In 2021, racial and ethnic disparities in healthcare are a top patient safety issue, according to ECRI’s annual list of major concerns facing healthcare consumers’ risks to adverse events that can harm them.
 ECRI has published their annual Top 10 list since 2018, when the list featured diagnostic errors, o behavioral health needs in acute care settings, and patient engagement and health literacy — all of which play into this year’s #1 issue, racial and ethnic disparities in health care.
ECRI has published their annual Top 10 list since 2018, when the list featured diagnostic errors, o behavioral health needs in acute care settings, and patient engagement and health literacy — all of which play into this year’s #1 issue, racial and ethnic disparities in health care.
In fact, among the risks in this year’s Top Ten list, eight were accelerated and highlighted by the COVID-19 pandemic (the two un-related to the coronavirus crisis were methotrexate therapy and peripheral vascular harm).
“By learning lessons from the pandemic,” ECRI explains in their report, “we can improve safety not just for this and future pandemics, but for all patient and resident care.”
 In discussing racial and ethnic disparities in health care, ECRI quotes Dr. Joia Crear-Perry, who noted,
In discussing racial and ethnic disparities in health care, ECRI quotes Dr. Joia Crear-Perry, who noted,
“The experiences of people of color in our health systems reveal that implicit and explicit bias and structural racism are driving health inequities like maternal mortality.”
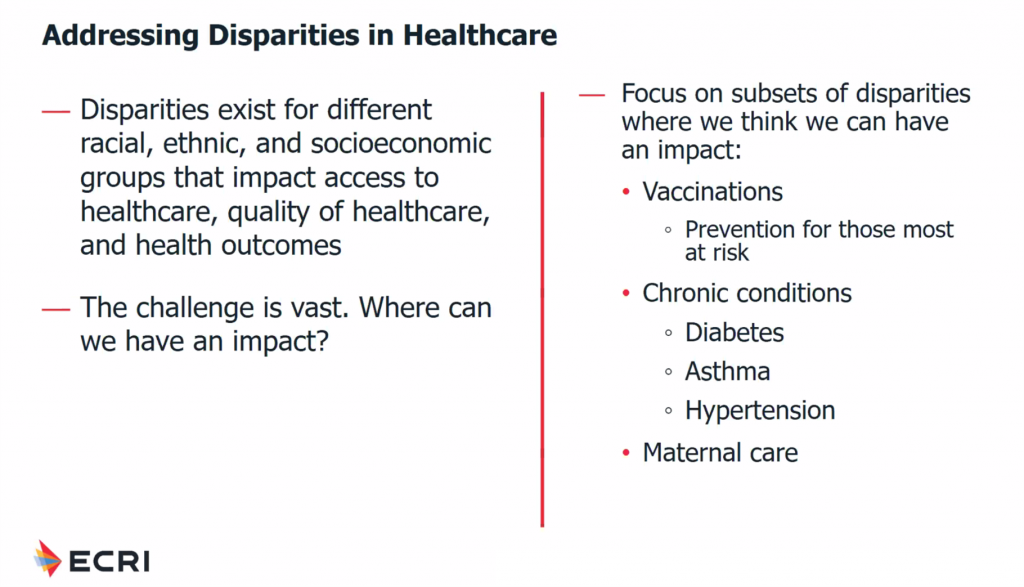
Maternal mortality is over 3 times higher among Black mothers compared with White mothers. This is one of several disparity challenges ECRI points out in as one of several areas that health systems can directly impact, along with vaccinations (with both vaccine hesitancy and trust barriers combined with supply access obstacles), and chronic conditions such as diabetes, asthma, and hypertension.
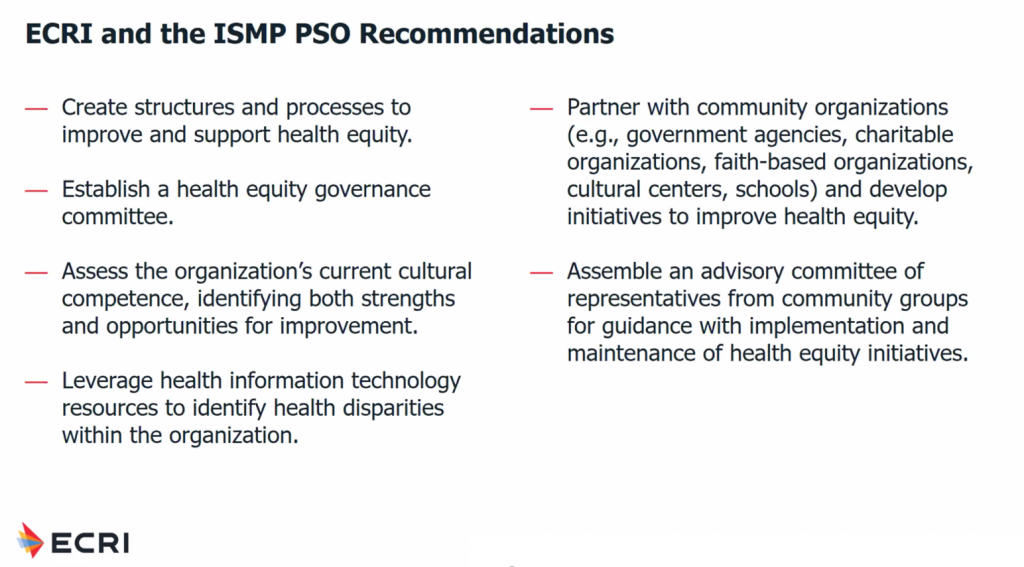 ECRI offers several recommendations and action-prescriptions for health systems to address racial disparities from a patient safety impact. These include:
ECRI offers several recommendations and action-prescriptions for health systems to address racial disparities from a patient safety impact. These include:
- Embed health equity into the organization’s strategy, structures and processes – and allocate resources to these work-flows
- Leverage health IT to identify disparities
- Partner with community organizations to develop initiatives baked with trust for communities
- Assemble an advisory committee of representatives from community groups to guide implementation and development of health equity programs
- Address institutional racism within the organization and recruit health care workers from under-represented groups
- Develop providers’ cultural competence through, say, educational programs, among other tactics.
 Health Populi’s Hot Points: In a wonderful interview with Mike Miliard in Healthcare IT News, the Biden Administration’s National Health IT Coordinator Micky Tripathi talks about his priorities for leading ONCHIT. After the immediate priority of dealing with interoperability and data to address the coronavirus pandemic, Micky talked about the weaknesses that COVID-19 revealed about U.S. health care — especially expressed by health disparities.
Health Populi’s Hot Points: In a wonderful interview with Mike Miliard in Healthcare IT News, the Biden Administration’s National Health IT Coordinator Micky Tripathi talks about his priorities for leading ONCHIT. After the immediate priority of dealing with interoperability and data to address the coronavirus pandemic, Micky talked about the weaknesses that COVID-19 revealed about U.S. health care — especially expressed by health disparities.
He explained his vision of “health equity by design.”
Mike writes in Healthcare IT News,
As he [Tripathi] explained it, health IT policymakers have often, in many areas “embraced technology and moved forward with standards and processes that didn’t explicitly take into account the consequences that our actions and activities might have on health equity. And then you catch up later, and you sort of do some measurement, and you realize, ‘Oh wow, this created some health disparities we didn’t realize, and now we have to go back and rectify and mitigate.’….What I think we all need to work on and move toward – and certainly within the ONC, we’re doing our best to do this – is thinking about health equity by design.”
Dr. Winston Wong and colleagues wrote an essay in JAMA in April 2015 called Achieving Health Equity by Design. In this viewpoint, the team called out health disparities by race and ethnicity, recommending that to design services that promote health equity, there must be a “clear focus on specific communities at risk, a commitment to listen and collect meaningful data to understand local needs and priorities, a conviction to make progress, and ongoing assessment of health outcomes.”
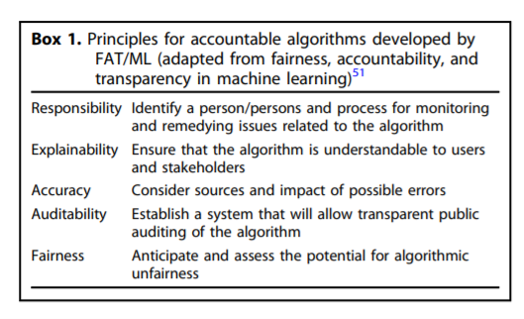 Part of that data collection in today’s world involves AI-enabled decision support tools, which Tripathi talked about in his interview. He pointed to the potential for algorithmic bias, of which we should all be mindful to avoid and identify.
Part of that data collection in today’s world involves AI-enabled decision support tools, which Tripathi talked about in his interview. He pointed to the potential for algorithmic bias, of which we should all be mindful to avoid and identify.
In closing the loop on racial/ethnic disparities as a patient safety issue and health equity by design, I’ll point you to a recent article in Nature Digital Medicine titled “Predictably unequal.” Here, Dr. Jessica Paulus and Dr. David Kent of Tufts University explain how algorithms can increase health disparities. They propose a framework to reduce that risk of making a decades-long problem, health inequities, worse in the AI era. The key principles are responsibility, explainability, accuracy, auditability, and fairness.
Those sound like great pillars on which health care for everyone would benefit.





 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...