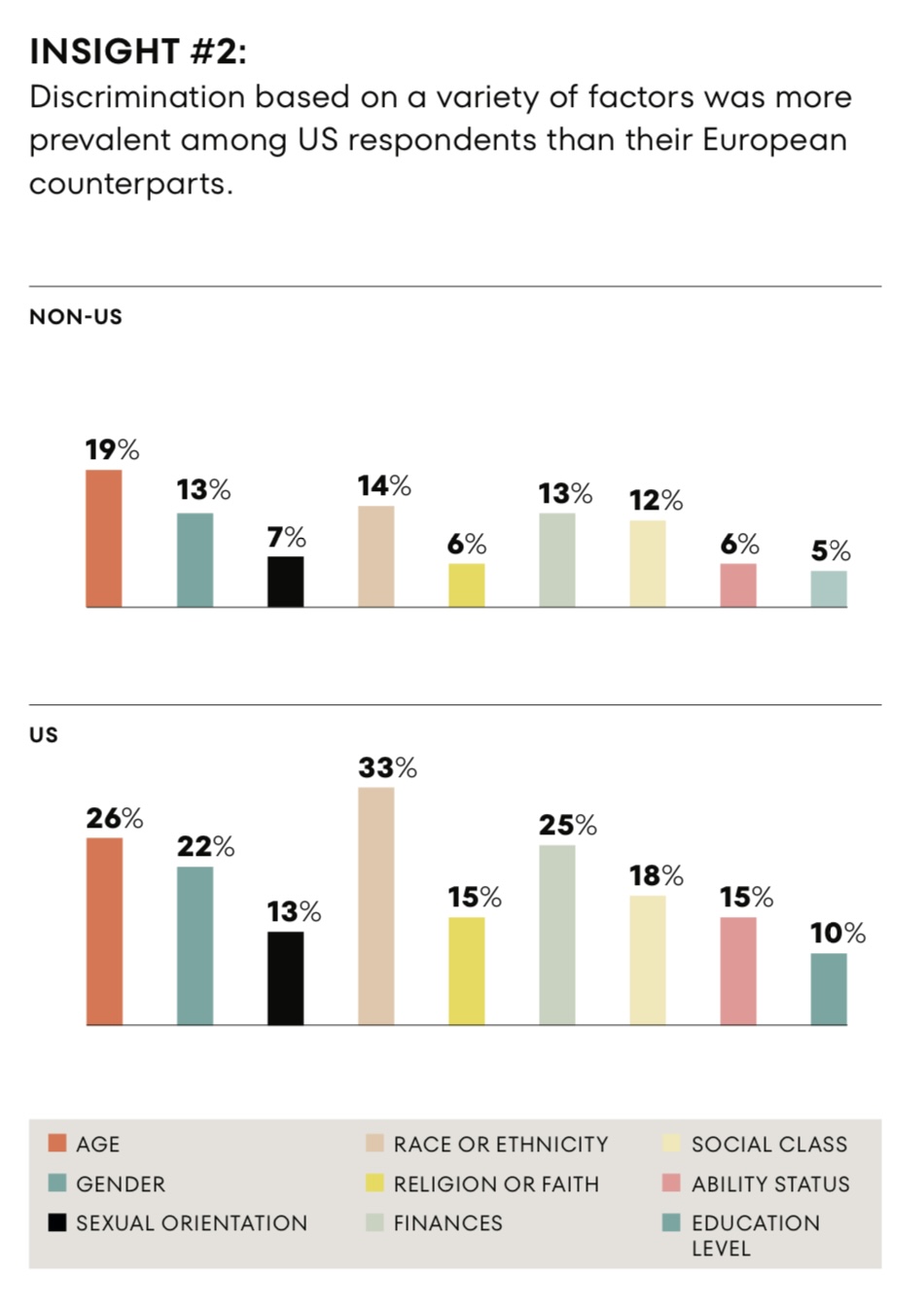
Discrimination in health care is reported by more people in the U.S. than in Germany, Spain, or the U.K., we learn in the research reported in The Intersection of Health Equity in Communities & Business Strategy: A Call-to-Action, from Omnicomm PR Group (OPRG) and Atlantic Insights. The study was conducted among 6,000 people living in Germany, Spain, the United Kingdom and the United States, fielding 1,500 interviews in each of the four countries in March 2023. The U.S. survey sample included 375 people identifying as Black, White, Hispanic, or
How Misinformation in Health Care Can Lead to Being “Dead Wrong” — KFF and Dr. G Connect the Dots
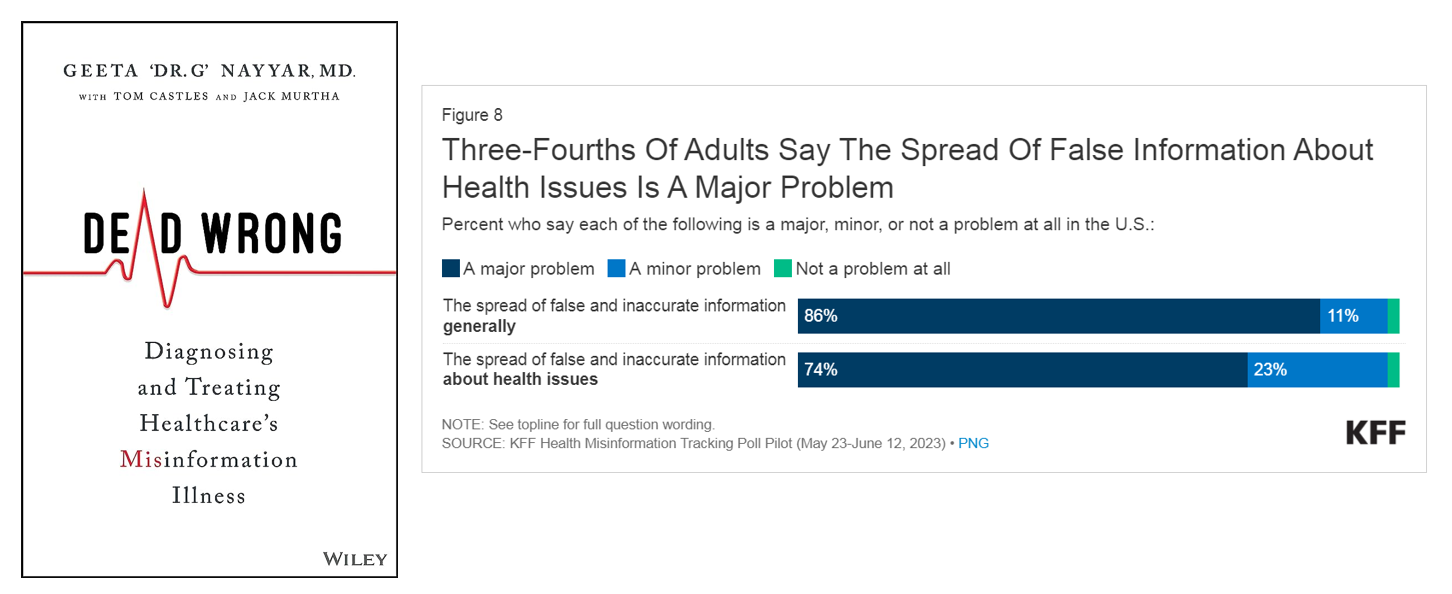
Three in four U.S. health citizens say the spread of false information about health issues is a major problem, found in Kaiser Family Foundation’s Health Misinformation Tracking Poll Pilot published earlier this month. KFF’s press release on the study summarized the top-line with, “Most Americans Encounter Health Misinformation, and Most Aren’t Sure Whether It’s True or False.” Explaining the implications of the broad reach of health misinformation in the U.S., Dr. Geeta Nayyar has written the book Dead Wrong: Diagnosing and Treating Healthcare’s Misinformation Illness, due out on October 17th and available now for pre-purchase
Barbie in Health Care – Joining the Barbie Zeitgeist
Barbie is having a moment, marketers agree. This weekend, many of us will buy movie tickets (yes, to see “real” movies in “real” brick-and-mortar cinemas) to see both the new film Oppenheimer along with the Barbie movie. So many movie-goers will be making it a double-feature experience that started as a meme, the portmanteau “Barbenheimer,” to mark the cultural-phenomenon moment. And the marketing frenzy accompanying the release of Greta Gerwig’s film has been an astonishing plethora of collaborations with consumer-goods companies and retailers. To join the pink-inspired fray, I’m featuring Barbie’s health care lives in
Patients-As-Health Care Payers Define What a Digital Front Door Looks Like
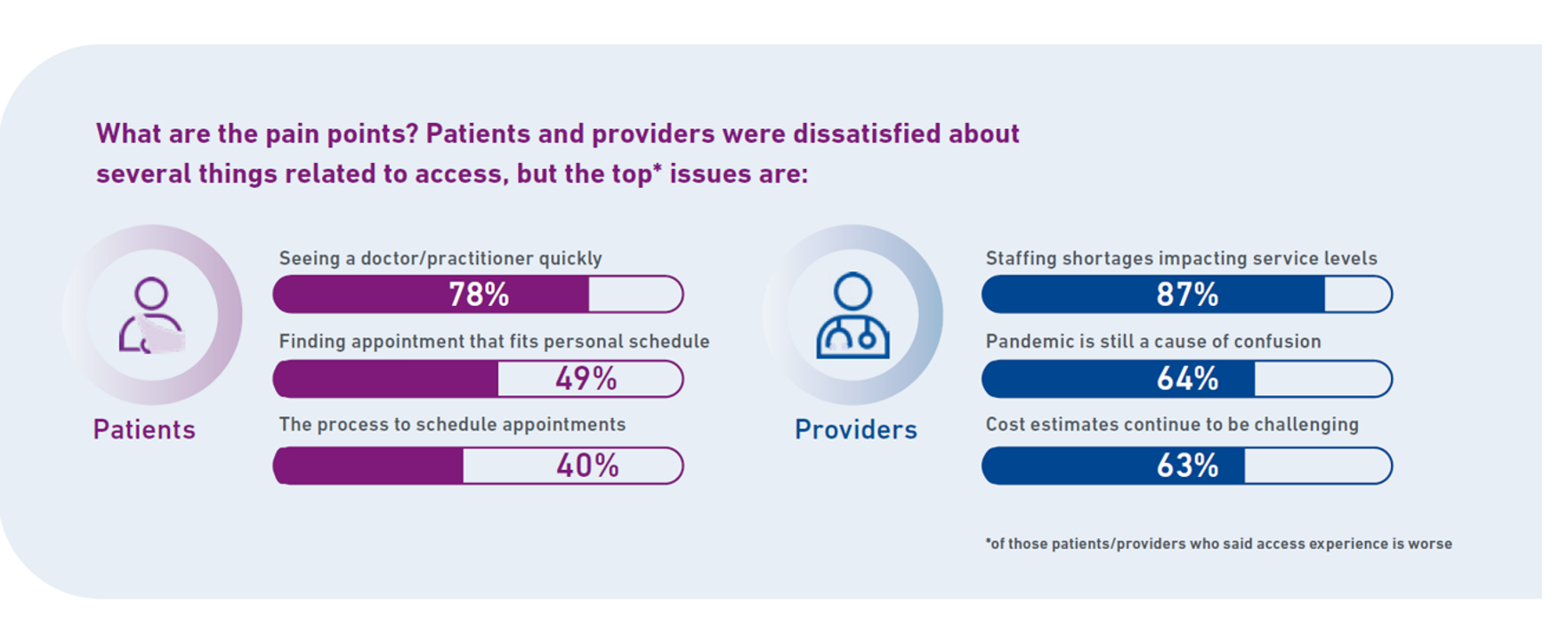
In health care, one of the “gifts” inspired by the coronavirus pandemic was the industry’s fast-pivot and adoption of digital health tools — especially telehealth and more generally the so-called “digital front doors” enabling patients to access medical services and personal work-flows for their care. Two years later, Experian provides a look into The State of Patient Access: 2023. You may know the name Experian as one of the largest credit rating agencies for consumer finance in the U.S. You may not know that the company has a significant footprint
Consumers and Cancer: 3 Patient-Focused Charts From IQVIA on the State of the Oncology in 2023 – and Introducing CancerX
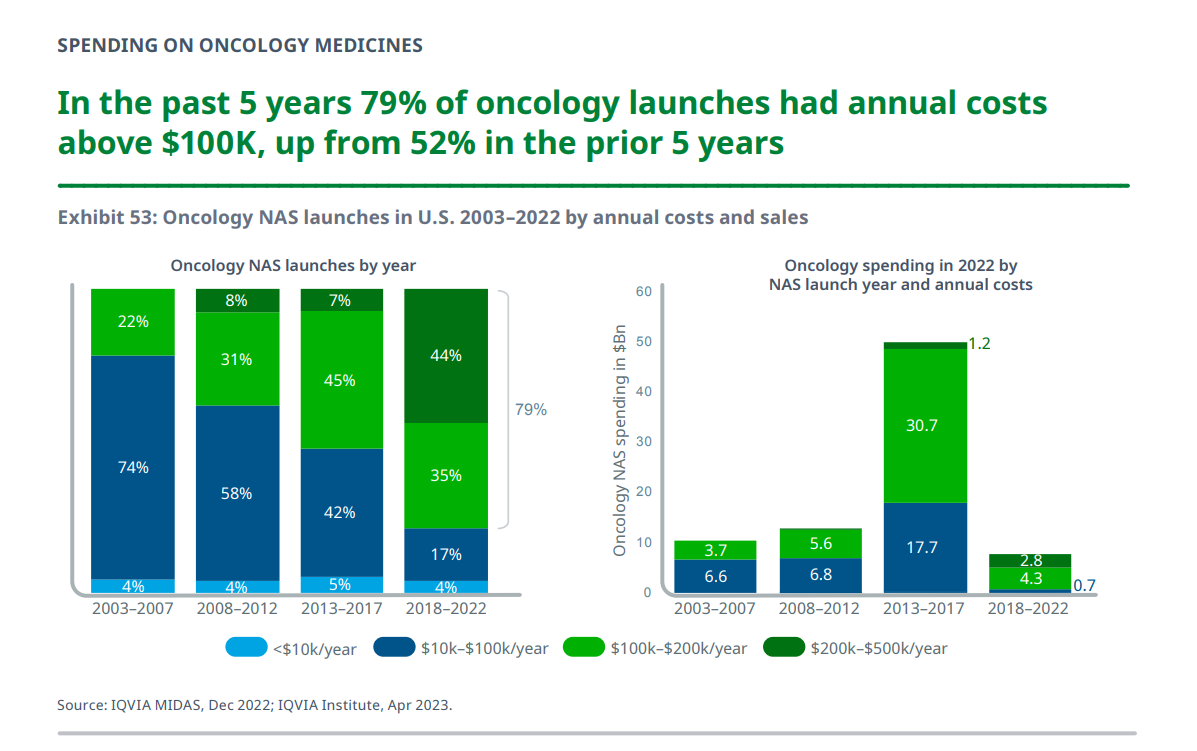
It’s time for the annual ASCO conference, currently convening the American Society for Clinical Oncology in Chicago. Starting 2nd June, there have been dozens of positive announcements updating research and therapies bringing hope to the 2 million new patients who will be diagnosed with cancer in the U.S. in 2023, and millions of more people worldwide. Just in time for #ASCO2023, the IQVIA Institute published their annual report on Global Oncology Trends 2023 – Outlook to 2027, an update featuring pipelines, therapy approvals, research updates, costs of oncology products, and patients.
Patients Have AI-Disconnect When it Comes to Their Health Care – Pew Research Center Insights
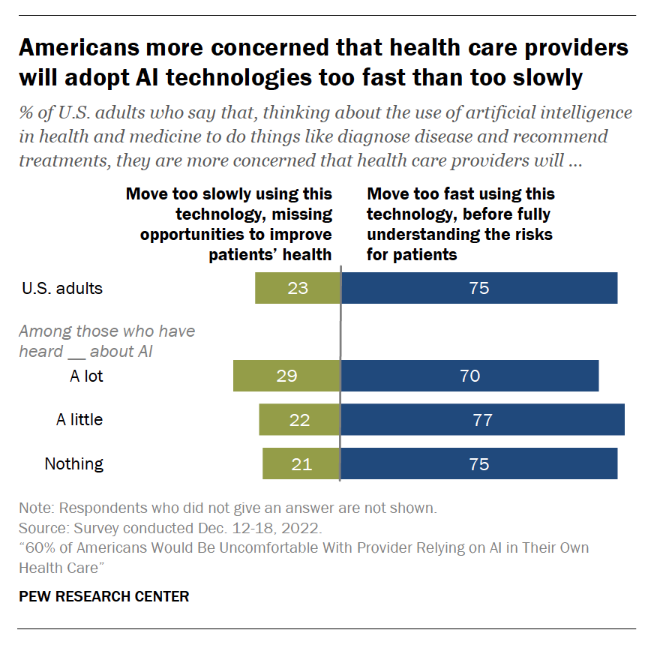
Most U.S. health citizens think AI is being adopted in American health care too quickly, feeling “significant discomfort…with the idea of AI being used in their own health care,” according to consumer studies from the Pew Research Center. The top-line is that 60% of Americans would be uncomfortable with [their health] provider relying on AI in their own care, found in a consumer poll fielded in December 2022 among over11,000 U.S. adults. Most consumers who are aware of common uses of AI know about wearable fitness trackers that can analyze exercise and sleep
Bayer at The Big Game LVII: the Heart Health Ecosystem is Ripe for Self-Care and DIY Health at Home

Joke if you must about Big Game cuisine being typically packed with calories and fat and carbs….and as such, not-so-great for health. For me, the ads are the attraction during The Big Game (along with the Philadelphia Eagles). In this year’s ad line-up, health will be featured in high-priced spots as it has for the past few years. Last year, I was intrigued by a female-focused 30-second spot from Hologic, educating viewers on cervical cancer, discussed here in Health Populi. This year, my eyes are on Bayer Aspirin’s campaign “encouraging sports fans to keep their heart
What Are Patients Looking for in a Doctor? It Depends on Who You Ask…and Their Race
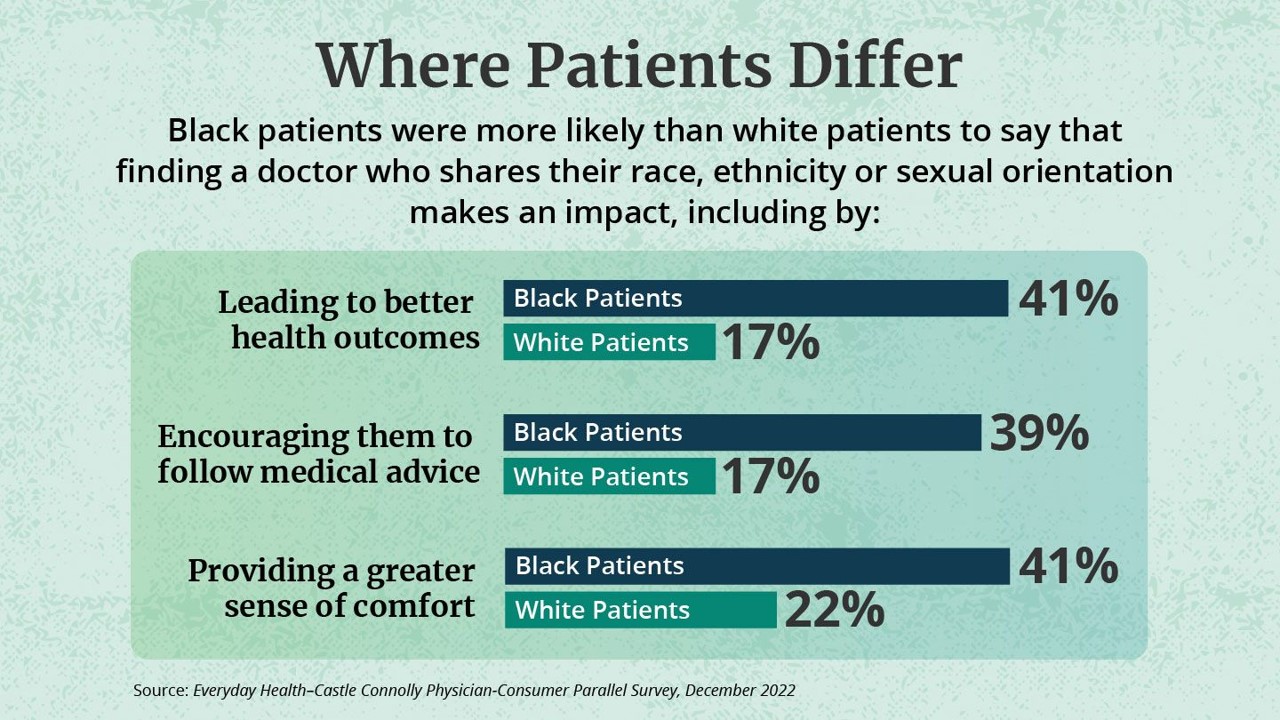
While the same proportion of Black and White patients say they are looking for a doctor with empathy and compassion, there are relatively large differences between patients based on their race, found in the Everyday Health-Castle Connolly Physician-Consumer study. The survey was conducted in December 2022 among a group of 1,001 U.S. consumers and 277 Castle Connolly health care professionals. As the first bar chart illustrates “where patients differ, “Black people were nearly twice as likely as white people (41 percent versus 22 percent) to completely agree that they would be more comfortable and
Of All Forms of Inequality, Injustice in Health Care is the Most Shocking and Inhumane: Listening to Martin Luther King, Jr.
Today as we appreciate the legacy of Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would deliver two months later in Washington, DC. Wisdom from the speech: “But now more than ever before, America is forced to grapple with this problem, for the shape of the world today does not afford us the luxury of an anemic democracy. The price that this nation must pay for the continued oppression and exploitation of the
The Heart Health Continuum at #CES2023 – From Prevention and Monitoring to Healthy Eating and Sleep
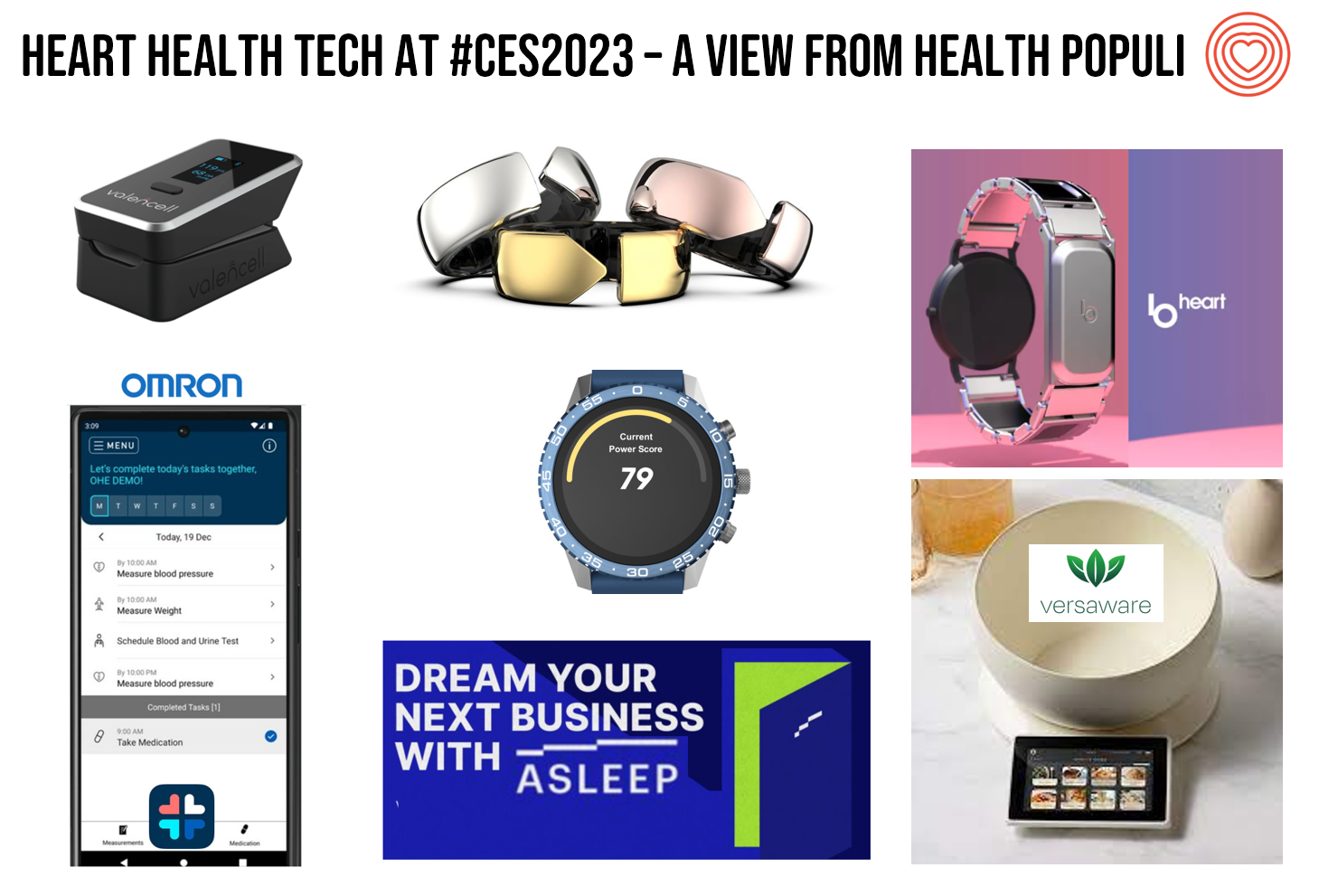
“Are we losing the battle against heart disease?” asks the lead article featured in the January 2023 issue of the AARP Bulletin. “Despite breathtaking medical advancements since President Harry Truman declared war on heart disease 75 years ago, researchers have observed a disturbing trend that started in 2009: America’s death rate from heart-related conditions is climbing again,” the detailed essay explains. AARP is in fact a very visible stakeholder in the 2023 CES, collaborating on the AgeTech content track at the tech conference. The track covers all aspects of aging well, from financial health to entertainment,
Can Consumer Electronics Help Stem the Decline of U.S. Life-Years? A Preface for #CES2023
Life expectancy in the U.S. dropped nearly three years between 2019 and 2021, from close to 79 years down to 76. We ended 2022 with this new, sobering statistic from the Centers tor Disease Control (CDC). We begin 2023 with the opening of CES 2023, the world’s largest annual meet-up of consumer electronics innovators, companies, and retailers. How can digital health and other consumer-facing technologies help our health? First, consider the stark data point(s), and then we can better respond to the question’s answer in the Hot Points, below. In case you
When Household Economics Blur with Health, Technology and Trust – Health Populi’s 2023 TrendCast
People are sick of being sick, the New York Times tells us. “Which virus is it?” the title of the article updating the winter 2022-23 sick-season asked. Entering 2023, U.S. health citizens face physical, financial, and mental health challenges of a syndemic, inflation, and stress – all of which will shape peoples’ demand side for health care and digital technology, and a supply side of providers challenged by tech-enabled organizations with design and data chops. Start with pandemic ennui The universal state of well-being among us mere humans is pandemic ennui: call it languishing (as opposed to flourishing), burnout, or
Black Panther: Wakanda Forever Inspires an NHS Blood Donor Campaign
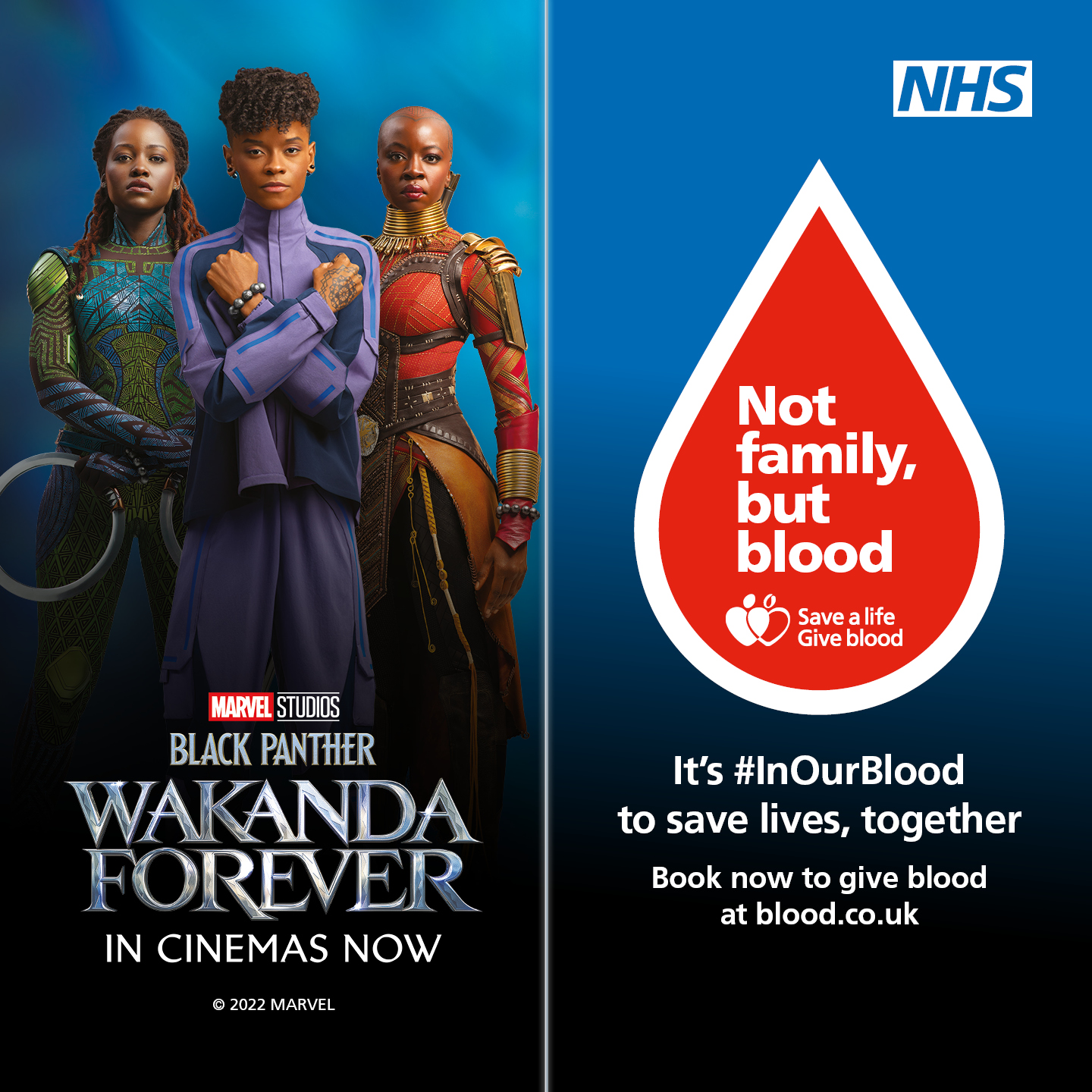
Lately we’ve been talking a lot in THINK-Health’s workflows with clients about trust and health citizenship: how inspiring positive individual health behaviors can initiate a flywheel of public health goodness. The UK’s National Health Service is acting on this concept through a new campaign to inspire people in the Black community to give blood. The NHS is linking the campaign to Marvel’s Black Panther: Wakanda Forever movie launch, which drops in UK cinemas on 11 November. Here’s the NHS video so you can get a sense of the public health message… The call-to-action: It’s #InOurBlood to save lives, together.
Health Is Social, With More People Using Apps for Physical and Emotional Wellbeing
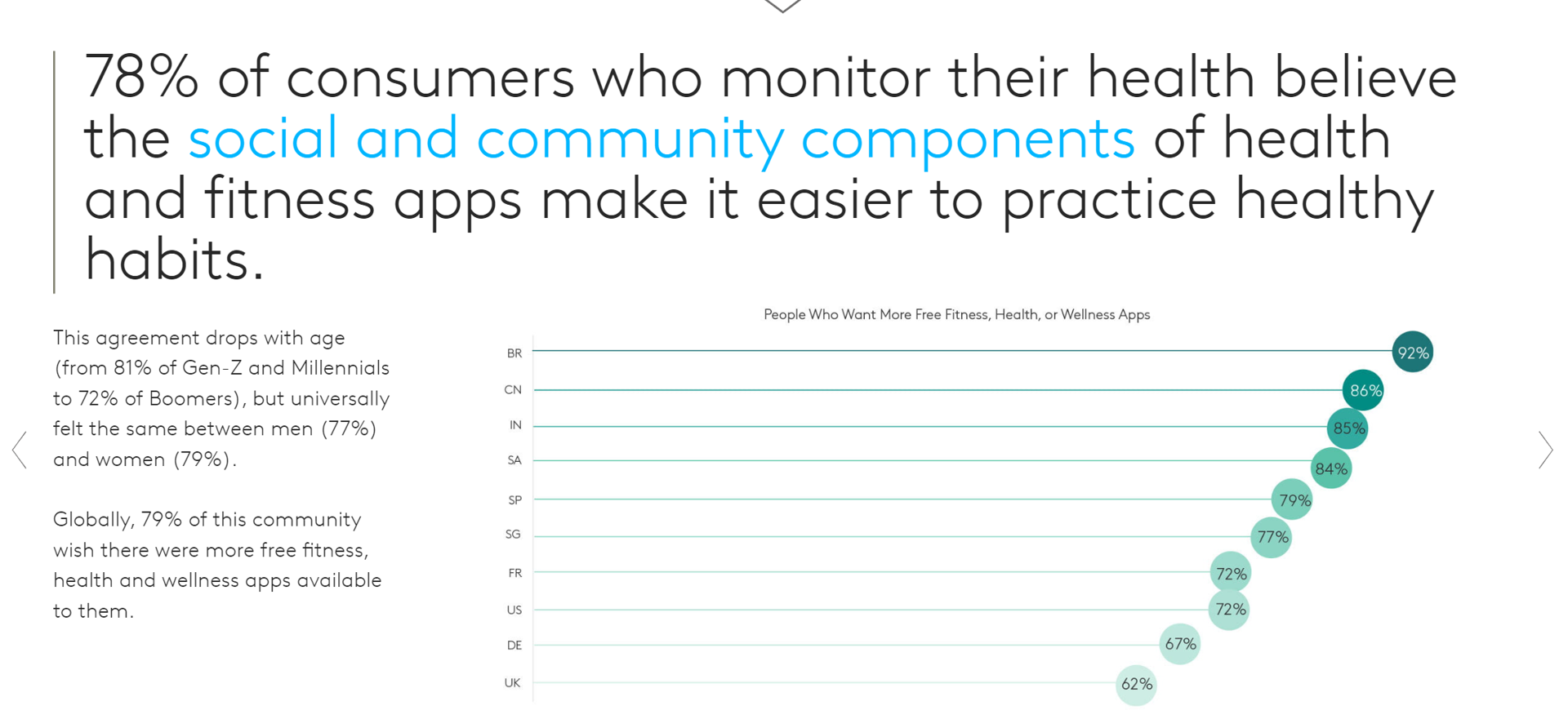
People who need people aren’t just the luckiest people in the world: they derive greater benefits through monitoring their health via apps that make it easier to make healthy choices. Channeling Barbra Streisand here to call out a key finding in new consumer research from Kantar on Connecting with the Health & Wellness Community. Kantar polled 10,000 online consumers in ten countries to gain perspectives on health citizens’ physical and emotional health and the role of technology to bolster (or diminish) well-being. The nations surveyed included Brazil, China, France, Germany, India, Singapore, South Africa, Spain,
It’s Mental Illness Awareness Week: “What I Wish I Had Known” About Mental Health

It’s Mental Illness Awareness Week: annually NAMI, the National Alliance on Mental Illness, devotes the first week of October to advocate for people facing managing a mental illness every day and to raise public consciousness on the pervasiveness of mental illness in America. This year, NAMI’s key themes address the over-arching message of “What I wish I had known,” each day looking into: Monday Oct. 3: Stigma Tuesday Oct. 4: Medication [National Day of Prayer for Mental Illness Recovery and Understanding] Wednesday Oct. 5: Therapy Thursday Oct. 6: Disclosing [National Depression Screening Day], and, Friday Oct. 7: Caregiving. To track
Consumers’ and the White House’s Growing Focus on Food and Nutrition
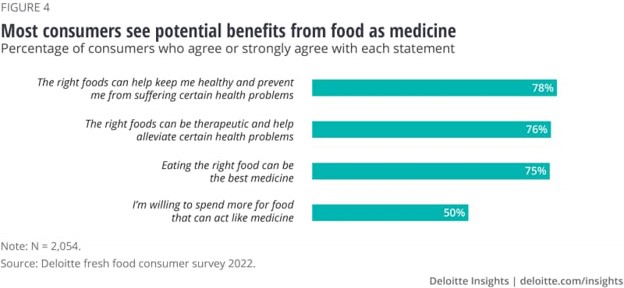
Today, the White House is convening a Conference on Hunger, Nutrition and Health. So it’s a propitious time to weave together some of the latest research and insights into food-as-medicine and a key determinant of health and well-being. This is the first White House conference focused on nutrition and food in over 50 years. The National Strategy was released today, and covers a range of programs that bake health and nutrition into Federal policies going beyond “food” itself: we see various determinants of health embedded into the Strategy, such as supporting physical activity,
Life Expectancy Falls in the U.S., the Largest 2-Year Decline in 100 Years
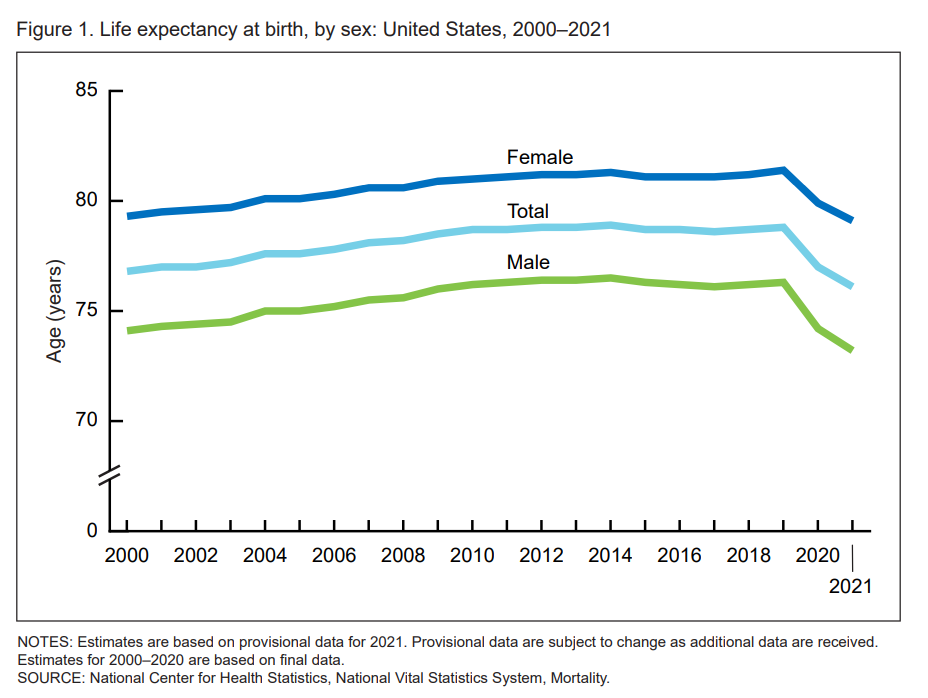
Life expectancy at birth in 2021 in the United States fell to 76.1 years, the lowest level since 1996. Men fared much worse than women, with 73,2 years of life expectancy versus 79.1 years for women, the latest research from the CDC’s National Center for Health Statistics revealed. In their Provisional Life Expectancy Estimates for 2021, the CDC kicks off a demographically detailed analysis with this simple line chart which graphs the dramatic decline in life expectancy at birth. The overall decline across gender and all race/ethnic groups was 2.7 years: 3.1 years
Health, Politics, Inflation and Women: Health Engagement at the Voting Booth
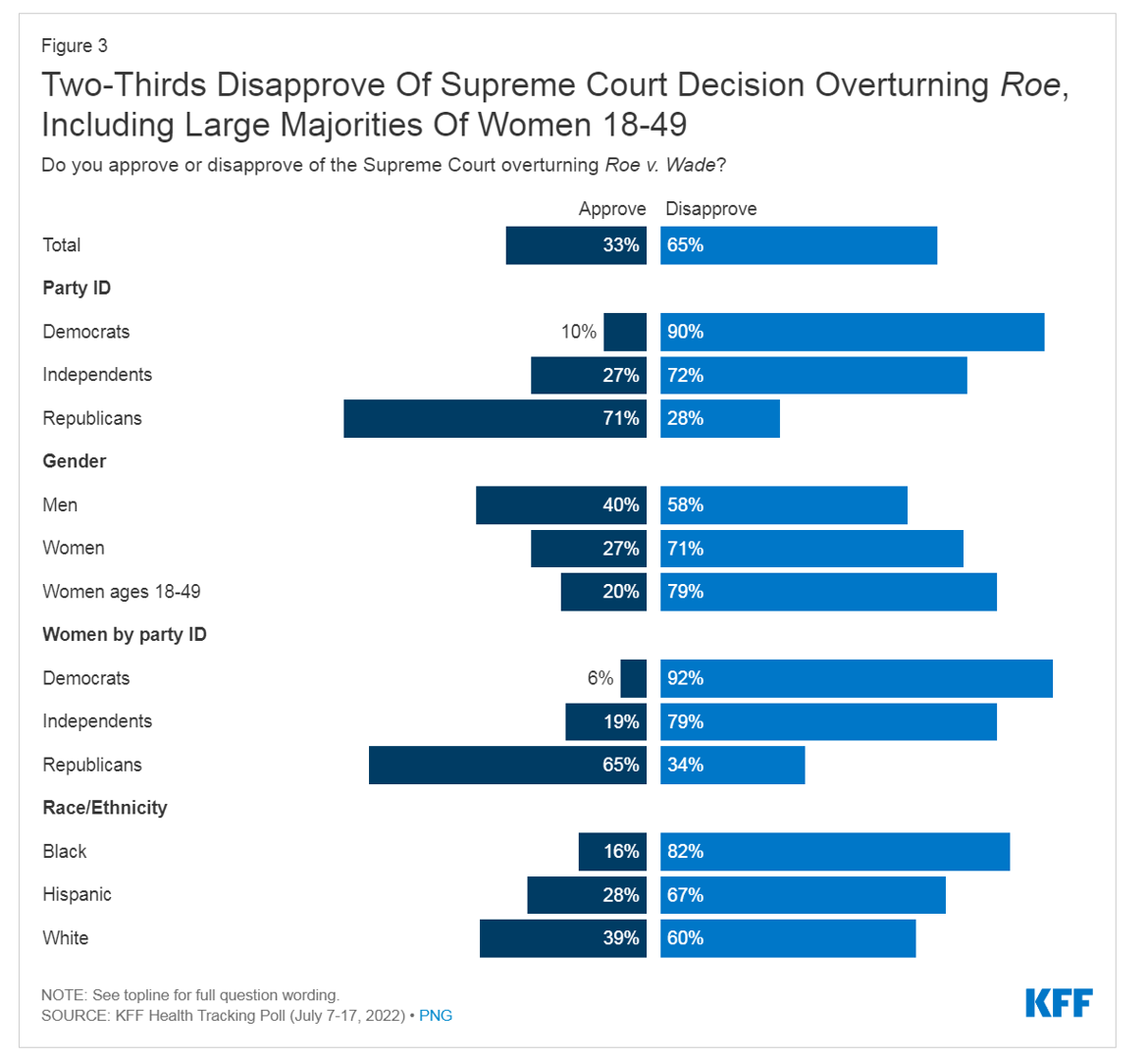
Two in three Americans disapproved of the Supreme Court’s decision to overturn the Roe v. Wade decision (aka the Dobbs case), the latest Kaiser Family Foundation Health Tracking Poll found. While inflation tops voters’ priorities, abortion access resonates for key voting blocs. KFF conducted this survey among 1,847 U.S. adults 18 and over between July 7 and 17, 2022. KFF published the study findings this week on August 2, a day of political primaries and ballot considerations in several U.S. states. Consider Kansas: a majority of Kansans voted on Tuesday to protect abortion rights
The Retail Health Battle Royale, Day 5 – Consumer Demands For a Health/Care Ecosystem (and What We Can Learn from Costco’s $1.50 Hot Dog)

In another factor to add into the retail health landscape, Dollar General (DG) the 80-year old retailer known for selling low-priced fast-moving consumer goods in peoples’ neighborhoods appointed a healthcare advisory panel this week. DG has been exploring its health-and-wellness offerings and has enlisted four physicians to advise the company’s strategy. One of the advisors, Dr. Von Nguyen, is the Clinical Lead of Public and Population Health at Google….tying back to yesterday’s post on Tech Giants in Healthcare. Just about one year ago, DG appointed the company’s first Chief Medical Officer, which I covered here in
Money and Guns Are the Top Two Sources of Anxiety in America This Summer
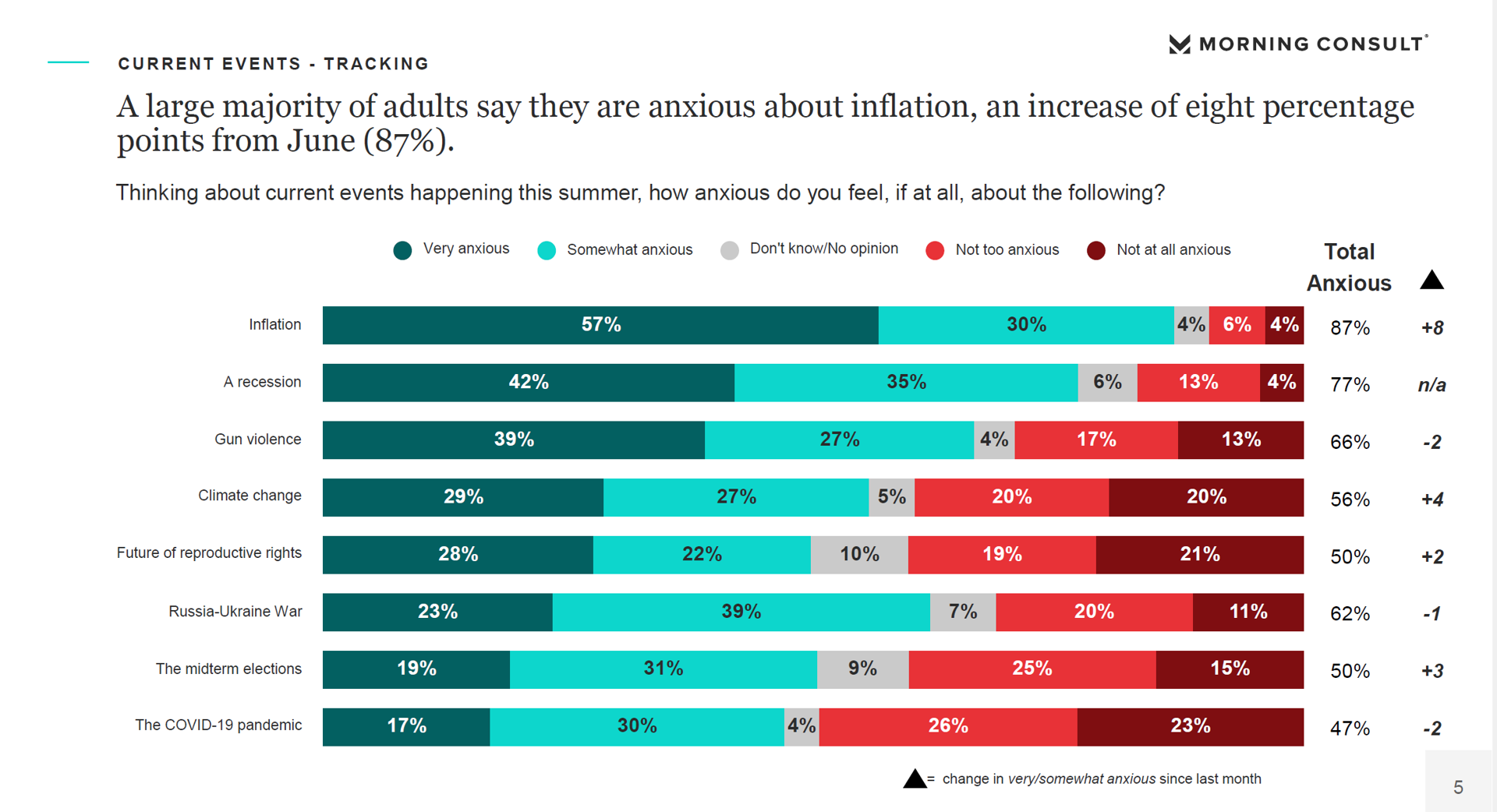
Inflation and the fear of economic recession were the top two causes of anxiety in America, followed by gun violence, in June 2022. Moms and Hispanic adults, in particular, were worried about losing income and of gun violence, discovered in the Healthy Minds Monthly Poll for July 2022 from the American Psychiatric Association (APA) and Morning Consult. For some context about these findings, note that this survey was fielded between June 18 and 20, 2022; that was, 24 days after the Robb Elementary School shooting in Uvalde, Texas Four days before the Supreme Court
Consumers’ Dilemma: Health and Wealth, Smartwatches and Transparency

Even as spending on healthcare per person in the United States is twice as much as other wealthy countries in the world, Americans’ health status ranks rock bottom versus those other rich nations. The U.S. health system continues to be marred by health inequalities and access challenges for man health citizens. Furthermore, American workers’ rank top in the world for feeling burnout from and overworked on the job. Welcome to The Consumer Dilemma: Health and Wellness,, a report from GWI based on the firm’s ongoing consumer research on peoples’ perspectives in the wake of
Use of Preventive Health Services Declined Among Commercially Insured People – With Big Differences in Telehealth for Non-White People, Castlight Finds
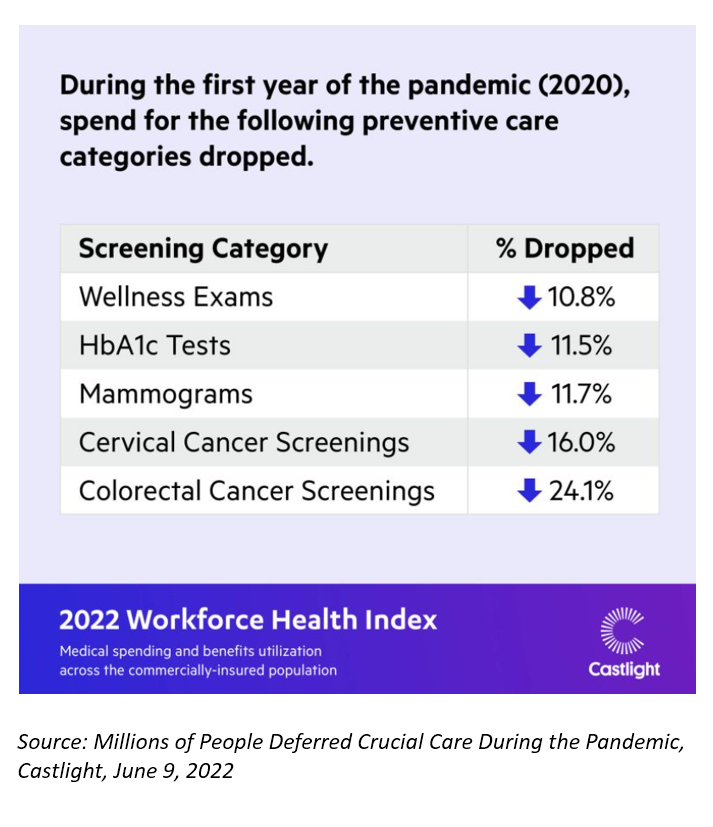
Declines in preventive care services like cancer screenings and blood glucose testing concern employers, whose continued to cover health insurance for employees during the pandemic. “As we enter the third year of the COVID-19 pandemic, employers continue to battle escalating clinical issues, including delayed care for chronic conditions, postponed preventive screenings, and the exponential increase in demand for behavioral health services,” the Chief Medical Officer for Castlight Health notes in an analysis of medical claims titled Millions of People Deferred Crucial Care During the Pandemic, published in June. The
Healthcare access, racial disparities, guns and climate – U.S. doctors are worried about some big social issues
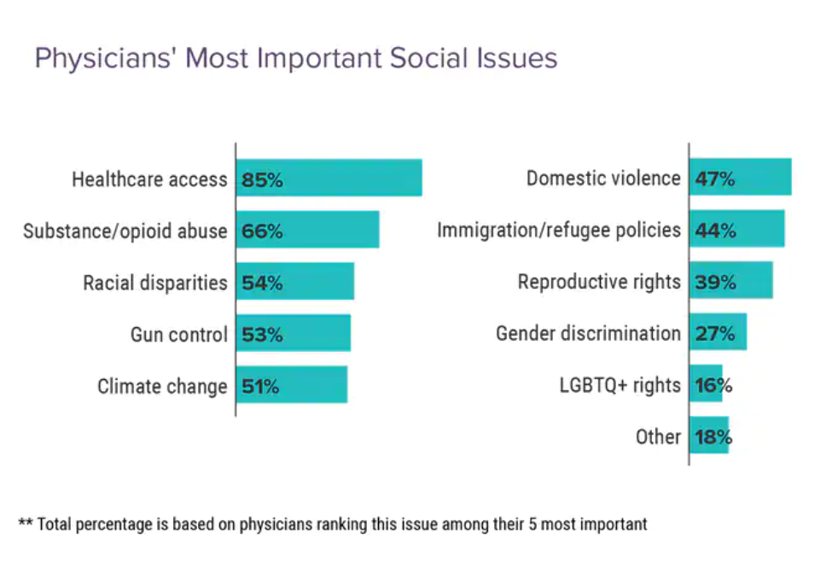
Doctors heads and hearts are jammed with concerns beyond curing patients’ medical conditions: U.S. physicians are worried about big social issues, according to a Medscape survey report, Physicians’ Views on Today’s Divisive Social Issues 2022. Topping physicians’ list of their top-five most important social issues, far above all others ranked healthcare access. Underneath that top-line statistic, it’s important to note that: 52% of doctors are “very concerned” about healthcare access, 28% are “concerned,” and 13% are “somewhat concerned.” Medscape underscores that in 2020, 31 million U.S. residents had no health insurance coverage, and
Social Determinants of Health Risks Challenge the Promise of Hospital-to-Home
In the wake of the pandemic and growing consumer preferences, the hospital-to-home movement is gaining traction among health systems. Amidst bullish forecasts for the promise of hospital-to-home discharges, the ability for many patients to make this migration would be a difficult bridge to cross. On the promising front, recent studies reviewed through a meta-analysis published in JAMA found that hospital-to-home programs can be clinically and cost-effective for inpatients discharged from hospital. Earlier this year, McKinsey addressed how “Care at Home” ecosystems can reshape the way health systems — and people — envision patient care. This
Health is Our Most Important Relationship: Inconvenient Truths from MRM/McCann Truth Central

We’ve hit a great “healthcare trust” recession around the world, translating into lower multiple points of medical ‘facts’ and pseudoscience, lower adherence to therapeutic regimens, and clinician burnout that has compromised medicine as the team sport it ideally should be. And that’s just one of five inconvenient truths unearthed in The Truth About Our Relationships with Health, the first in a series of papers that MRM is developing to, in their words, “look at the truths pr7eventing us from achieving a better relationship with our own health and with those along our health journey.” This report from MRM analyzes research
Three in Five People 50+ in the US Will Likely Use Telehealth In the Future – An Update from AARP
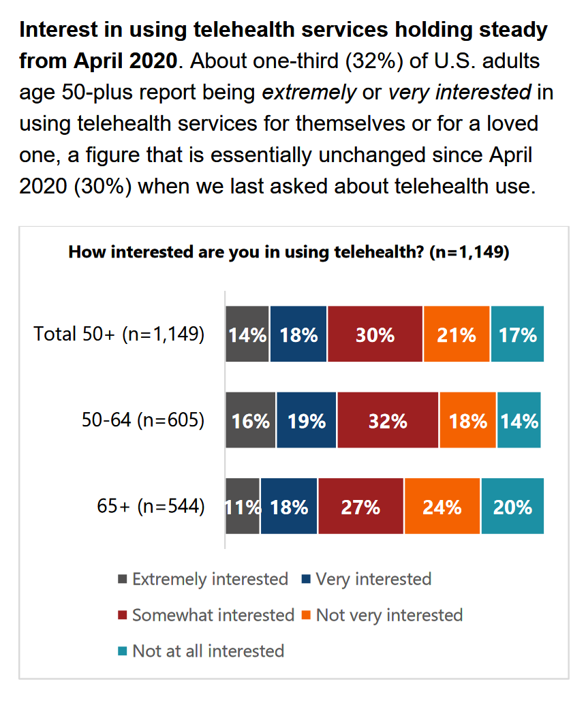
“Telehealth certainly appears to be here to stay,” the AARP forecasts in An Updated Look at Telehealth Use Among U.S. Adults 50-Plus from AARP. Two years after the emergence of the COVID-19 pandemic, one-half of U.S. adults over 50 said they or someone in their family had used telehealth. In early 2022, over half of those over 50 (the AARP core membership base) told the Association they would likely use telehealth in the future. This future expectation varies by race, the implications of which I discuss below in
People Thinking More About the Value of Health Care, Beyond Cost
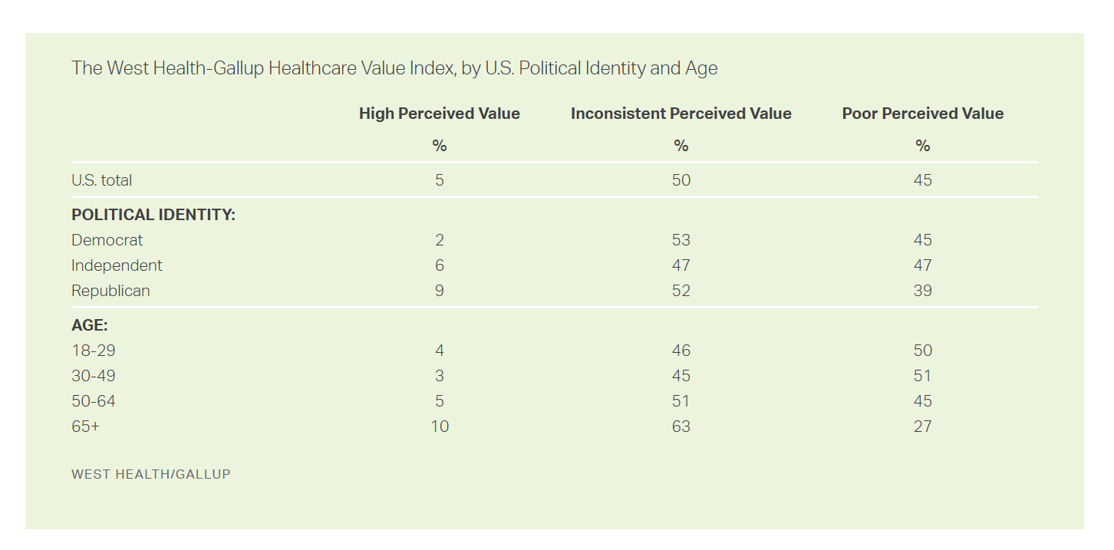
The rate of people in the U.S. skipping needed health care due to cost tripled in 2021. This prompted West Health (the Gary and Mary West nonprofit organizations’ group) and Gallup to collaborate on research to quantified Americans’ views on and challenges with personal medical costs. This has resulted in The West Health-Gallup Healthcare Affordability Index and Healthcare Value Index. The team’s research culminated in the top-line finding that some 112 million people in the U.S. struggle to pay for their care. That’s about 4.5 in 10 health citizens. Furthermore, 93% of people
The Color of Care – Oprah and The Smithsonian Channel Partner on Health Equity
A new documentary and educational campaign on health equity will be launched on May 1st, 2022, from Oprah’s Harpo Productions studio partnering with The Smithsonian Channel. The Color of Care documents stories of people who have lost loved ones in the COVID-19 pandemic as well as expert interviews with frontline workers and public health experts and researchers sharing data on systemic racism in health care that has underpinned racial health disparities since slavery was instituted in America. Oprah’s website talked about the project, quoting her saying, “At the height of the pandemic, I read something that stopped me in
How Business Can Bolster Determinants of Health: The Marmot Review for Industry
“Until now, focus on….the social determinants of health has been for government and civil society. The private sector has not been involved in the discussion or, worse, has been seen as part of the problem. It is time this changed,” asserts the report, The Business of Health Equity: The Marmot Review for Industry, sponsored by Legal & General in collaboration with University College London (UCL) Institute of Health Equity, led by Sir Michael Marmot. Sir Michael has been researching and writing about social determinants of health and health equity for decades, culminating publications
The Financial Toxicity of Health Care Costs: From Cancer to FICO Scores
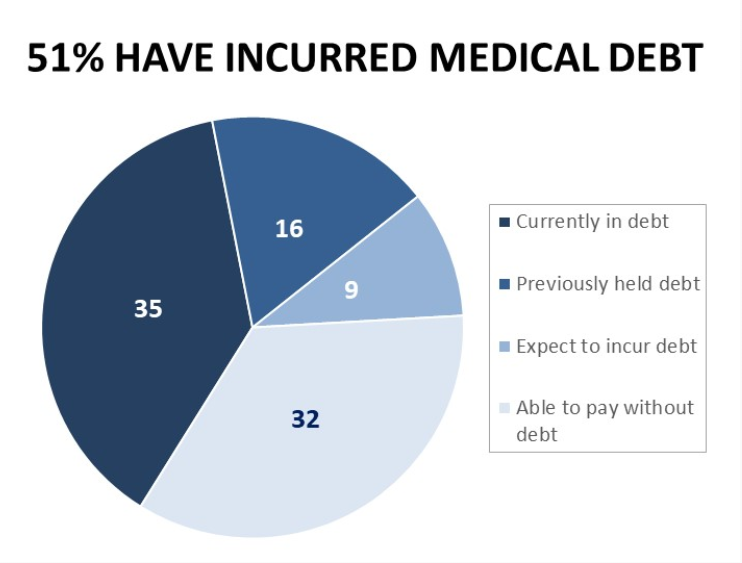
The financial toxicity of health care costs in the U.S. takes center stage in Health Populi this week as several events converge to highlight medical debt as a unique feature in American health care. “Medical debt is the most common collection tradeline reported on consumer credit records,” the Consumer Financial Protection Bureau called out in a report published March 1, 2022. CFPB published the report marking two years into the pandemic, discussing concerns about medical debt collections and reporting that grew during the COVID-19 crisis. Let’s connect the dots on: A joint announcement this week from three major credit agencies,
Stress in America on the Pandemic’s 2nd Anniversary: Money, Inflation, and War Add to Consumers’ Anxiety
As we mark the second anniversary of the COVID-19 pandemic, the key themes facing health citizens deal with money, inflation, and war — “piled on a nation stuck in COVID-19 survival mode,” according to the latest poll on Stress in America from the American Psychological Association. Financial health is embedded in peoples’ overall sense of well-being and whole health. Many national economies entered the coronavirus pandemic in early 2020 already marked by income inequality. The public health crisis exacerbated that, especially among women who were harder hit financially in the past two years than men were. That situation was even worse
How Social Media Can Get Public Health So Wrong
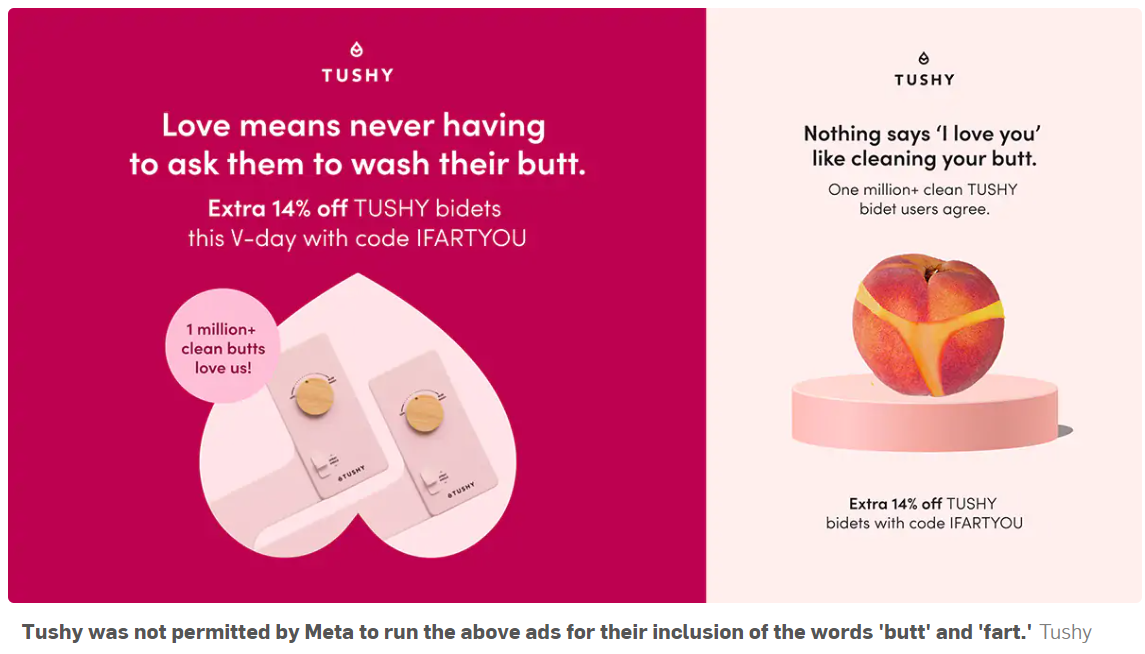
This week, public health truths have collided with social media, the infodemic, and health citizenship. First, I read in Becker’s Health IT on February 16 that the peer-reviewed policy journal Health Affairs was prevented by a social media outlet from promoting its February 2022 issue themed “Racism and Health.” The company said the topic was too controversial to feature in this moment. “Google and Twitter are blocking its paid media ads to promote the content, flagging racism as ‘sensitive content,'” Molly Gamble explained in Becker’s. I myself used the blogging platform you’re on now to promote the February ’22 issue of
Love and Health: The Education of Abner Mason, SameSky Health
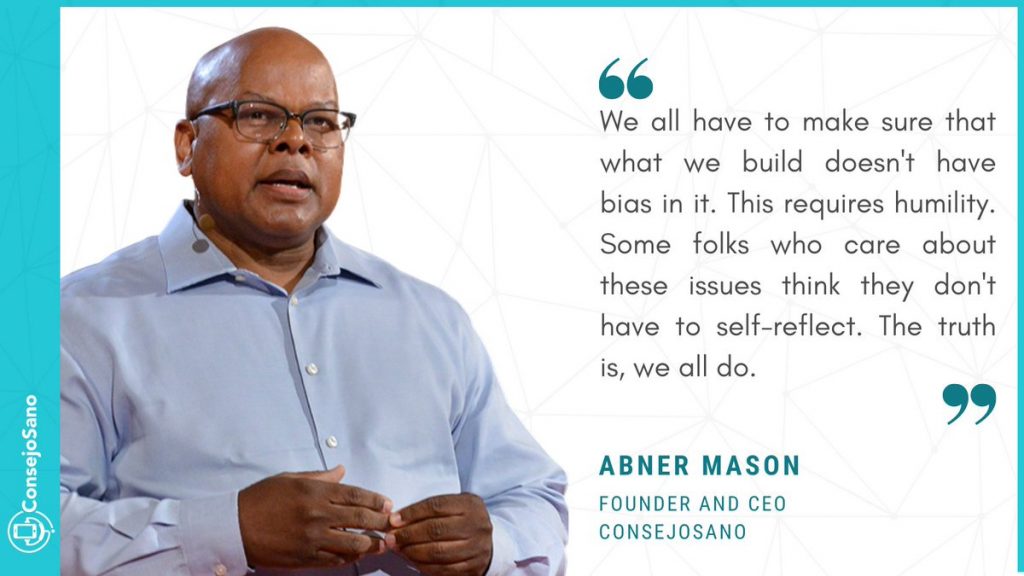
It felt super appropriate that I met up with Abner Mason, Founder of SameSky Health, on Valentine’s Day 2022. While we conversed via Zoom, Abner’s positive energy vibrated over the 5,600 miles between him in LA County and me in Brussels, Belgium – nine hours apart, but in the proverbial same room in the conversation. My initial ask of Abner was to discuss the re-branding of ConsejoSano to SameSky Health, but I first wanted to hear the man’s origin story. And that, you will learn, has everything to do with loving parents, the power of education from a young age,
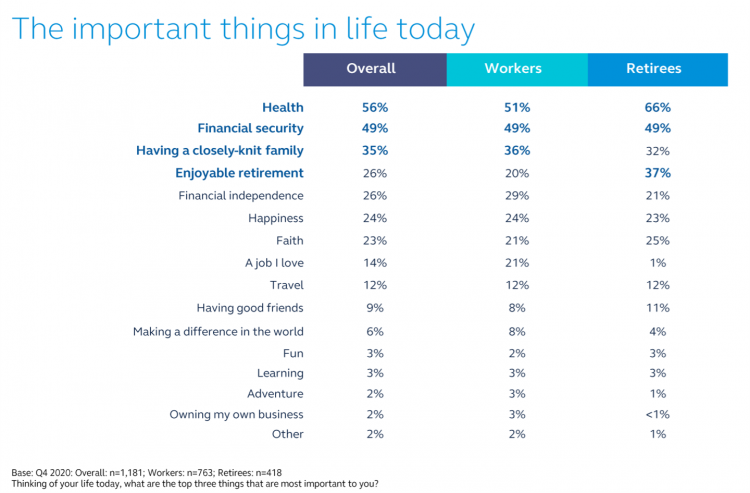
Health Care Planning for 2022 – Start with a Pandemic, Then Pivot to Health and Happiness

One of my favorite Dr. Seuss characters is the narrator featured in the book, I Had Trouble In Getting to Solla-Sollew. I frequently use this book when conducting futures and scenario planning sessions with clients in health/care. “The story opens with our happy-go-lucky narrator taking a stroll through the Valley of Vung where nothing went wrong,” the Seussblog explains. Then one day, our hero (shown here on the right side of the picture from the book) is not paying attention to where he is walking….thus admitting, “And I learned there are troubles of more than one kind, some come from
Designing Digital Health for Public Health Preparedness and Equity: the Consumer Tech Association Doubles Down
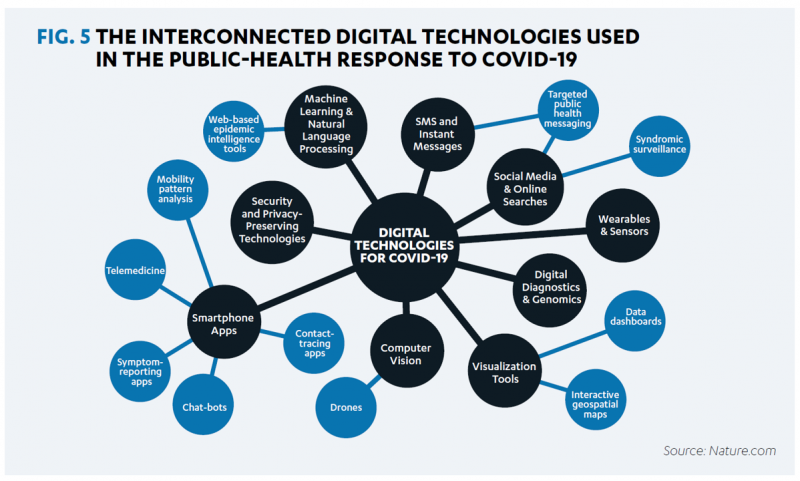
A coalition of health care providers, health plans, technology innovators, NGOs, and medical societies has come together as the Public Health Tech Initiative (PHTI), endorsed by the Consumer Technology Association (CTA) with the goal of advancing the use of trustworthy digital health to proactively meet the challenge of future public health emergencies….like pandemics. At the same time, CTA has published a paper on Advancing Health Equity Through Technology which complements and reinforces the PHTI announcement and objective. The paper that details the PHTI program, Using Heath Technology to Response to Public Health Emergencies, identifies the two focus areas: Digital health
Still Struggling with Stress in America in 2021
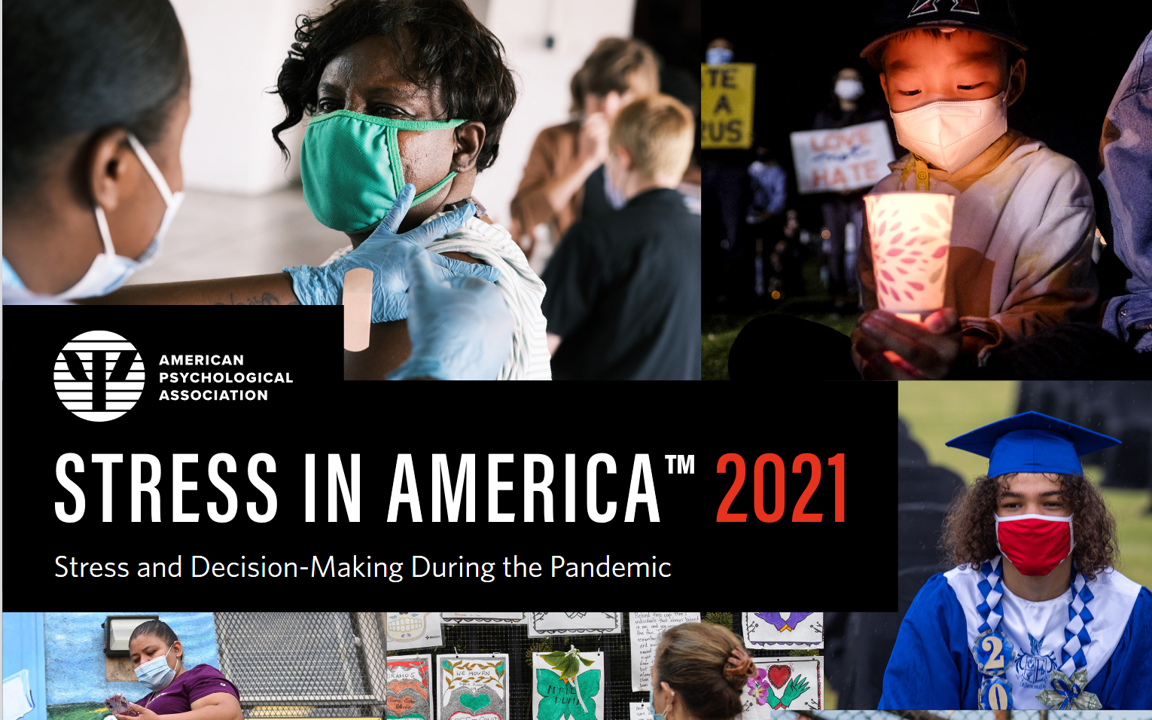
“Americans remain in limbo between lives once lived and whatever the post-pandemic future holds,” the American Psychological Association observes in their latest read into Stress in America 2021, with this phase of the perennial study focused on Stress and Decision-Making During the Pandemic. The top-line: people face a daily web of risk assessment, up-ended routines, and endless news about the coronavirus locally and globally. While most people in the U.S. believe that “everything will work out” after the pandemic ends, the mental, emotional, and logistical daily distance between “now” and “then” brings uncertainty and indeed, prolonged stress. More Millennials, who
Consider Mental Health Equity on World Mental Health Day
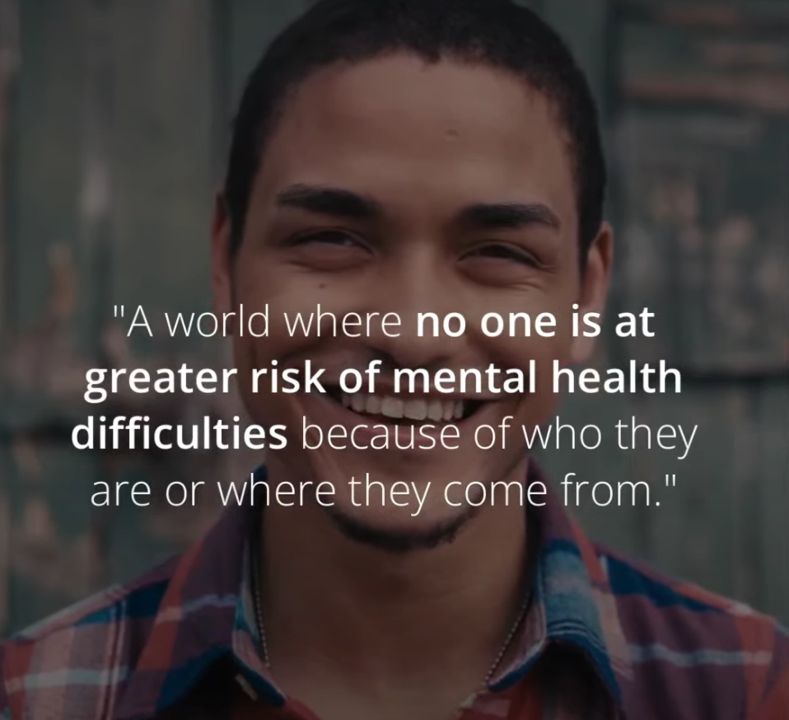
COVID-19 exacted a toll on health citizens’ mental health, worsening a public health challenge that was already acute before the pandemic. It’s World Mental Health Day, an event marked by global and local stakeholders across the mental health ecosystem. On the global front, the World Health Organization (WHO) describes the universal phenomenon and burden of mental health on the Earth’s people… Nearly 1 billion people have a mental disorder Depression is a leading cause of disability worldwide, impacting about 5% of the world’s population People with severe mental disorders like schizophrenia tend to die as much as 20 years earlier
Genentech’s Look Into the Mirror of Health Inequities

In 2020, Genentech launched its first study into health inequities. The company spelled out their rationale to undertake this research very clearly: “Through our work pursuing groundbreaking science and developing medicines for people with life-threatening diseases, we consistently witness an underrepresentation of non-white patients in clinical research. We have understood inequities and disproportionate enrollment in clinical trials existed, but nowhere could we find if patients of color had been directly asked: ‘why?’ So, we undertook a landmark study to elevate the perspectives of these medically disenfranchised individuals and reveal how this long-standing inequity impacts their relationships with the healthcare system
A Nutrition Label for Health IT
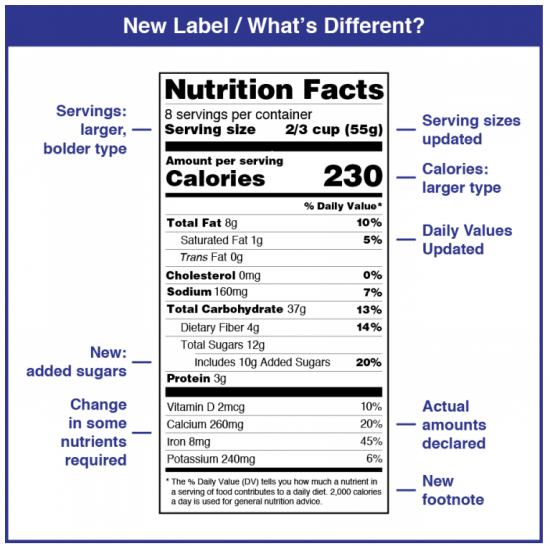
“Shouldn’t we, as a society, demand a nutrition label on our algorithms?” asked Dr. John Halamka. Dr. Halamka, President of the Mayo Clinic Platform, was speaking at the HIMSS 2021 annual conference on the meeting’s digital channel. Artificial intelligence and health equity were two key themes discussed during #HIMSS21, and Dr. Halamka’s concerns echoed through the week-long event. To illustrate the need for a healthier approach to AI, he offered this scenario: “If I use a data set of one million Scandinavian Lutherans to create the most amazing EKG algorithm ever and then we decide to use it in Spain,
Health Disparities in America: JAMA Talks Structural Racism in U.S. Health Care

“Racial and ethnic inequities in the US health care system have been unremitting since the beginning of the country. In the 19th and 20th centuries, segregated black hospitals were emblematic of separate but unequal health care,” begins the editorial introducing an entire issue of JAMA dedicated to racial and ethnic disparities and inequities in medicine and health care, published August 17, 2021. This is not your typical edition of the Journal of the American Medical Association. The coronavirus pandemic has changed so many aspects of American health care for so many people, including doctors. Since the second quarter of 2020,
Nurses and Aides Are Beloved and Deserve Higher Pay; and a Spotlight on the Filipinx Frontline
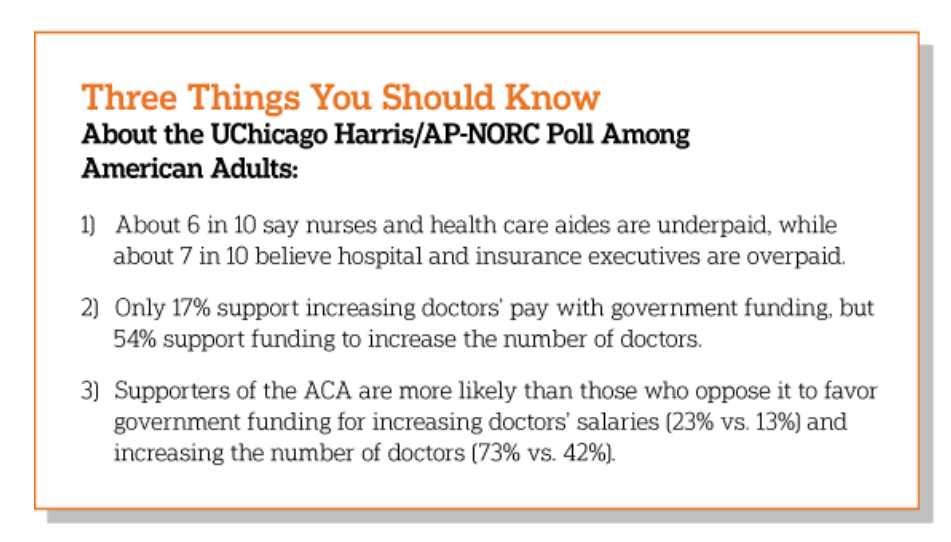
A majority of Democrats, Independents, and Republicans agree that nurses are underpaid. Most Americans across political parties also believe that hospital executives are overpaid, according to a poll from The Associated Press-NORC Center for Public Affairs Research. The survey analysis is aptly titled, Most Americans Agree That Nurses and Aides Are Underpaid, While Few Support Using Federal Dollars to Increase Pay for Doctors, . Insurance executives are also overpaid, according to 73% of Americans — an even higher percent of people than the 68% saying hospital execs make too much money. In addition to nurses being underpaid, 6 in 10
Our Pandemic Lessons: Listening to Michael Dowling – a #HIMSS21 Wrap-Up

“We don’t un-learn,” Dr. Amy Abernethy asserted as she shared her pandemic perspectives on a panel with 2 other former U.S. health policy and regulatory leaders. The three spoke about navigating compliance (think: regulations and reimbursement) in an uncertain world. An uncertain world is our workplace in the health/care ecosystem, globally, in this moment. So to give us some comfort in our collective foxhole, my last post for this week of immersion in #HIMSS21 is based on the keynote speech of Michael Dowling, CEO of Northwell Health. Dowling keynoted on the theme of “Leading for the Future,” sharing his lessons
What Poor Birth and Maternity Outcomes in the U.S. Say About American Healthcare & “Infrastructure”
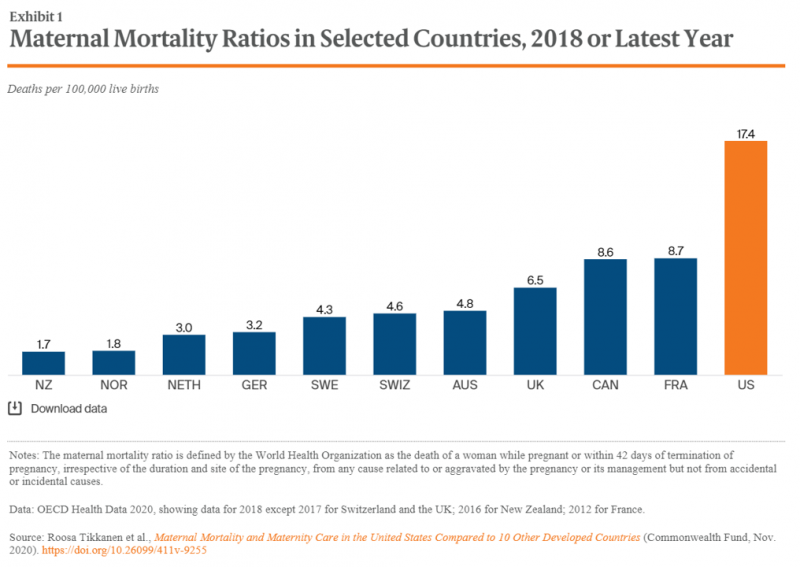
Cain Brothers is a 100+ year old financial services firm with a strong health care experience, now part of KeyBanc. A recent “House Calls” memo and podcast from two company analysts detailed the state of Medicaid, Motherhood and America’s Future: Giving Birth to Better Maternity Outcomes. Christian Pesci and David Johnson’s in-depth discussion detailed their bottom-line that, “maternity care in the U.S. is in crisis but poised for rapid evolution…(recognizing) that an uncoordinated system with misaligned incentives harms too many individuals, families, and communities.” They lay out the crisis as follows: Medicaid funds nearly one-half of births in the U.S.
CVS Finds Differences in Mental and Behavioral Health Among Men Vs. Women in the Pandemic
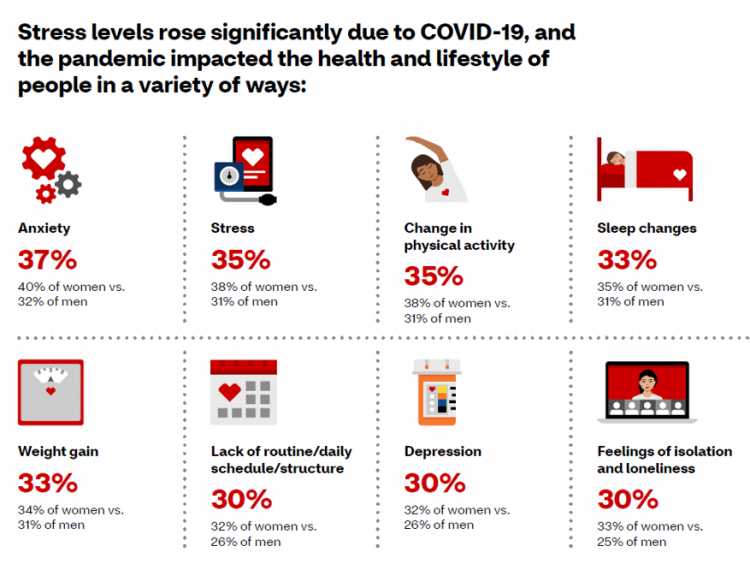
As the COVID-19 pandemic shifts to a more endemic phase — becoming part of peoples’ everyday life for months to come — impacts on peoples’ mental health will persist, according to new research from CVS Health in the company’s annual Health Care Insights Study. CVS conducted the annual Health Care Insights Study among 1,000 U.S. adults in March 2021. To complement the consumer study, an additional survey was undertaken among 400 health care providers including primary care physicians and specialists, nurse practitioners, physician assistants, RNs and pharmacists. CVS has been tracking the growing trend of health care consumerism in the
The Many Factors That Make a Child’s Well-Being Build Our Adult Health – the Aspirational OECD Framework
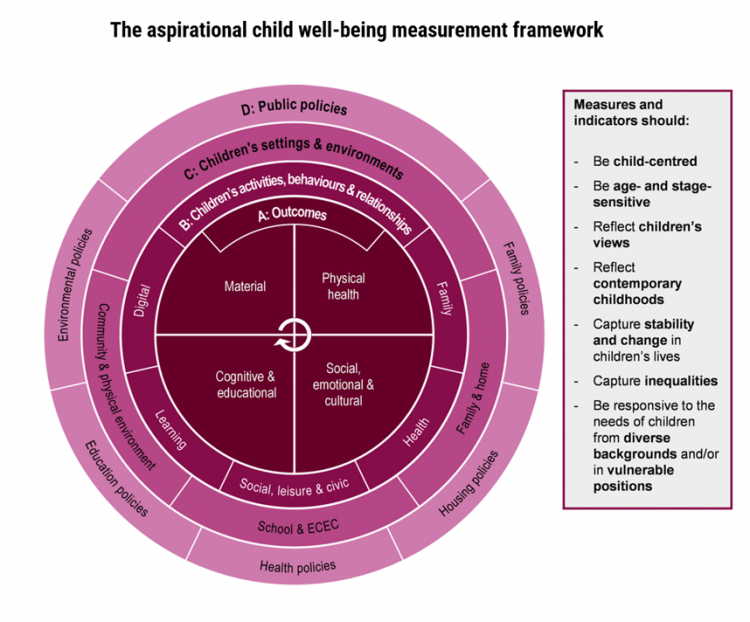
The ultimate health and wellbeing of an adult depends on the factors that shape us when we are children. A new, deep report from the OECD, Measuring What Matters for Child Well-being and Policies, spells out the many domains of experience that, together, bolster our whole health as we grow from child to adult. The first chart presents the OECD’s framework for measuring child well-being, calling out the nature of being “aspirational.” This re-look at children’s health data is aspirational because it is laying out how to best measure child well-being to set the bar higher for doing so. It addresses
5.5 Million Years of Life Will Be Lost Due to COVID-19 in the U.S. in 2020
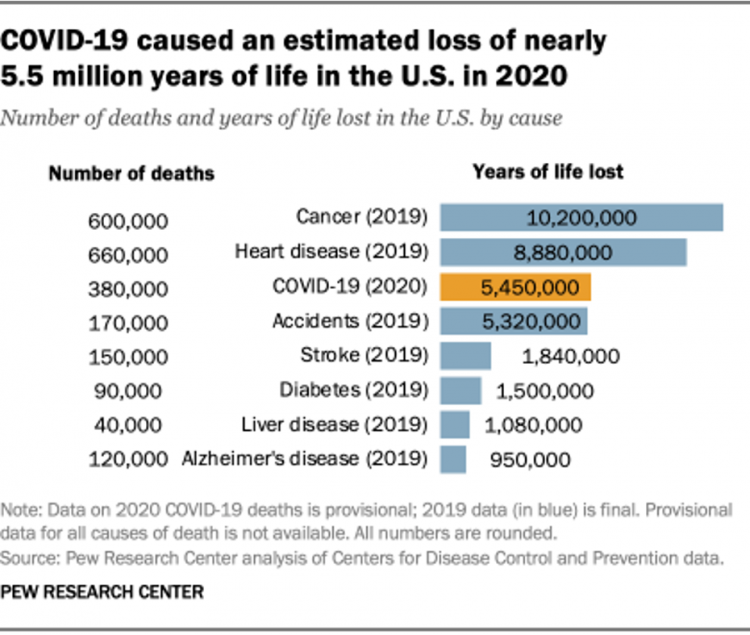
In 2020 in the U.S., 380,000 people are expected to die due to COVID-19. These people lost due to the coronavirus would, collectively, have lived another 5.5 million life-years would they not have succumbed to the virus. COVID-19 has cut lives short relative to their life expectancy, calculated in an analysis by the Pew Research Center based on CDC data from 2019 and 2020, coupled with additional statistics on life expectancy by age and gender. The bottom-line from the Pew Research Center’s analysis, simply stated, is that, “The pandemic…has killed many Americans who otherwise might have expected to live for
Thinking Mothers’ Health at Mother’s Day 2021…and the Marshall Plan for Moms

To all the Moms I’ve loved and lost and those I still blessed to have in my life…. I’m thinking about our collective and individual health this 2021 Mother’s Day weekend. There are three themes that whirl in the current Moms’ Health Mix: The impact of the COVID-19 pandemic on mothers’ health and life Mom-economics and the She-Cession — the financial roots of health inequity, and The larger context that is the persistence of women’s health disparities. First, the impact of the coronavirus and the economy have been intertwined, hitting women hard in terms of physical health, work, mental health
Health Disparities and the Risks of Social Determinants for COVID-19 – 14 Months of Evidence
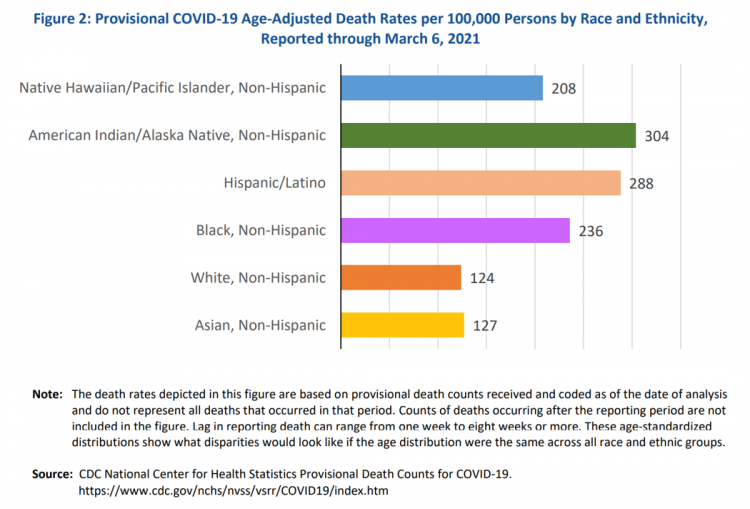
In April 2020, the U.S. Centers for Disease Control issued a report featuring evidence that in the month of March 2020, the coronavirus pandemic was not an equal-opportunity killer. Within just a couple of months of COVID-19 emerging in America, it became clear that health disparities were evident in outcomes due to complications from the coronavirus. An update from that early look at differences in COVID-19 diagnoses and mortality rates was published in Health Disparities by Race and Ethnicity During the COVID-19 Pandemic: Current Evidence and Policy Approaches, In this report, the Assistant Secretary for Planning and Evaluation, part of
Health, the Great Unifier (For Most)

As the COVID-19 expanded peoples’ consciousness about infectious disease and opportunities to keep a tricky virus at bay, consumers grew new muscles about public and individual wellness…now, “more invested in achieving it,” according to In Health We Trust, a survey report from Healthline Media. To gauge Americans changing perspectives on personal health, HealthLine conducted surveys among 1,533 U.S. consumers age 18 and over in February 2020 (just about the time the coronavirus pandemic was emerging in the U.S.) and 1,577 consumers in December 2020. One of the subtle shifts in health care consumerism concerns cost, which before the pandemic has
A Year Into COVID19, Mental Health Impacts Heavier on Moms Than Dads in America
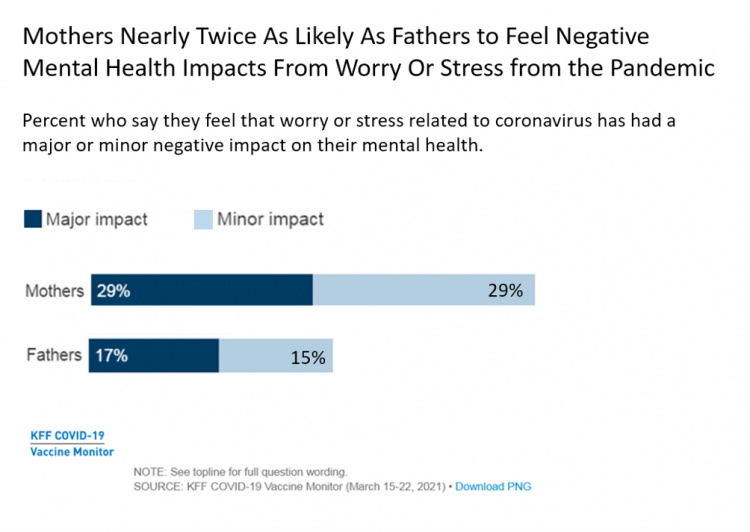
In the summer of 2020, four months into the pandemic, one-half of people living in the U.S. felt worry or stress related to the coronavirus that had a negative impact on their mental health. Over a year into the COVID-19 in America, nearly one-half of people still have negative mental health impacts due to the coronavirus, based on research from the Kaiser Family Foundation (KFF) published in their April 2021 update on the mental health impact of the COVID-19 pandemic. Note the line in the bar chart from the study has flat-lined and settled at just about 50% of U.S.
The Pandemic’s Death Rate in the U.S.: High Per Capita Income, High Mortality
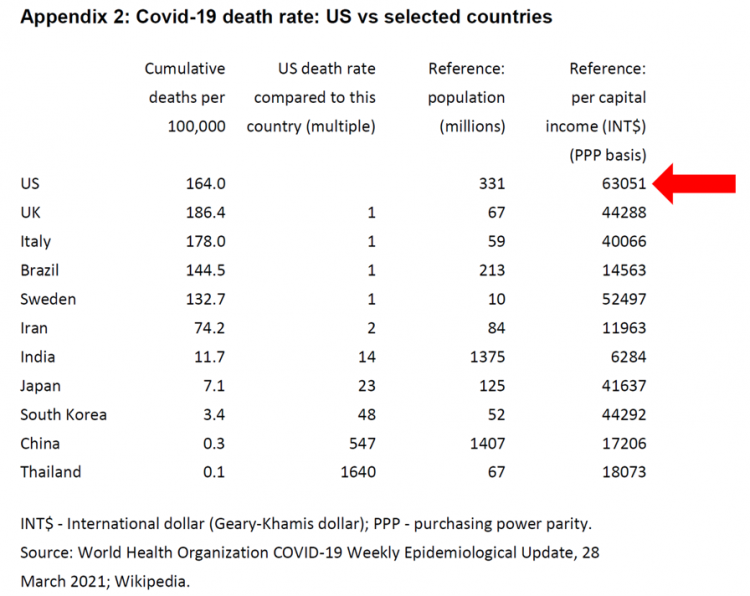
The United States has among the highest per capita incomes in the world. The U.S. also has sustained among the highest death rates per 100,000 people due to COVID-19, based on epidemiological data from the World Health Organization’s March 28, 2021, update. Higher incomes won’t prevent a person from death-by-coronavirus, but risks for the social determinants of health — exacerbated by income inequality — will and do. I have the good fortune of access to a study group paper shared by Paul Sheard, Research Fellow at the Mossaver-Rahmani Center for Business and Government at the Harvard Kennedy School. In reviewing
The Cost of Healthcare Can Drive Medical Rationing and Crowd Out Other Household Spending
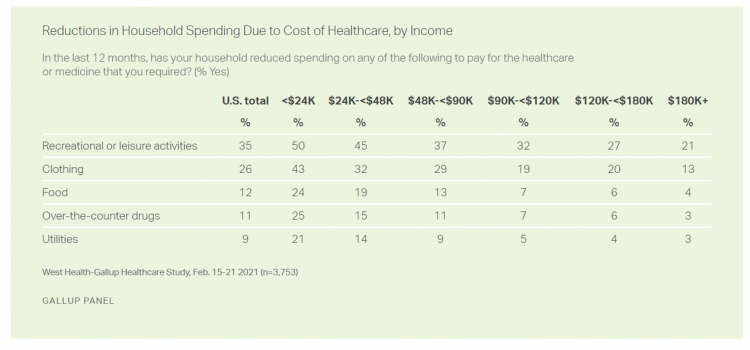
One in five people in the U.S. cannot afford to pay for quality health care — an especially acute challenge for Black and Hispanic Americans, according to a West Health-Gallup poll conducted in March 2021, a year into the COVID-19 pandemic. “The cost of healthcare and its potential ramifications continues to serve as a burdensome part of day-to-day life for millions of Americans,” the study summary observed. Furthermore, “These realities can spill over into other health issues, such as delays in diagnoses of new cancer and associated treatments that are due to forgoing needed care,” the researchers expected. The first table
Housing as Prescription for Health/Care – in Medecision Liberation

COVID-19 ushered in the era of our homes as safe havens for work, shopping, education, fitness-awaking, bread-baking, and health-making. In my latest essay written for Medecision, I weave together new and important data and evidence supporting the basic social determinant of health — shelter, housing, home — and some innovations supporting housing-as-medicine from CVS Health, UnitedHealth Group, AHIP, Brookings Institution, the Urban Land Institute, and other stakeholders learning how housing underpins our health — physical, mental, financial. Read about a wonderful development from Communidad Partners, working with the Veritas Impact Partners group, channeling telehealth to housing programs serving residents with
How Fruits and Veg Can Make Health and Lower Costs – Calling Chef José Andrés to the White House
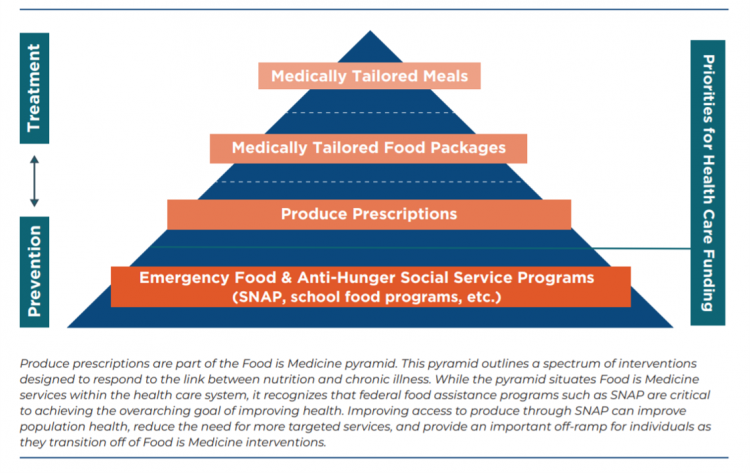
Springtime is finally emerging on the east coast of the U.S. and my local CSA farm is on my mind. It’s timely, then, to re-visit a research paper on subsidizing fruits and vegetables from a March 2019 issue of PLOS as an introduction to a new initiative growing out of The Center for Health Law and Policy Innovation of Harvard Law School (CHLPI) on produce prescriptions. Timely, too, that Chef José Andrés has been called to President Biden’s White House to help address food security in America. First, let’s look at the research in PLOS: Cost-effectiveness of financial incentives for
The Patient Safety Issue of Racial Disparities and the Opportunity for “Health Equity By Design”

In 2021, racial and ethnic disparities in healthcare are a top patient safety issue, according to ECRI’s annual list of major concerns facing healthcare consumers’ risks to adverse events that can harm them. ECRI has published their annual Top 10 list since 2018, when the list featured diagnostic errors, o behavioral health needs in acute care settings, and patient engagement and health literacy — all of which play into this year’s #1 issue, racial and ethnic disparities in health care. In fact, among the risks in this year’s Top Ten list, eight were accelerated and highlighted by the COVID-19 pandemic
The Continued Erosion of Trust in the Age of COVID
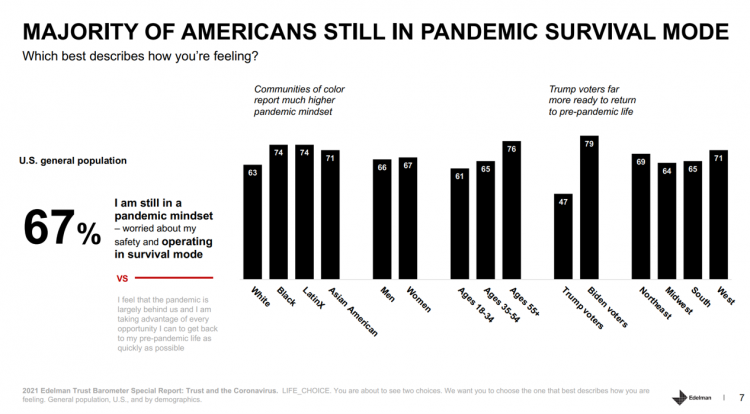
A year into the COVID-19 pandemic, most Americans are still in “survival mode,” according to an update of the 2021 Edelman Trust Barometer, Trust and the Coronavirus in the U.S. Updating the company’s annual Trust Barometer, Edelman conducted a new round of interviews in the U.S. among 2,500 people in early March. [For context, you can read my take on the 2021 Edelman Trust Barometer published during the World Economic Forum in January 2021 here in Health Populi]. The first chart shows that two in three people in the U.S. are still in a pandemic mindset, worried about safety and
Stress in America, One Year into the Pandemic – an APA Update on Parents, Healthcare Workers, and Black Americans
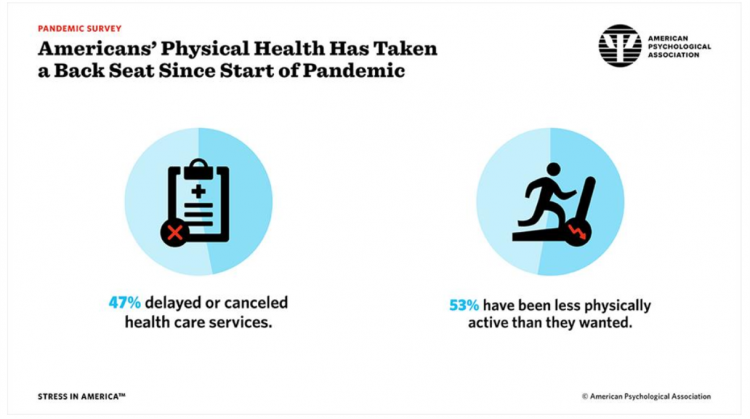
A Year into our collective coronavirus experience, Americans remain stressed, with physical health taking a back seat to our daily grinds based on the 2021 Stress in America survey from the American Psychological Association (APA). The APA has been updating us on U.S.-stress for several years, and more frequently since the start of the COVID-19 pandemic at the start of 2020. In their latest report, APA updates their previous profiles of Americans’ stress looking into different demographic groups and coping mechanisms. The topline, across all adults living in America, is that one-half have delayed or cancelled health care services. One-half has
How Young People Are Using Digital Tools to Help Deal with Mental Health
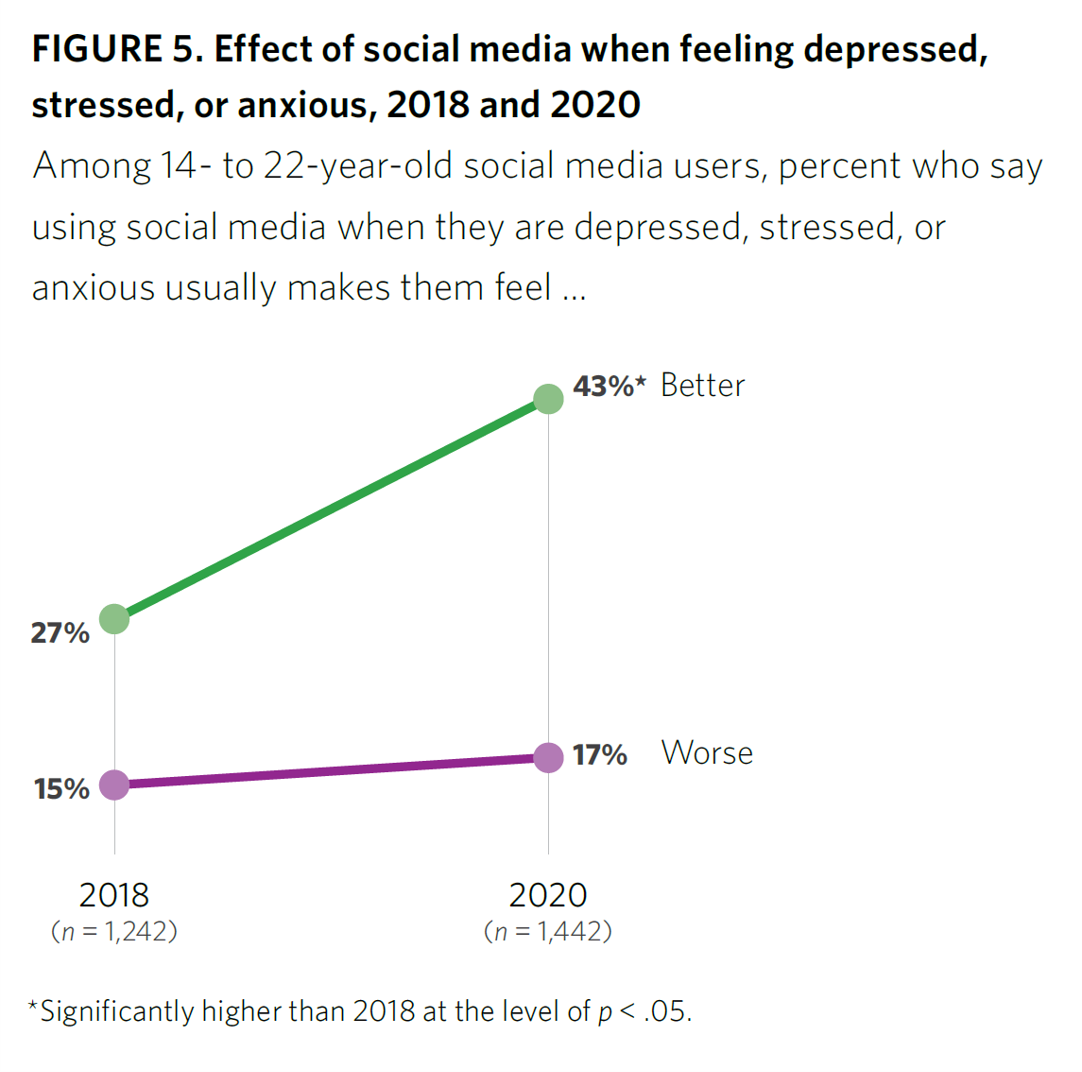
After a year of living with and “in” the coronavirus pandemic, younger people in the U.S. have had to deal with over twelve months of quarantine and lockdown, going to school remotely from home, and distancing from friends. For most young people, the public health crisis has been more about that social distancing from friends, a collective sense of isolation, and mental and behavioral health impacts. These dynamics and these young health citizens’ coping mechanisms are captured in the report, Coping with COVID-19: How Young People Use Digital Media to Manage Their Mental Health. Three organizations collaborated to conduct and
The Ongoing Reality of COVID-19 – My Conversation with Dr. Michael Osterholm at SXSW
“So close and yet so far” feels like the right phrase to use a year after the World Health Organization used the “P-word,” “pandemic,” to describe the coronavirus’s impact on public health, globally. One year and over 550,000 COVID-related deaths in the U.S. later, we face a New Reality that Dr. Michael Osterholm and I are brainstorming today at the 2021 South-by-Southwest Festival. Usually held live and very up-close-and-personally crowded in Austin, Texas, this year we are all virtual — including the film, music, and interactive festivals alike. While I regret to not be in the same room as Dr.
A BA Degree as Prescription for a Longer Life – Update on Deaths of Despair from Deaton and Case
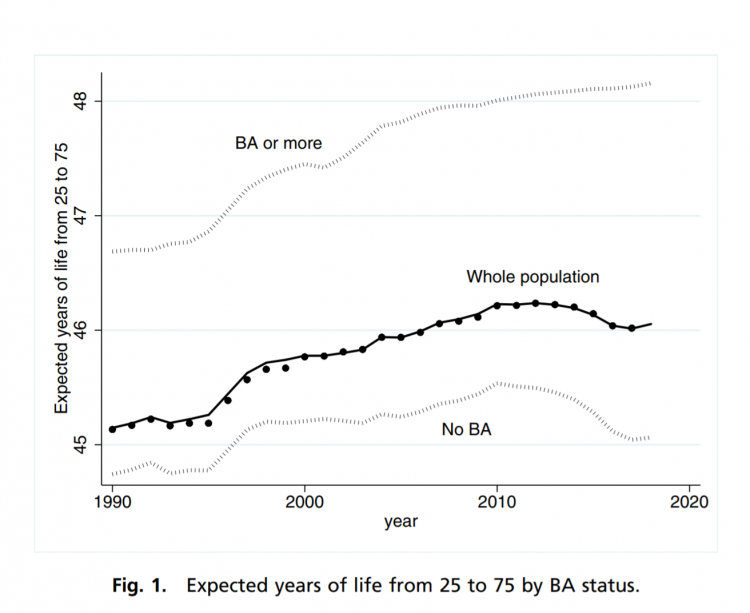
“Without a four-year college diploma, it is increasingly difficult to build a meaningful and successful life in the United States,” according to an essay in PNAS, Life expectancy in adulthood is falling for those without a BA degree, but as educational gaps have widened, racial gaps have narrowed by Anne Case and Angus Deaton. Case and Deaton have done extensive research on the phenomenon of Deaths of Despair, the growing epidemic of mortality among people due to accidents, drug overdoses, and suicide. Case and Deaton wrote the book on Deaths of Despair (detailed here in Health Populi), Case and Deaton
How to Restore Americans’ Confidence in U.S. Health Care: Deal With Access and Cost
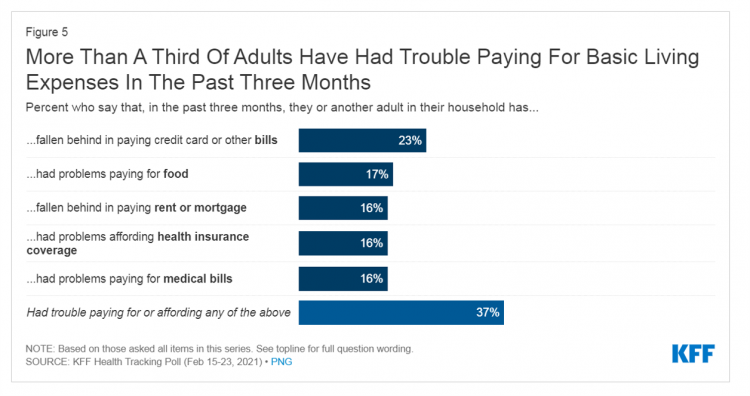
With a vaccine supply proliferating in the U.S. and more health citizens getting their first jabs, there’s growing optimism in America looking to the next-normal by, perhaps, July 4th holiday weekend as President Biden reads the pandemic tea leaves. But that won’t mean Americans will be ready to return to pre-pandemic health care visits to hospital and doctor’s offices. Now that hygiene protocols are well-established in health care providers’ settings, at least two other major consumer barriers to seeking care must be addressed: cost and access. The latest (March 2021) Kaiser Family Foundation Tracking Poll learned that at least one
The Most Relevant Companies in Health Care – Learning from the W2O Group
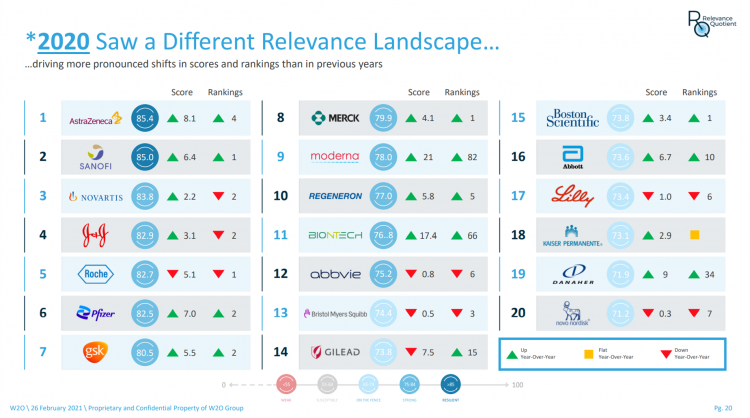
Five years ago, in 2016, the W2O Group said that, “Relevance is reputation.” That year the firm began to study the relevance of, well, relevance for organizations especially operating in the health/care ecosystem. 2020 changed everything, the W2O team asserts, now issuing its latest look into the issue through the Relevance Quotient. Relevance is built on recognizing, meeting and exceeding stakeholder expectations of organizations. In the Relevance Quotient methodology, W2O Group defines key stakeholders as employees, patients (including the sick and the well, caregivers, consumers, et al), health care providers, advocacy groups, analysts and investors, policy makers, journalists and media outlets.
Americans Lost Future Life-Years in 2020: How Much Life Was Lost Depends on the Color of One’s Skin
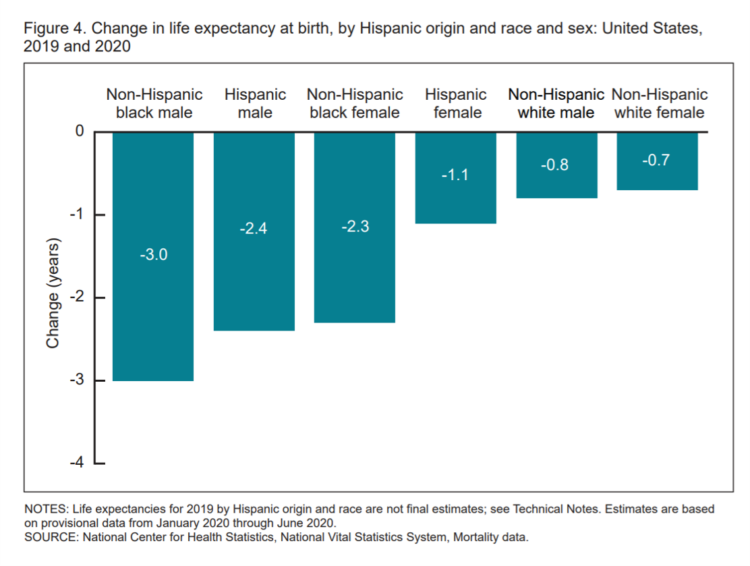
Some people remark about 2020 being a “lost year” in the wake of the coronavirus pandemic. That happens to be a true statement, sadly not in jest: in the U.S., life expectancy at birth fell by one full year over the first half of 2020 compared with 2019, to 77.8 years. In 2019, life expectancy at birth was 78.8 years, according to data shared by the National Center for Health Statistics (NCHS), part of the Centers for Disease Control and Prevention (CDC). Life expectancy at birth declined for both females and males, shown in the first chart. The differences between
The Social Determinants of Prescription Drugs – A View From CoverMyMeds
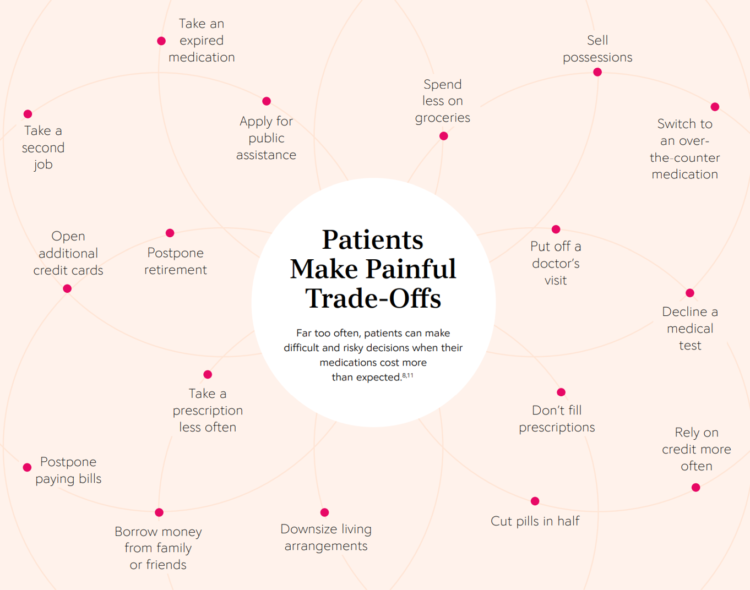
The COVID-19 pandemic forced consumers to define what were basic or essential needs to them; for most people, those items have been hygiene products, food, and connectivity to the Internet. There’s another good that’s essential to people who are patients: prescription drugs. A new report from CoverMyMeds details the current state of medication access weaving together key health care industry and consumer data. The reality even before the coronavirus crisis emerged in early 2020 was that U.S. patients were already making painful trade-offs, some of which are illustrated in the first chart from the report. These include self-rationing prescription drug
Three in Four People Avoiding Health Care in the Pandemic Have Had Chronic Conditions
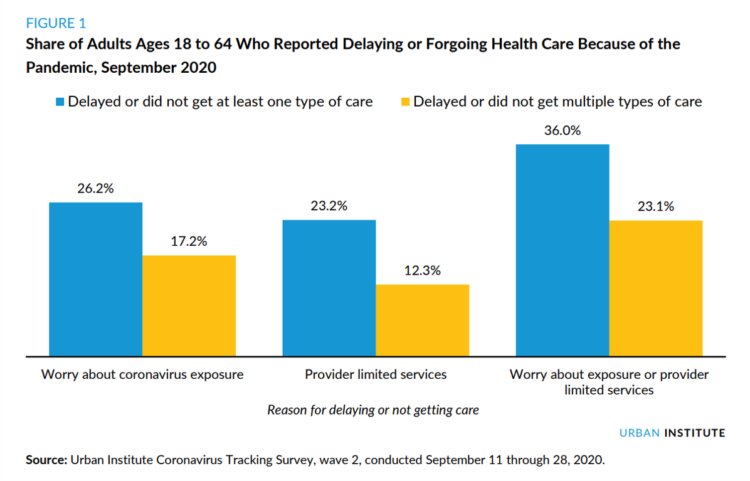
By the autumn of 2020, U.S. physicians grew concerned that patients who were avoiding visits to doctor’s offices were missing care for chronic conditions, discussed in in Delayed and Forgone Health Care for Nonelderly Adults during the COVID-19 Pandemic from the Urban Institute. More than three-fourths of people who delayed or forewent care had at least one chronic health condition. The pandemic may have led to excess deaths from diabetes, dementia, hypertension, heart disease, and stroke, as well as record drug overdoses in the 12 months ending in May 2020. In their JAMA editorial on these data, Dr. Bauchner and
Most Americans Want a Vaccine, Dissatisfied with the Rollout
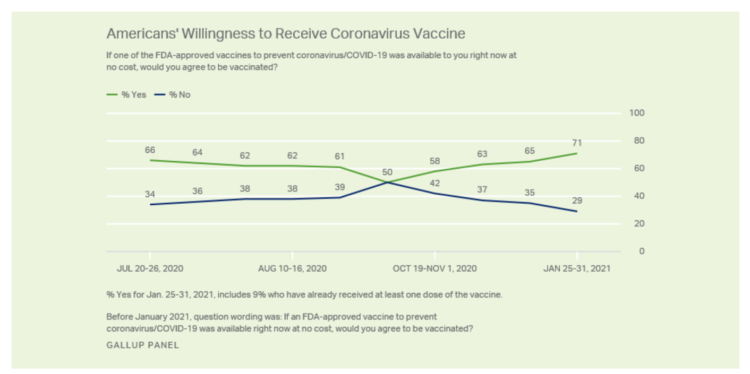
Seven in 10 U.S. adults are willing to be vaccinated, and they’re not happy about the process in getting their jab, according to Gallup’s poll taken in the last week of January 2021. The proportion of Americans willing to receive a COVID-19 vaccine has steadily grown since October 2020, which fell to a mere 50% of folks keen to get the shot. That percentage has risen to 71% as of February 1 2021, as the first line chart shows the reversal in public embrace for vaccination against the coronavirus. Now that most people in the U.S. welcome the opportunity to
Ten In Ten: Manatt’s Healthcare Priorities to 2031

The coronavirus pandemic has exposed major weaknesses in the U.S. health care system, especially laying bare inequities and inertia in American health care, explained in The Progress We Need: Ten Health Care Imperatives for the Decade Ahead from Manatt Health. The report details the ten objectives that are central to Manatt’s health care practice, a sort of team manifesto call-to-action and North Star for the next decade. Their ten must-do’s for bending the cost curve while driving constructive change for a better health care system are to: Ensure access Achieve health equity Stability the safety net and rebuild public health
Americans A Year Into the Pandemic – A View from Pew
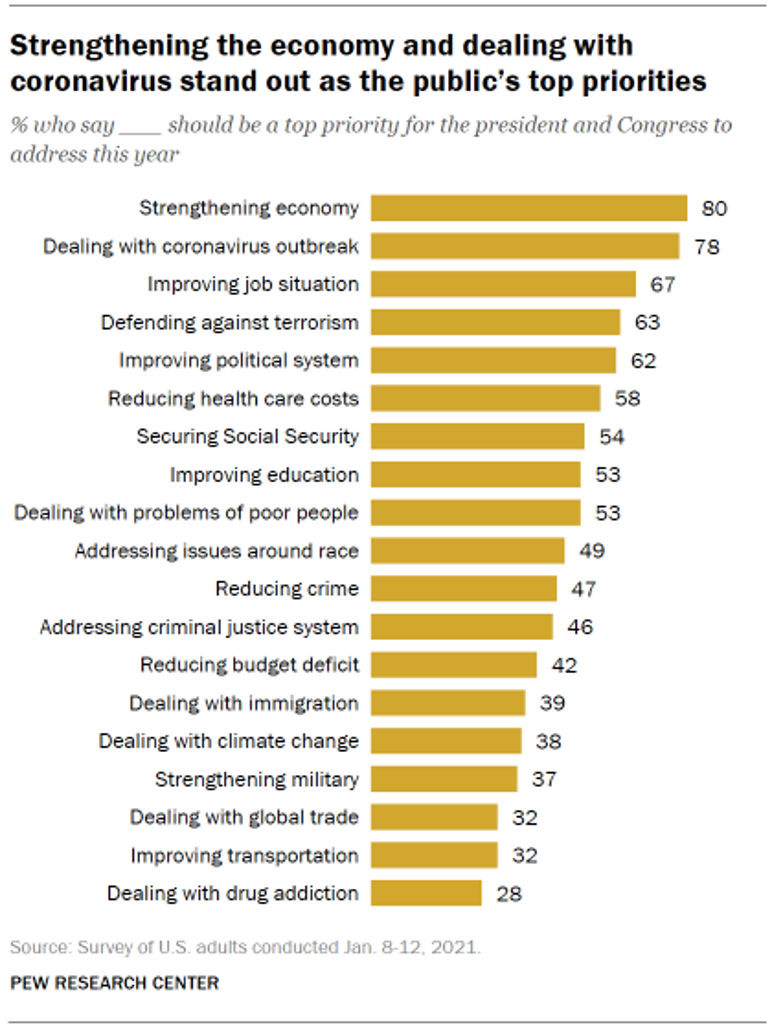
Nearly a year into the COVID-19 pandemic, the same percent of Americans say strengthening the U.S. economy and dealing with the coronavirus outbreak should be a top priority for President Biden and Congress to address this year, according to data from the Pew Research Center collected during the second week of January 2021. Two-thirds of people in the U.S. also want government leaders to prioritize improving the employment situation, defending against terrorism, and improving the political system, the study learned. At Americans’ low end of the priority list for the President and Congress are dealing with global trade, improving transportation,
Food Trends and Hunger in the Pandemic – the Importance of Food Security in Health and Economic Security
In 2020, the COVID-19 pandemic changed all kinds of aspects of our daily lives, not the least of which were our food habits — how we shopped for food, how we bought food, how we cooked and baked from scratch, and how our tastes and nutritional choices changed with our #StayHome and #WorkFromHome lifestyles. People who could keep their jobs and work from home connected by broadband learned how to build up pandemic pantries, shop online, and stay well-fed. But for people in the U.S. who lost employment, had hours cut, or were compelled to stay home to teach kids
The Biden Administration’s Whole-of-Government Approach to Equity – in Health and Beyond
In the U.S., the COVID-19 pandemic has revealed disparities in housing, food, and job security, and the role that one’s ZIP code and social determinants play in health outcomes. Overall, America has done poorly in light of being 4% of the world’s population but having one-fifth of the planet’s deaths due to the coronavirus. But these have disproportionately hit non-white people, who are nearly three times as likely to die from COVID-19 than white Americans. I’ve been head-down reviewing the first two days of President Biden’s signing Executive Orders, reading the National Strategy for COVID-19 Response, and inventorying line items
The Digital Consumer, Increasingly Connected to Health Devices; Parks Associates Kicking Off #CES2021

In 2020, the COVID-19 pandemic drove U.S. consumers to increase spending on electronics, notably laptops, smartphones, and desktop computers. But the coronavirus era also saw broadband households spending more on connecting health devices, with 42% of U.S. consumers owning digital health tech compared with 33% in 2015, according to research discussed in Supporting Today’s Connected Consumer from Parks Associates. developed for Sutherland, the digital transformation company. Consumer electronics purchase growth was, “likely driven by new social distancing guidelines brought on by COVID-19, which requires many individuals to work and attend school from home. Among the 26% of US broadband households
“The virus is the boss” — U.S. lives and livelihoods at the beginning of 2021
“The virus is the boss,” Austan Goolsbee, former Chair of the Council of Economic Advisers under President Obama, told Stephanie Ruhle this morning on MSNBC. Goolsbee and Jason Furman, former Chair of Obama’s Council of Economic Advisers, tag-teamed the U.S. economic outlook following today’s news that the U.S. economy lost 140,000 jobs — the greatest job loss since April 2020 in the second month of the pandemic. The 2020-21 economic recession is the first time in U.S. history that a downturn had nothing to do with the economy per se. As Uwe Reinhardt, health economist guru, is whispering in my
The 2021 Health Populi TrendCast – Health Care, Self-Care, and the Rebirth of Love in Public Health

In numerology, the symbolic meaning behind the number “21” is death and re-birth. In tarot cards, 21 is a promise of fulfillment, triumph, and victory. How apropos that feels right now as we say goodbye and good riddance to 2020 and turn the page for a kinder, gentler, healthier New Year. It would be sinful to enter a New Year as challenging as 2021 promises to be without taking the many lessons of our 2020 pandemic life and pain into account. For health care in America, it is a time to re-build and re-imagine a better, more equitable landscape for
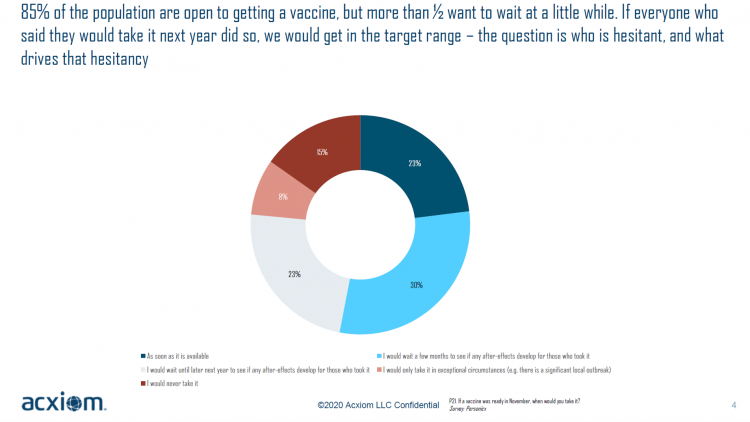
Vaccine Hesitancy Is Greatest Among Those at Highest Risk of Dying from COVID-19: Black People
While 85% of people are open to receiving a COVID-19 vaccine, over one-half of them would want to wait some time to observe if after-effects developed in people who took the jab, according to a new study from Acxiom, the data analytics-marketing company. Not all people are as enthused about getting a coronavirus vaccine at all, Acxiom discovered: in fact, those hardest hit by the virus — Black people — would be the least-likely to want to get a COVID-19 vaccine, discussed in in Vaccine Hesitancy in the U.S., a survey the company conducted among 10,000 people in the U.S.
The COVID Healthcare Consumer – 5 Trends Via The Medecision Liberation Blog
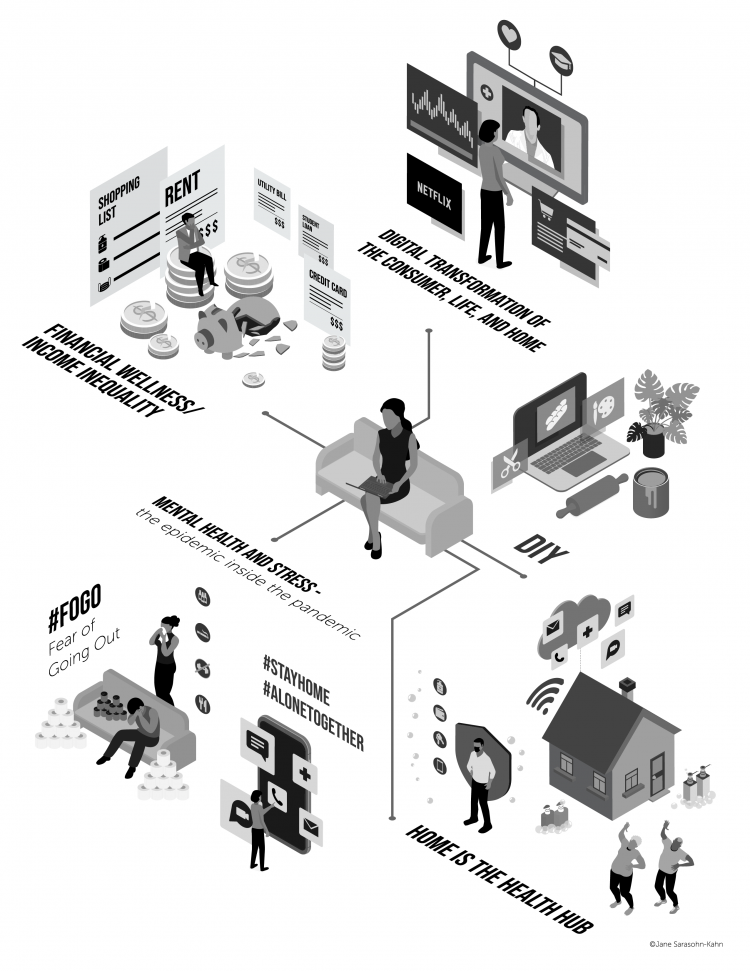
The first six months into the coronavirus pandemic shocked the collective system of U.S. consumers for living, learning, laboring, and loving. I absorbed all kinds of data about consumers in the wake of COVID-19 between March and mid-August 2020, culminating in my book, Health Citizenship: How a virus opened hearts and minds, published in September on Kindle and in print in October. In this little primer, I covered the five trends I woven based on all that data-immersion, following up the question I asked at the end of my previous book, HealthConsuming: when and how would Americans claim their health
The Pandemic Has Been a Shock to Our System – Learning from Known
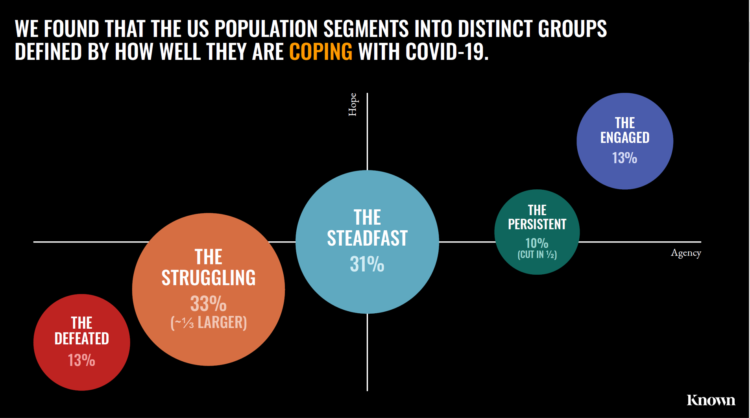
The coronavirus pandemic has been a shock to people across all aspects of everyday living, for older and younger people, for work and school, for entertainment and travel — all impacting our hearts, minds, and wallets. “As the bedrock of daily life was shaken, uncertainty predictably emerged as the prevailing emotion of our time but this universal problem was eliciting a highly differentiated reaction in different people,” Kern Schireson, CEO of Known, observed. His company has conducted a large quantitative and qualitative research program culminating in a first report, The Human Condition 2020: A Shock To The System. Known’s team of
Rebuilding Resilience, Trust, and Health – Deloitte’s Latest on Health Care and Sustainability
The COVID-19 pandemic has accelerated health care providers’ and plans’ investment in digital technologies while reducing capital spending on new physical assets, we learn in Building resilience during the COVID-19 pandemic and beyond from the Deloitte Center for Health Solutions. What must be built (or truly re-built), health care leaders believe, is first and foremost trust, followed by financial viability to ensure long-term resilience and sustainability — for the workforce, the organization, the community, and leaders themselves. For this report, Deloitte interviewed 60 health care chief financial officers to gauge their perspectives during the pandemic looking at the future of
Will We See A Field of Dreams for the COVID-19 Vaccine in the U.S.?
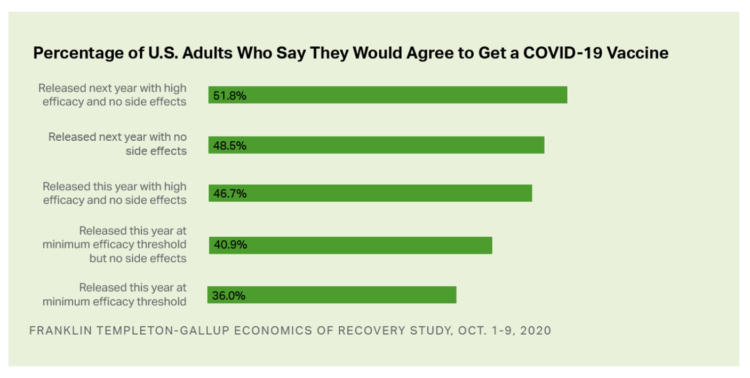
“If you build it, he will come,” the voice of James Earl Jones echoes in our minds when we recall the plotline of the film, Field of Dreams. A quick summary if you don’t know the movie: the “it” was a baseball field to be built in a rural cornfield. The “he” was a baseball player, ultimately joined by a dream-team of ball players who would convene on that dreamy field to play an amazing game. Today, the day after Pfizer announced a 90% benefit for its coronavirus vaccine, bolstering Wall Street returns on 9th November 2020, two new consumer
Voting for Health in 2020

In the 2018 mid-term elections, U.S. voters were driven to polls with health care on their minds. The key issues for health care voters were costs (for care and prescription drugs) and access (read: protecting pre-existing conditions and expanding Medicaid). Issue #2 for 2018 voters was the economy. In 2020, as voting commences in-person tomorrow on 3rd November, U.S. voters have lives and livelihoods on their minds. It’s the pandemic – our physical lives looming largest in the polls – coupled with our fiscal and financial lives. Health is translating across all definitions for U.S. voters in November 2020: for
Women’s Health Policy Advice for the Next Occupant of the White House: Deal With Mental Health, the Pandemic, and Health Care Costs
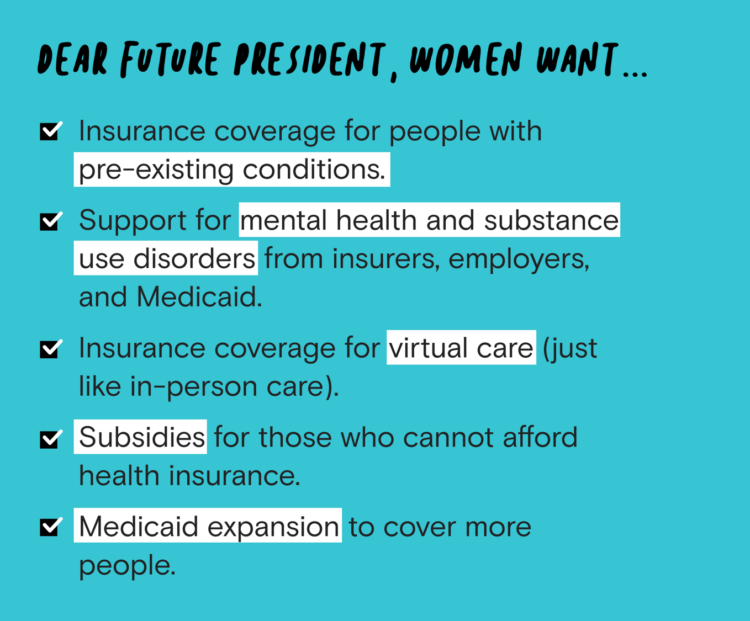
2020 marked the centennial anniversary of the 19th Amendment to the U.S. Constitution, giving women the right to vote. In this auspicious year for women’s voting rights, as COVID-19 emerged in the U.S. in February, women’s labor force participation rate was 58%. Ironic timing indeed: the coronavirus pandemic has been especially harmful to working women’s lives, the Brookings Institution asserted last week in their report in 19A: The Brookings Gender Equality Series. A new study from Tia, the women’s health services platform, looks deeply into COVID-19’s negative impacts on working-age women and how they would advise the next occupant of
Black Health Should Matter More in America: The Undefeated Survey on Race and Health
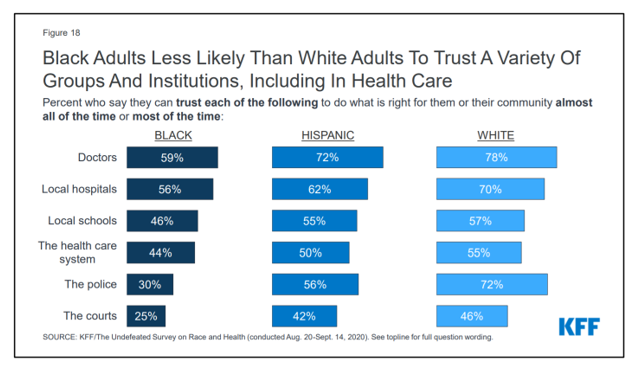
In 2020, most Black people, men and women alike, feel it is a bad time to be Black in America. More than twice as many Black men believed that in 2020 compared with 2006. More than four times as many Black women believed that it’s a bad time to be Black in America in 2020 versus 2011, we learn in The Undefeated Survey on Race and Health from Kaiser Family Foundation (KFF). KFF collaborated with The Undefeated, ESPN’s project that focuses on sports, race, and culture. The Undefeated program was started in May 2016, and has become a thought leader
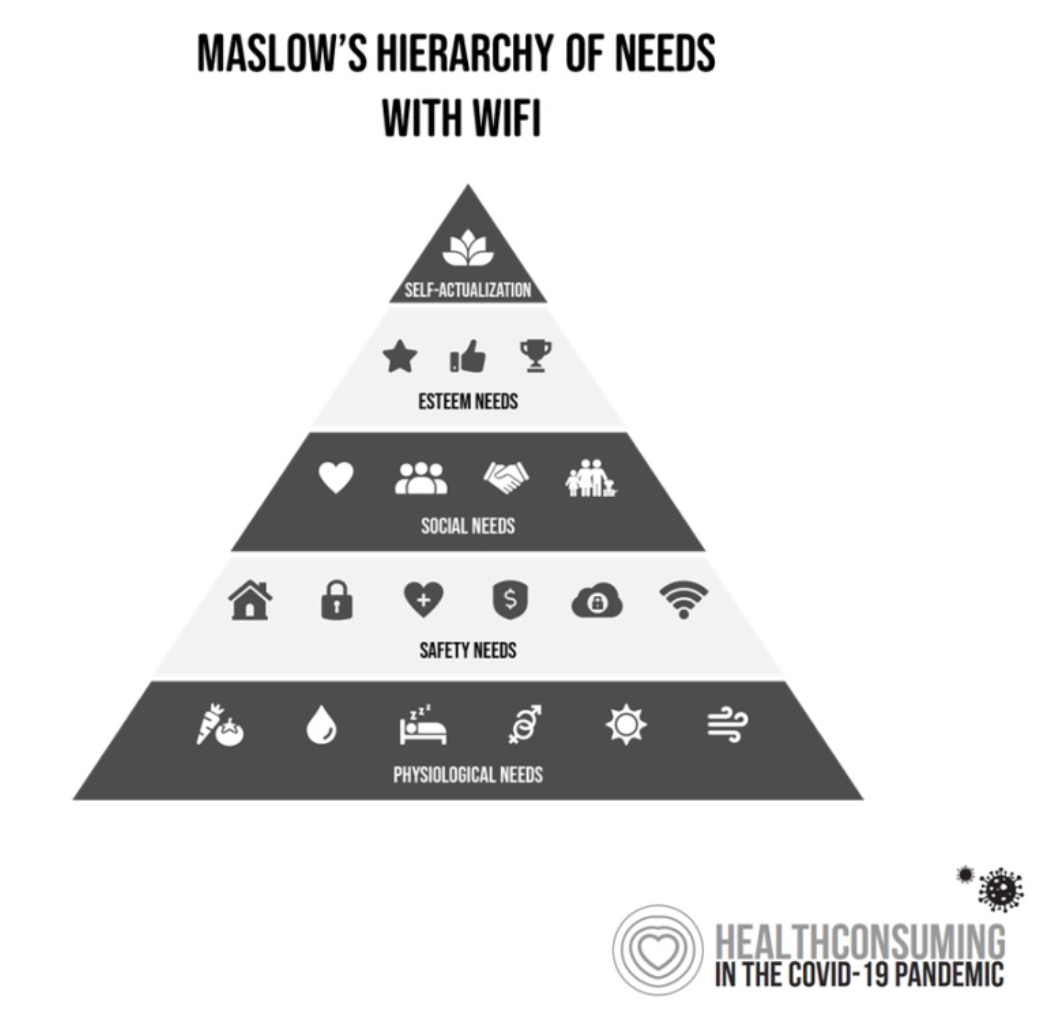
Our Home Is Our Health Hub: CTA and CHI Align to Address Digital and Health Equity

In the pandemic, I’ve been weaving together data to better understand how people as consumers are being re-shaped in daily life across their Maslow Hierarchies of Needs. One of those basic needs has been digital connectivity. People of color have faced many disparities in the wake of the pandemic: the virus itself, exacting greater rates of mortality and morbidity being the most obvious, dramatic inequity. Another has been digital inequity. Black people have had a more difficult time paying for phone and Internet connections during the COVID-19 crisis, we learned in a Morning Consult poll fielded in June 2020. In
Redefining PPE As Primary Care, Public Health, and Health Equity – The Community PPE Index
In May 2020, the Oxford English Dictionary (OED) re-visited the acronym, “PPE.” As OED evolves the definition of PPE, the wordsmiths could borrow from OSHA’s website, noting that PPE, “is equipment worn to minimize exposure to hazards that cause serious workplace injuries and illnesses. These injuries and illnesses may result from contact with chemical, radiological, physical, electrical, mechanical, or other workplace hazards. Personal protective equipment may include items such as gloves, safety glasses and shoes, earplugs or muffs, hard hats, respirators, or coveralls, vests and full body suits.” Perhaps Definition 3 in the OED could be updated by a blog
Health Citizenship in America. If Not Now, When?
On February 4th, 2020, in a hospital in northern California, the first known inpatient diagnosed with COVID-19 died. On March 11th, the World Health Organization called the growing prevalence of the coronavirus a “pandemic.” On May 25th, George Floyd, a 46-year-old Black man, died at the hands of police in Minneapolis. This summer, the Dixie Chicks dropped the “Dixie” from their name, and NASCAR cancelled the confederate flag from their tracks. Today, nearly 200,000 Americans have died due to the novel coronavirus. My new book, Health Citizenship: How a virus opened hearts and minds, launched this week. In it, I
Only in America: The Loss of Health Insurance as a Toxic Financial Side Effect of the COVID-19 Pandemic

In terms of income, U.S. households entered 2020 in the best financial shape they’d been in years, based on new Census data released earlier this week. However, the U.S. Census Bureau found that the level of health insurance enrollment fell by 1 million people in 2019, with about 30 million Americans not covered by health insurance. In fact, the number of uninsured Americans rose by 2 million people in 2018, and by 1.9 million people in 2017. The coronavirus pandemic has only exacerbated the erosion of the health insured population. What havoc a pandemic can do to minds, bodies, souls, and wallets. By September 2020,
Americans Worry About Medical Bankruptcy, As Prescription Drug Costs Play Into Voters’ Concerns
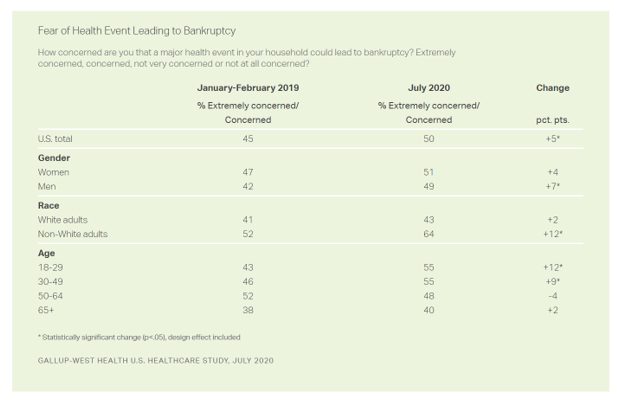
One in two people in the U.S. are concerned that a major health event in their family would lead to bankruptcy, up 5 percent points over the past eighteen months. In a poll conducted with West Health, Gallup found that more younger people are concerned about medical debt risks, along with more non-white adults, published in their study report, 50% in U.S. Fear Bankruptcy Due to Major Health Event. The survey was fielded in July 2020 among 1,007 U.S. adults 18 and older. One of the basic questions in studies like these is whether a consumer could cover a $500
Behavioral Health Side-Effects in the COVID Era
“This surge of people experiencing acute behavioral health problems…has the potential to further impact the healthcare system for years to come,” a report from McKinsey expects looking at the hidden costs of COVID-19’s impact on U.S. health care. The coronavirus pandemic has taken a toll on Americans’ mental health, with anxiety and depression growing as a side-effect to worries about the virus itself, the long Great Lockdown in much of the country, and the economic recession that has particularly impacted women and people of color. I covered depression impacts due to COVID-19 here in Health Populi yesterday, and wanted to
The Racial Divide Due to COVID-19 Also Applies to Healthcare and Pharma Costs
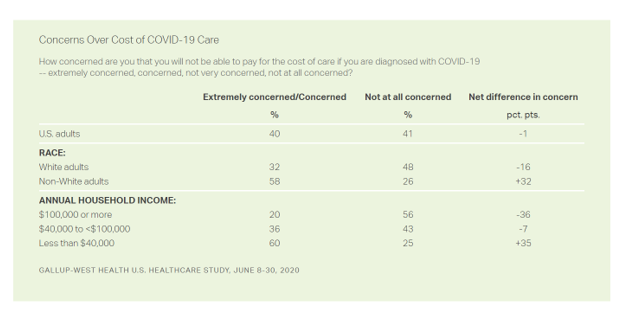
Into the sixth month of the coronavirus pandemic in the U.S., it’s clear that COVID-19 has wreaked a greater mortality and morbidity impact on people of color than on white adults. A new Gallup-West Health poll found that the coronavirus also concerns more non-white Americans than whites when it comes to the cost of health care and medicines to deal with the effects of COVID-19. Considering the cost of COVID-19 treatment, across all U.S. adults, 40% of people are concerned (extremely/concerned), and 41% are “not at all concerned.” Broken down by race, there is a stark difference in levels of




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.