In the wake of the pandemic and growing consumer preferences, the hospital-to-home movement is gaining traction among health systems. Amidst bullish forecasts for the promise of hospital-to-home discharges, the ability for many patients to make this migration would be a difficult bridge to cross.
On the promising front, recent studies reviewed through a meta-analysis published in JAMA found that hospital-to-home programs can be clinically and cost-effective for inpatients discharged from hospital. Earlier this year, McKinsey addressed how “Care at Home” ecosystems can reshape the way health systems — and people — envision patient care. This quote comes from the McKinsey analysis.
Along with the potential of the home evolving as a patient, consumer, and caregiver’s health hub come the realities and challenges of peoples’ daily lives: those social (and other) determinants of health (SDoH) and living situations that are real obstacles for many patients’ discharged to home.
These barriers are revealed in research conducted by a team from the University of Michigan (my alma mater) published in JAMA (May 6, 2022), Patient Perspectives on Care Transitions From Hospital to Home.
The overall finding that emerges out of patients’ own observations: that one’s race, age, insurance status, admission diagnosis, and living situation were all associated with completion of physician follow-up — or lack of follow-up.
Patients who reported at least one SDoH concern were less likely to complete a physician follow-up visit post-discharge than patients who reported no SDOH concerns.
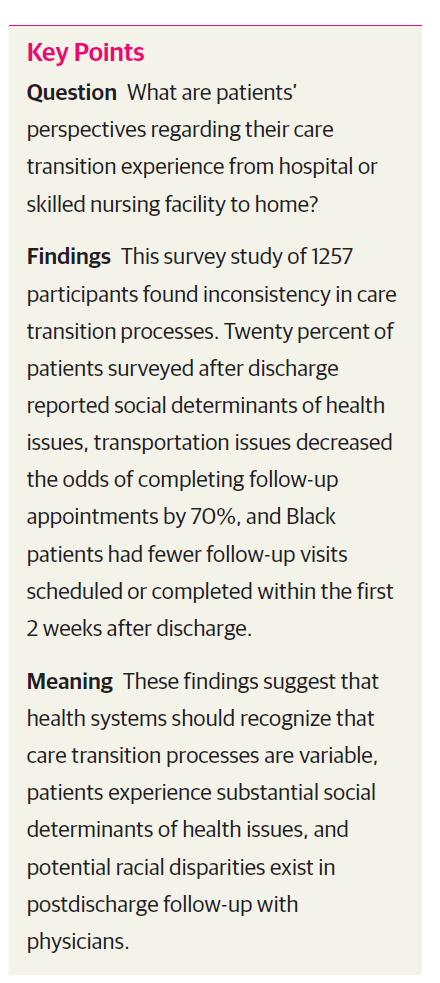
The Key Points chart here from the study summarizes the study learnings.
One of the powerful aspects about this study’s methodology is that the research collected input from patients themsevles — that is, patient-reported outcomes (PROs). While PROs can be criticized for skewing individual expectations, listening to patients is key to informing design of care that’s person-centered, aligning with peoples’ values and beliefs.
Thus in addition to the typical demographic categories such as race, sex, age, chief medical condition, and insurance type, the study codified the patient’s living situation (alone, with others) and SDoH factors such as ability to afford medications, medical visits, basic needs, transportation access, and help at home.
Furthermore, researchers asked whether the patient was able to take meds as prescribed, was prepared to go home, was confident using medical equipment, and whether they spoke with their physician about personal health goals, among other personal considerations not generally collected in studies on discharges to home.
Based on these data, the research found that one in five patients reported at least one SDoH concern; most commonly, these were affording components of care (medications, equipment, PT, home health), access to transportation for physician appointments, affording visits and copayments, and having enough help at home to care for oneself.
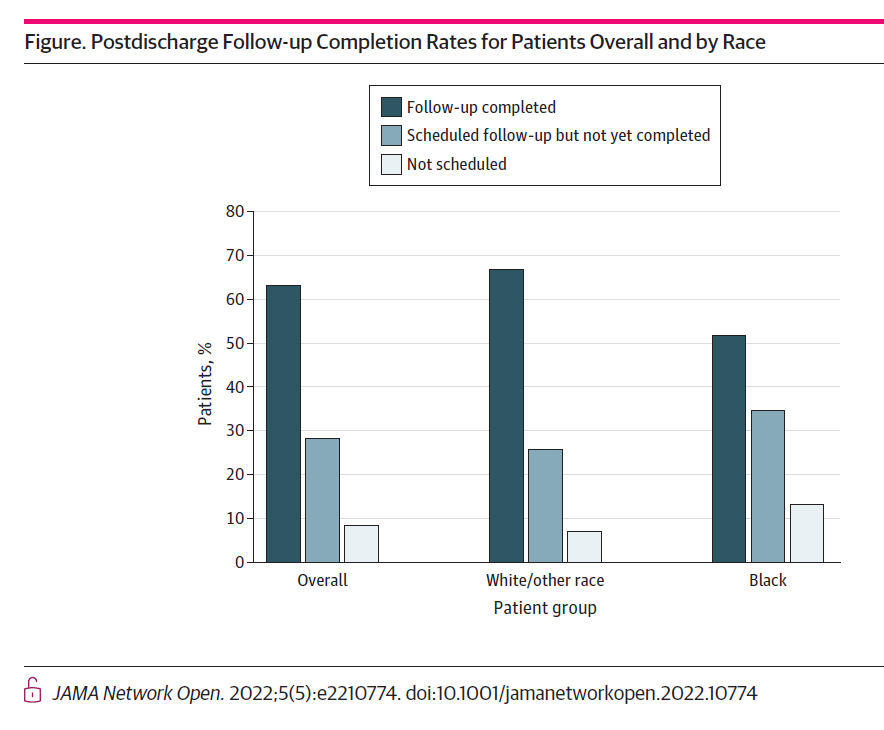
More granularly, here is a finding that illustrates the disparity between patients by race: compared with White patients, Black patients were less likely to complete their post-discharge follow-up visit with their physician, more likely to schedule the visit but not complete it, and more likely to not have scheduled that follow-up visit, shown in the bar chart from the JAMA report.
Doubling-down on the issue of disparities exacerbated by digital health technology, Boston-based researchers published their view on Telehealth’s Double-Edged Sword: Bridging or Perpetuating Health Inequities in the Journal of General Internal Medicine in March 2022.
“Today, anyone can access care by walking into an emergency room,” they observed, “but when it comes to telehealth, patients have to use a number of proprietary portals and platforms that are health system specific. During the pandemic, patients had to learn multiple technology platforms ranging from commercial off-the-shelf platorms such as Zoom to EHR portal-connected telehealth systems….Health systems must invest in capabilities for training patients, family members, and healthcare teams to use these technologies,” the authors recommend.

Health Populi’s Hot Points: One of the limiting factors to taking advantage of hospital-to-home discharge is the reality that some patients do not have a home living situation that can support the transition and tasks required to support the ailing person at home.
Enter Archangels, whose mission is to recognize and lift up caregivers — long unpaid, and to be sure, unseen.
“Caring for a loved one is an honor – it’s also incredibly hard. For the 43% of us in the role of unpaid caregiver, 70% have at least one significant mental health impact,” Alexandra Drane, founder of Archangels, pointed out in an email to me.
Those mental health impacts were anxiety, depression, or suicidal ideation, found in Archangels’ research done in collaboration with the CDC culminating in the team’s landmark study revealing an epidemic of caregiver stress that worsened during the COVID-19 pandemic.
The report assessed mental health among 10,444 parents of children under 18 years of age and unpaid caregivers of adults during the pandemic, December 2020 and February-March 2021. Two of the report’s stunning key findings were that,
- The caregivers (both parents of children and caregivers of adults) had significantly worse mental health than adults not in these roles — notably, five times the odds of any adverse mental health symptoms, and.
- Parents and caregivers, especially those balancing roles as both parents and caregivers, experienced higher levels of adverse mental health symptoms during the COVID-19 pandemic than adults without these responsibilities.
“We need to start respecting and accounting for unpaid caregivers. Any and all of us serving in this role need to be included at every point of the care equation. We need a ‘New Checklist’ at the point of discharge,” Alex recommended, a call-to-action which comports well with the JAMA research discussed above.
Archangels has developed a Caregiver Intensity Score that enables us to calculate just how stressed we are in our roles taking care of loved ones. Click here to get your score, or share with those you know how may be caregiving and, potentially, at-risk of burnout.
As this post goes live on 1 June, Alex will be participating in Life Itself, a collaboration hosted by Dr. Sanjay Gupta and Mark Hodesh of TEDMED, bringing together people re-making health and healthcare for the better.
You can read and glean more insights about unpaid caregivers’ mental health and financial stress in this McKinsey interview with Alex, and watch the videos as Alex explains how to spot the “red light” of intensity and lift up caregivers so people can heal at home…and their loving caregivers be supported along their care journeys….




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...