The Real Face of Men’s Health in America: Years of Life Lost, Yearning for Social Connection, and Eroding Trust in Health Care
In 2023, more than one-half of male deaths in the U.S. were premature: this is The Real Face of Men’s Health in America, a new report analyzing 2025 U.S. data from the Movember Foundation. The report was published as we approach November which the project chose for Men’s Health Month when launching in Australia over 20 years ago. Compared with the rest of the economically-developed world, Movember found that the “U.S. stands out for the sheer number of years of life lost (YLL), as well as the enormous toll of men’s early deaths
There’s a Health Gap for Women Around the World – and the World Economic Forum Has a Blueprint to Fix It
Even though women comprise one-half of the world’s population, their health outcomes and inputs do not match up to men’s: there’s a women’s health gap on Planet Earth. Meeting in Davos this week for #WEF2025, the World Economic Forum published a report on that gender-health chasm titled, Blueprint to Close the Women’s Health Gap: How to Improve Lives and Economies for All. In collaboration with the McKinsey Health Institute, the report focuses on nine key conditions that, if addressed, could reduce the global disease burden by 27 million disability adjusted life years and add
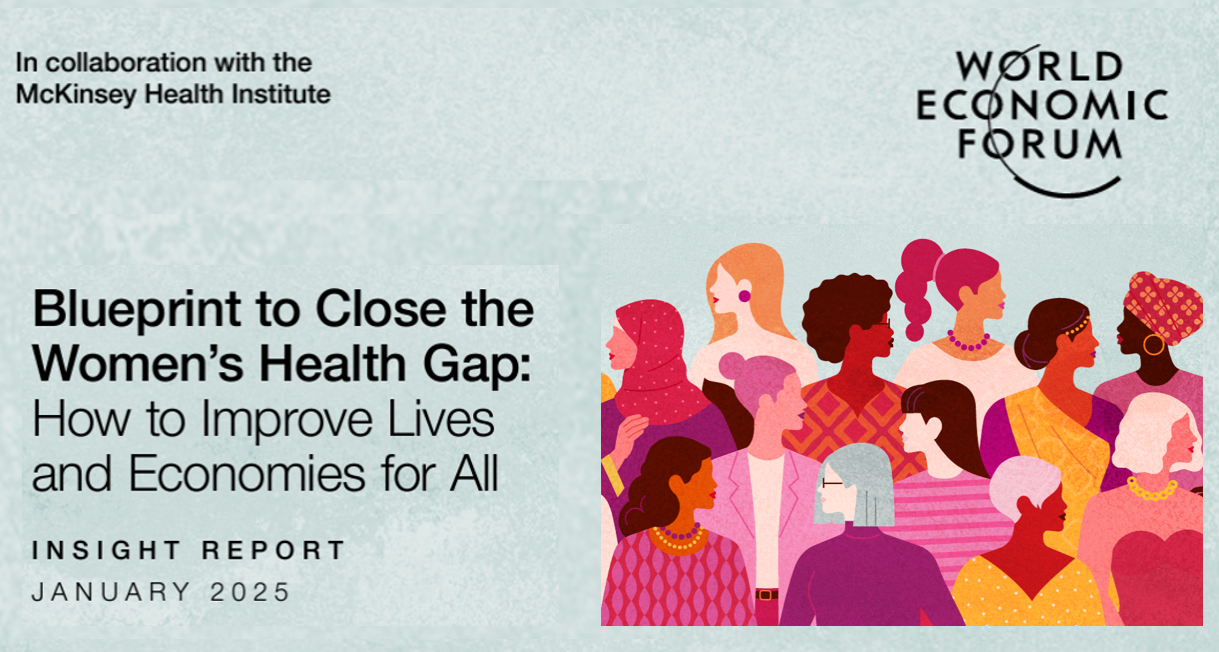
The Impacts of Heat on Health Across All Dimensions – from Death to “Heat-Flation” on the Pocketbook
Rising energy bills are confronting U.S. households (and indeed, health citizens in many parts of the world) due to extreme heat, PBS reported on 1st September. But the record heat waves in so much of the world is impacting both peoples’ fiscal and financial well-being along with physical health impacts, ranging from exacerbating chronic respiratory conditions to, literally, risks to lives. A recent letter to JAMA, published August 26, 2024, quantifies Trends of Heat-Related Deaths in the U.S., 1999-2023. The authors examined studies finding exposure to extreme heat associated with mortality,
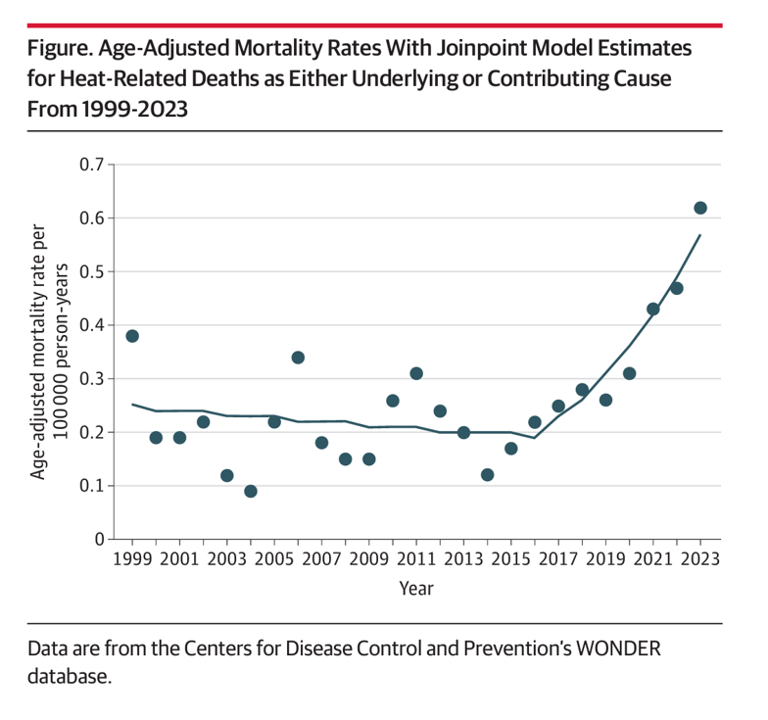
Women’s Health Outcomes in the U.S.: Spending More, Getting (Way) Less – 4 Charts from The Commonwealth Fund
Women in the U.S. have lower life expectancy, greater risks of heart disease, and more likely to face medical bills and self-rationing due to costs, we learn in the latest look into Health Care for Women: How the U.S. Compares Internationally from The Commonwealth Fund. The Fund identified four key conclusions in this global study: Mortality, shown in the first chart which illustrates women in the U.S. having the lowest life expectancy of 80 years versus women in other high-income countries; Health status, with women in the U.S. more likely to consume multiple prescription
Medical Debt, Aflac on Eroding Health Benefits, the CBO’s Uninsured Forecast & Who Pays for Rising Health Care Prices: A Health Consumer Financial Update
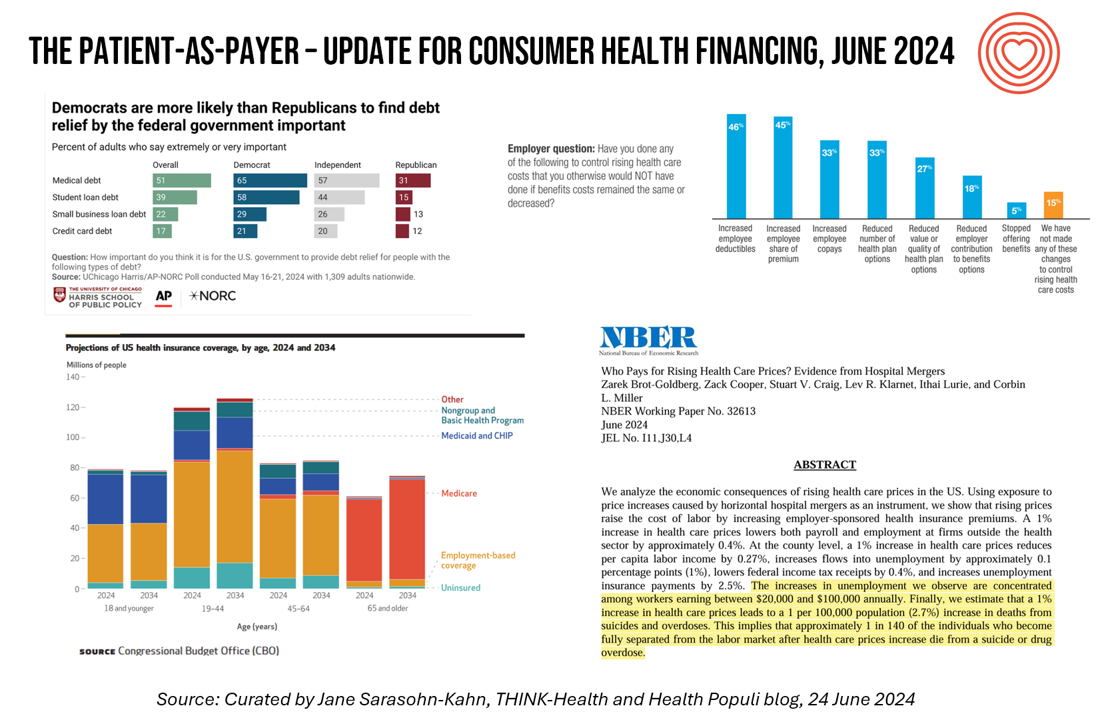
On June 11, Rohit Chopra, the Director of the Consumer Financial Protection Bureau (CFPB) announced the agency’s vision to ban Americans’ medical debt from credit reports. He called out that, “In recent years, however, medical bills became the most common collection item on credit reports. Research from the Consumer Financial Protection Bureau in 2022 showed that medical collections tradelines appeared on 43 million credit reports, and that 58 percent of bills that were in collections and on people’s credit records were medical bills.” Chopra further explained that medical debt on a consumer credit report was quite different than other kinds
Rebel Health: The Personal and Professional Passion of Susannah Fox
A “rebel” is both a noun and a verb. As a noun, Merriam-Webster tells us that a rebel is a person who opposes or takes up arms against a government or a ruler. As a verb, “to rebel” is to oppose or disobey one in authority or control, or otherwise renounce and resist by force the authority of one’s government.” An additional definition of the verb is, “to feel or exhibit anger or revulsion.” If you’ve been a patient facing a diagnosis of an illness, whether rare or common, you may well have felt these various feelings stirring inside your self.
A Public Health Wake-Up Call: Reading Between the Lines in IQVIA’s 2023 Use of Medicines Report
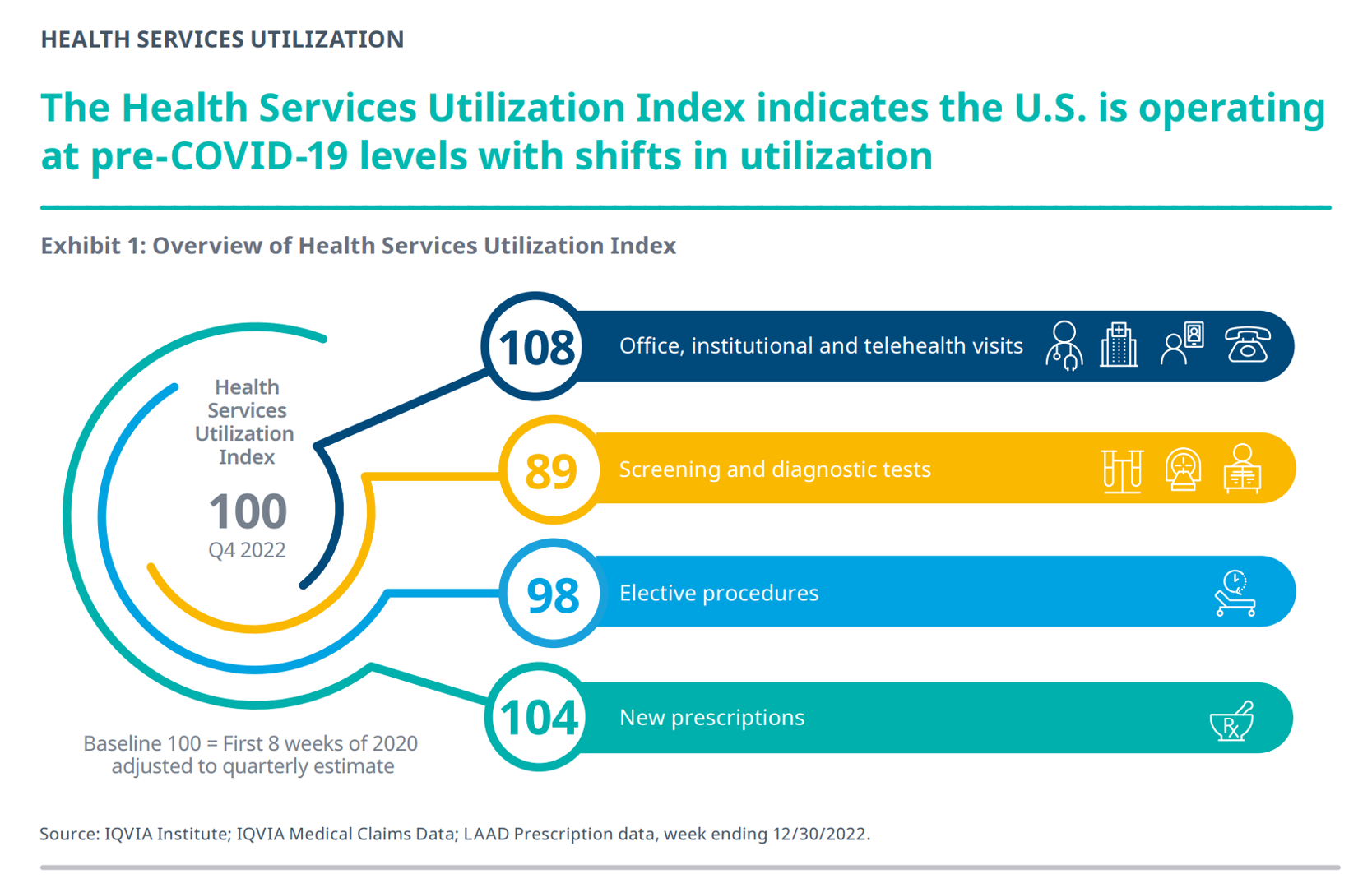
Reviewing the annual 2023 report from the IQVIA Institute for Human Data Science discussing The Use of Medicines in the U.S. is always a detailed, deep, and insightful dive into the state of prescription drugs. It’s a volume speaking volumes on the current picture of prescribed meds, spending and revenues, health care utilization trends, and a forecast looking out to 2027. In my read of this year’s review, I see a flashing light for U.S. health care: “Wake up, public health!” I’ve pulled out a few of the data points that speak to me about population health, prevention and early
The Heart Health Continuum at #CES2023 – From Prevention and Monitoring to Healthy Eating and Sleep
“Are we losing the battle against heart disease?” asks the lead article featured in the January 2023 issue of the AARP Bulletin. “Despite breathtaking medical advancements since President Harry Truman declared war on heart disease 75 years ago, researchers have observed a disturbing trend that started in 2009: America’s death rate from heart-related conditions is climbing again,” the detailed essay explains. AARP is in fact a very visible stakeholder in the 2023 CES, collaborating on the AgeTech content track at the tech conference. The track covers all aspects of aging well, from financial health to entertainment,
How Will the “New” Health Economy Fare in a Macro-Economic Downturn?

What happens to a health care ecosystem when the volume of patients and revenues they generate decline? Add to that scenario a growing consensus for a likely recession in 2023. How would that further impact the micro-economy of health care? A report from Trilliant on the 2022 Trends Shaping the Health Economy helps to inform our response to that question. Start with Sanjula Jain’s bottom-line: that every health care stakeholder will be impacted by reduced yield. That’s the fewer patients, less revenue prediction, based on Trilliant’s 13 trends re-shaping the U.S. health
Life Expectancy Falls in the U.S., the Largest 2-Year Decline in 100 Years
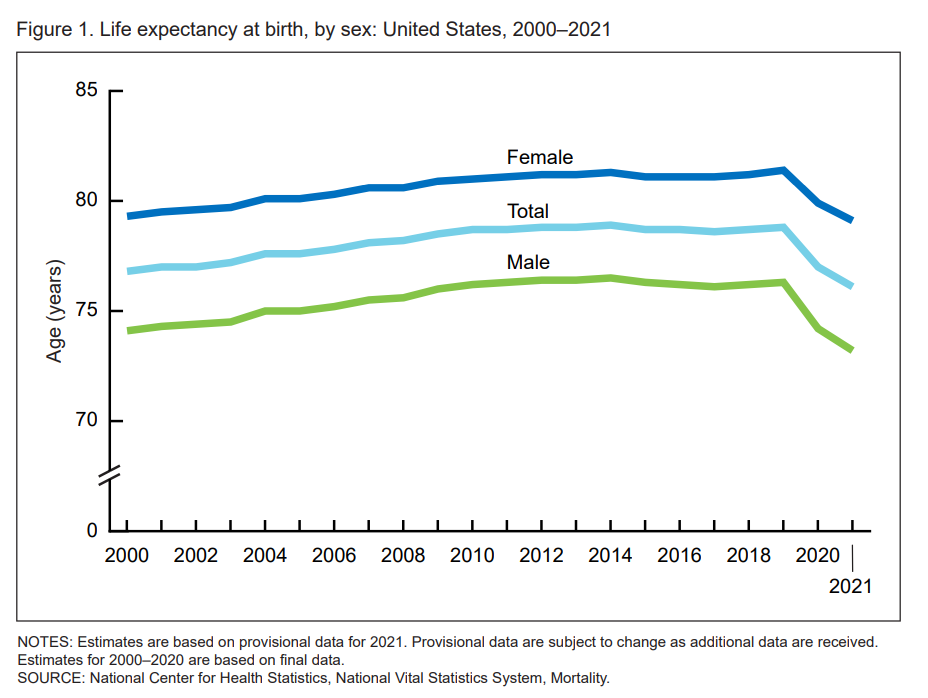
Life expectancy at birth in 2021 in the United States fell to 76.1 years, the lowest level since 1996. Men fared much worse than women, with 73,2 years of life expectancy versus 79.1 years for women, the latest research from the CDC’s National Center for Health Statistics revealed. In their Provisional Life Expectancy Estimates for 2021, the CDC kicks off a demographically detailed analysis with this simple line chart which graphs the dramatic decline in life expectancy at birth. The overall decline across gender and all race/ethnic groups was 2.7 years: 3.1 years
The 2022 US Health System Report Card: Pretty Terrific If You Live in Hawaii or Massachusetts
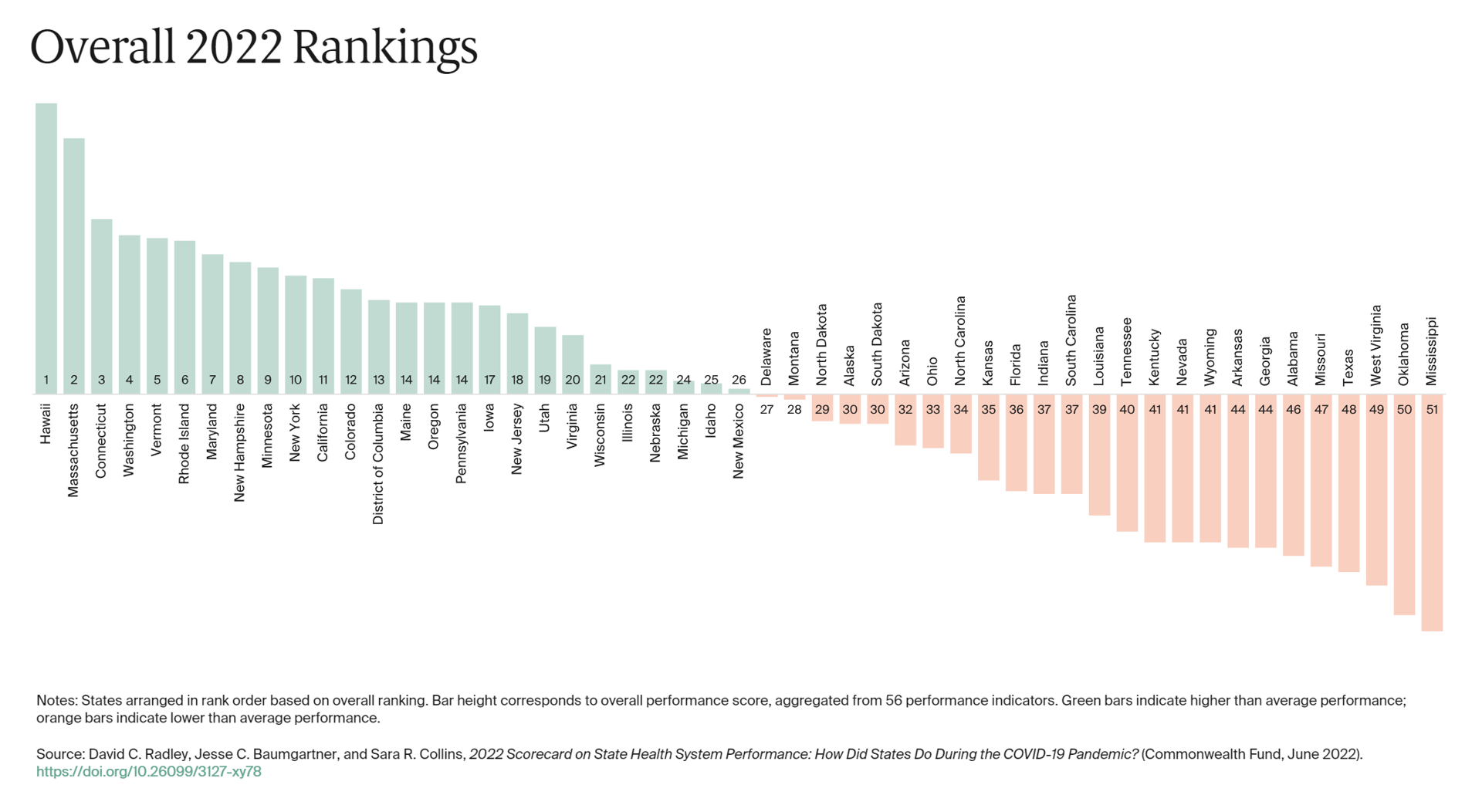
The best U.S. states to live in for health and health care are Hawaii, Massachusetts, Connecticut, Washington, Vermont, Rhode Island, and Maryland… Those are the top health system rankings in the new 2022 Scorecard on State Health System Performance annual report from the Commonwealth Fund. If you live in Mississippi, Oklahoma, West Virginia, Texas, Missouri, Alabama, Georgia, or Arkansas, your health care and outcomes are less likely to be top-notch, the Fund’s research concluded. The Commonwealth Fund has conducted this study since 2006, assessing a range
How Business Can Bolster Determinants of Health: The Marmot Review for Industry

“Until now, focus on….the social determinants of health has been for government and civil society. The private sector has not been involved in the discussion or, worse, has been seen as part of the problem. It is time this changed,” asserts the report, The Business of Health Equity: The Marmot Review for Industry, sponsored by Legal & General in collaboration with University College London (UCL) Institute of Health Equity, led by Sir Michael Marmot. Sir Michael has been researching and writing about social determinants of health and health equity for decades, culminating publications
McKinsey’s Six Shifts To Add Life to Years — and One More to Consider
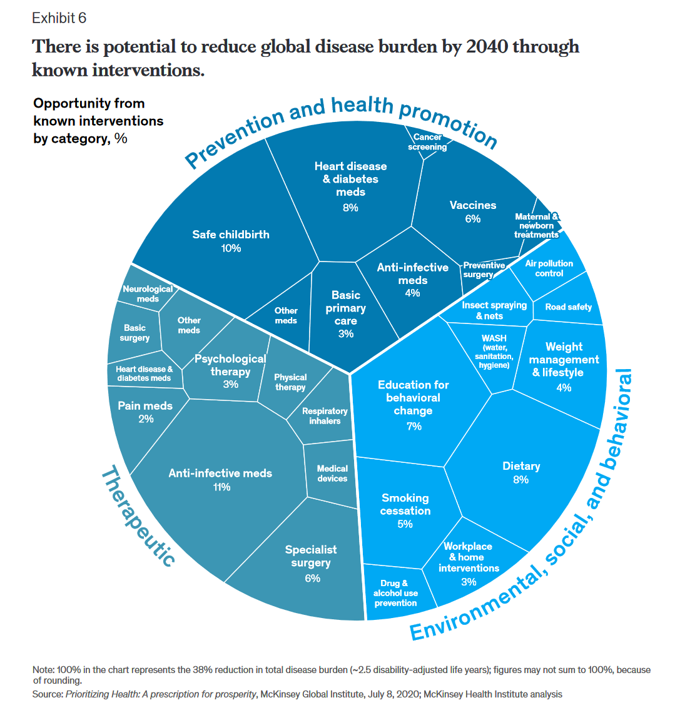
People spend one-half of their lives in “less-than-good health,” we learn early in the paper, Adding years to life and life to years from the McKinsey Health Institute. In this data-rich essay, the McKinsey team at MHI sets out an agenda that could help us add 45 billion extra years of higher-quality life equal to an average of six years per person (depending on your country and population demographics). The first graphic from the report illustrates four dimensions of health and the factors underneath each of them that can bolster or diminish our well-being: personal behaviors (such as sleep and diet),
“We’ve normalized a very high death toll in the U.S.” – How A Trust Deficit Has Infected America’s COVID Outcomes
Trust, or really lack thereof, is a killer app for people’s coronavirus health outcomes. That is the through-line found in a very deep dive into 177 countries’ health data published in The Lancet in a research article on pandemic preparedness and COVID-19. The Lancet study, published on 1 February 2022, was funded by the Gates Foundation in partnership with The Bloomberg Philanthropies et al. The study was researched and written up by a team of COVID-19 National Preparedness Collaborators, led by Dr. Joseph Dieleman of the University of Washington’s Institute for Health Metrics and Evaluation, a group that has been long-tracking
Health Disparities in America: JAMA Talks Structural Racism in U.S. Health Care

“Racial and ethnic inequities in the US health care system have been unremitting since the beginning of the country. In the 19th and 20th centuries, segregated black hospitals were emblematic of separate but unequal health care,” begins the editorial introducing an entire issue of JAMA dedicated to racial and ethnic disparities and inequities in medicine and health care, published August 17, 2021. This is not your typical edition of the Journal of the American Medical Association. The coronavirus pandemic has changed so many aspects of American health care for so many people, including doctors. Since the second quarter of 2020,
Nurses and Aides Are Beloved and Deserve Higher Pay; and a Spotlight on the Filipinx Frontline
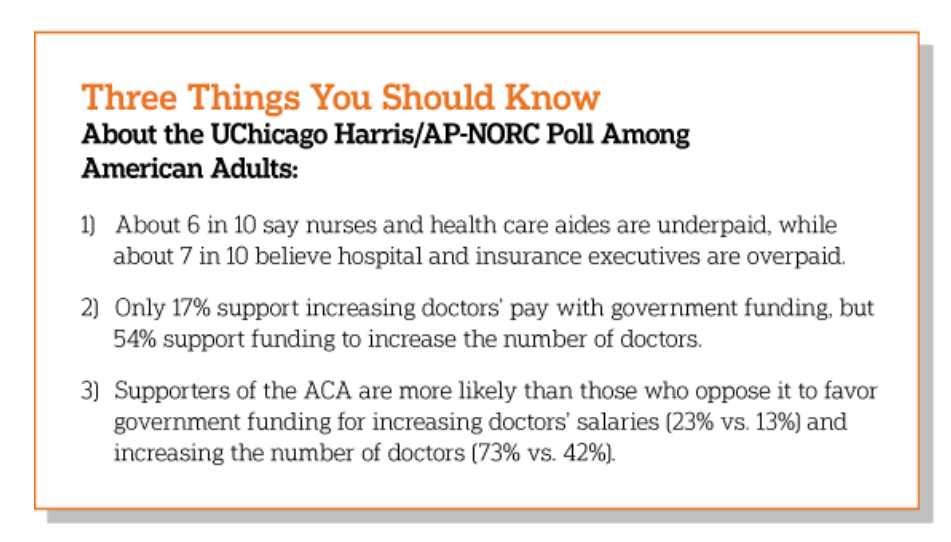
A majority of Democrats, Independents, and Republicans agree that nurses are underpaid. Most Americans across political parties also believe that hospital executives are overpaid, according to a poll from The Associated Press-NORC Center for Public Affairs Research. The survey analysis is aptly titled, Most Americans Agree That Nurses and Aides Are Underpaid, While Few Support Using Federal Dollars to Increase Pay for Doctors, . Insurance executives are also overpaid, according to 73% of Americans — an even higher percent of people than the 68% saying hospital execs make too much money. In addition to nurses being underpaid, 6 in 10
What Poor Birth and Maternity Outcomes in the U.S. Say About American Healthcare & “Infrastructure”
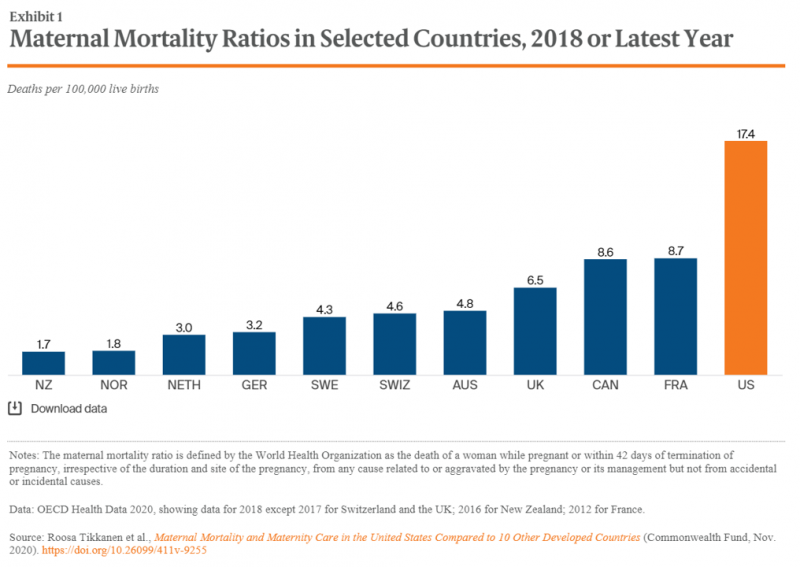
Cain Brothers is a 100+ year old financial services firm with a strong health care experience, now part of KeyBanc. A recent “House Calls” memo and podcast from two company analysts detailed the state of Medicaid, Motherhood and America’s Future: Giving Birth to Better Maternity Outcomes. Christian Pesci and David Johnson’s in-depth discussion detailed their bottom-line that, “maternity care in the U.S. is in crisis but poised for rapid evolution…(recognizing) that an uncoordinated system with misaligned incentives harms too many individuals, families, and communities.” They lay out the crisis as follows: Medicaid funds nearly one-half of births in the U.S.
The Healthiest Communities in the U.S. After the Pandemic – U.S. News & Aetna Foundation’s Post-COVID Lists

Some of America’s least-healthy communities are also those that index greater for vaccine hesitancy and other risks for well-being, found in U.S. News & World Report’s 2021 Healthiest Communities Rankings. U.S. News collaborated with the Aetna Foundation, CVS Health’s philanthropic arm, in this fourth annual list of the top geographies for well-being in the U.S. Six of the top ten healthiest towns in America are located in the state of Colorado. But #1 belongs to Los Alamos County, New Mexico, which also ranked first in ___. Beyond Colorado and New Mexico, we find that Virginia fared well for health in
5.5 Million Years of Life Will Be Lost Due to COVID-19 in the U.S. in 2020
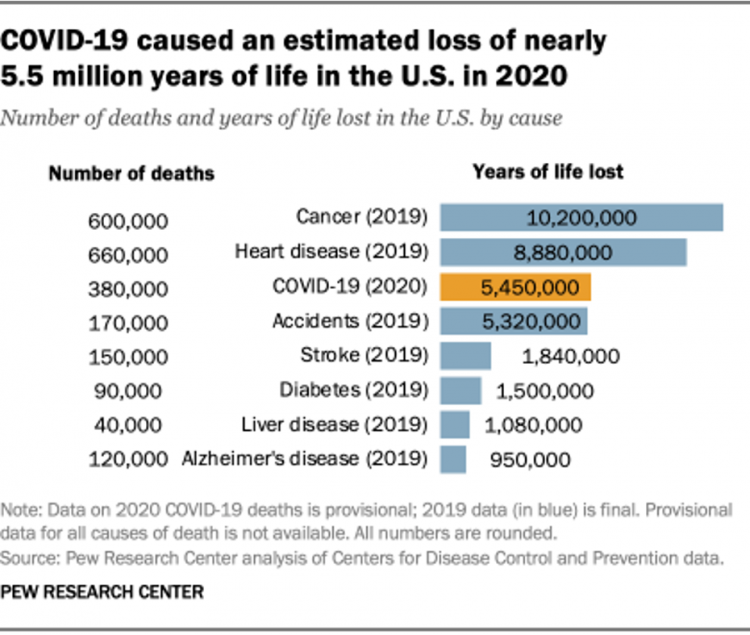
In 2020 in the U.S., 380,000 people are expected to die due to COVID-19. These people lost due to the coronavirus would, collectively, have lived another 5.5 million life-years would they not have succumbed to the virus. COVID-19 has cut lives short relative to their life expectancy, calculated in an analysis by the Pew Research Center based on CDC data from 2019 and 2020, coupled with additional statistics on life expectancy by age and gender. The bottom-line from the Pew Research Center’s analysis, simply stated, is that, “The pandemic…has killed many Americans who otherwise might have expected to live for
Health Disparities and the Risks of Social Determinants for COVID-19 – 14 Months of Evidence
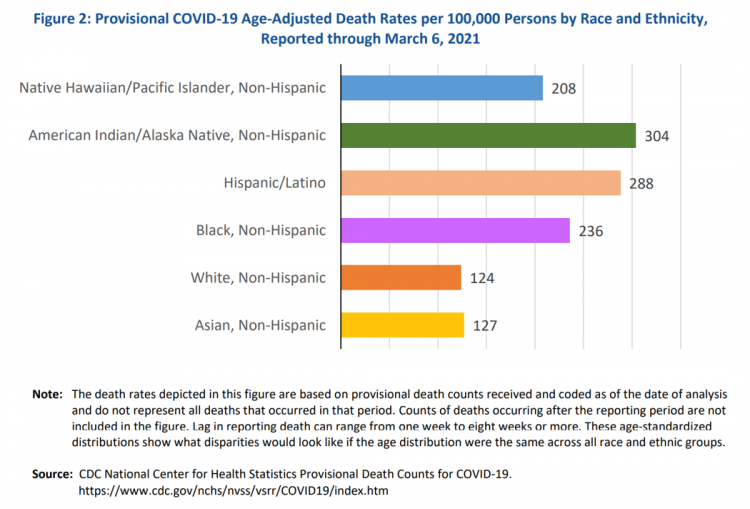
In April 2020, the U.S. Centers for Disease Control issued a report featuring evidence that in the month of March 2020, the coronavirus pandemic was not an equal-opportunity killer. Within just a couple of months of COVID-19 emerging in America, it became clear that health disparities were evident in outcomes due to complications from the coronavirus. An update from that early look at differences in COVID-19 diagnoses and mortality rates was published in Health Disparities by Race and Ethnicity During the COVID-19 Pandemic: Current Evidence and Policy Approaches, In this report, the Assistant Secretary for Planning and Evaluation, part of
The Pandemic’s Death Rate in the U.S.: High Per Capita Income, High Mortality
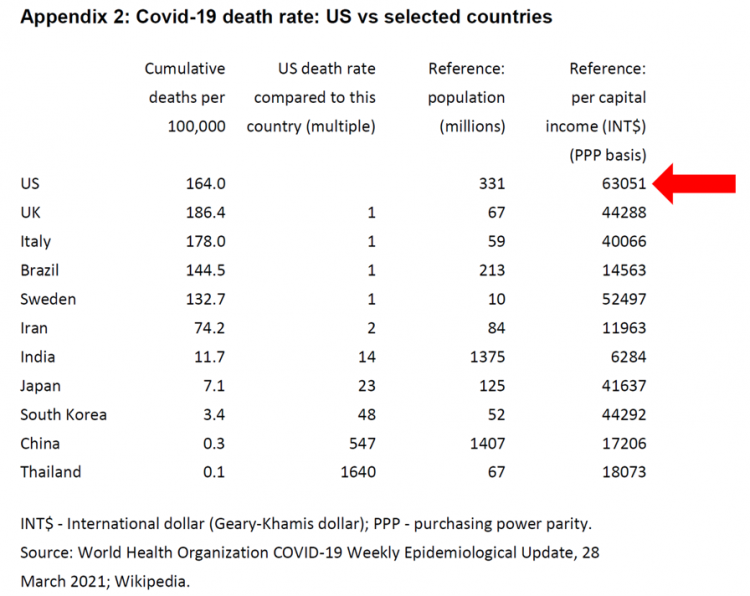
The United States has among the highest per capita incomes in the world. The U.S. also has sustained among the highest death rates per 100,000 people due to COVID-19, based on epidemiological data from the World Health Organization’s March 28, 2021, update. Higher incomes won’t prevent a person from death-by-coronavirus, but risks for the social determinants of health — exacerbated by income inequality — will and do. I have the good fortune of access to a study group paper shared by Paul Sheard, Research Fellow at the Mossaver-Rahmani Center for Business and Government at the Harvard Kennedy School. In reviewing
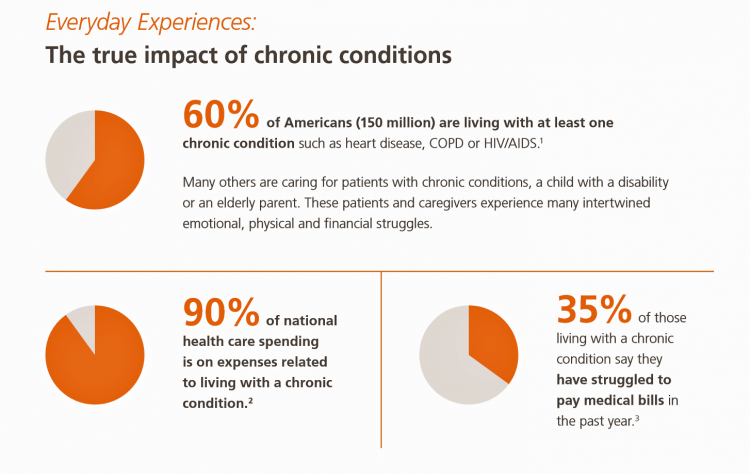
The Cost of Healthcare Can Drive Medical Rationing and Crowd Out Other Household Spending
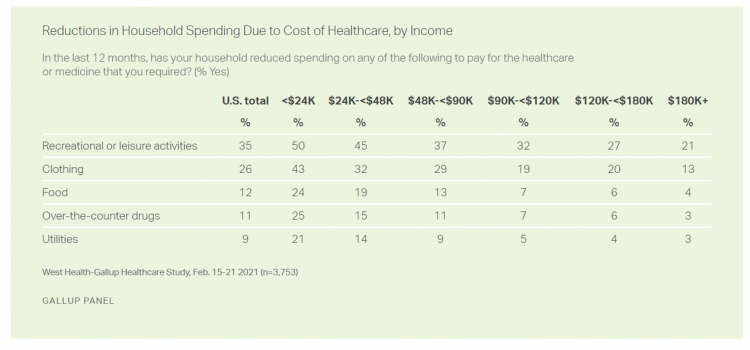
One in five people in the U.S. cannot afford to pay for quality health care — an especially acute challenge for Black and Hispanic Americans, according to a West Health-Gallup poll conducted in March 2021, a year into the COVID-19 pandemic. “The cost of healthcare and its potential ramifications continues to serve as a burdensome part of day-to-day life for millions of Americans,” the study summary observed. Furthermore, “These realities can spill over into other health issues, such as delays in diagnoses of new cancer and associated treatments that are due to forgoing needed care,” the researchers expected. The first table
A BA Degree as Prescription for a Longer Life – Update on Deaths of Despair from Deaton and Case
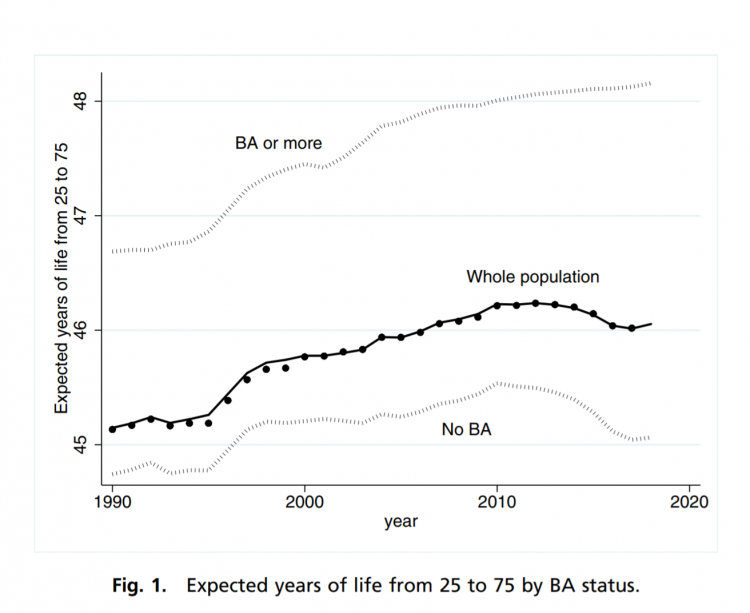
“Without a four-year college diploma, it is increasingly difficult to build a meaningful and successful life in the United States,” according to an essay in PNAS, Life expectancy in adulthood is falling for those without a BA degree, but as educational gaps have widened, racial gaps have narrowed by Anne Case and Angus Deaton. Case and Deaton have done extensive research on the phenomenon of Deaths of Despair, the growing epidemic of mortality among people due to accidents, drug overdoses, and suicide. Case and Deaton wrote the book on Deaths of Despair (detailed here in Health Populi), Case and Deaton
Value-Based Health Care Needs All Stakeholders at the Table – Especially the Patient

2021 is the 20th anniversary of the University of Michigan Center for Value-Based Insurance Design (V-BID). On March 10th, V-BID held its annual Summit, celebrating the Center’s 20 years of innovation and scholarship. The Center is led by Dr. Mark Fendrick, and has an active and innovative advisory board. [Note: I may be biased as a University of Michigan graduate of both the School of Public Health and Rackham School of Graduate Studies in Economics]. Some of the most important areas of the Center’s impact include initiatives addressing low-value care, waste in U.S. health care, patient assistance programs, Medicare
2020 Was Our Year of COVID; 2021 Will Be Our Year of Vaccines and Excess Deaths in America
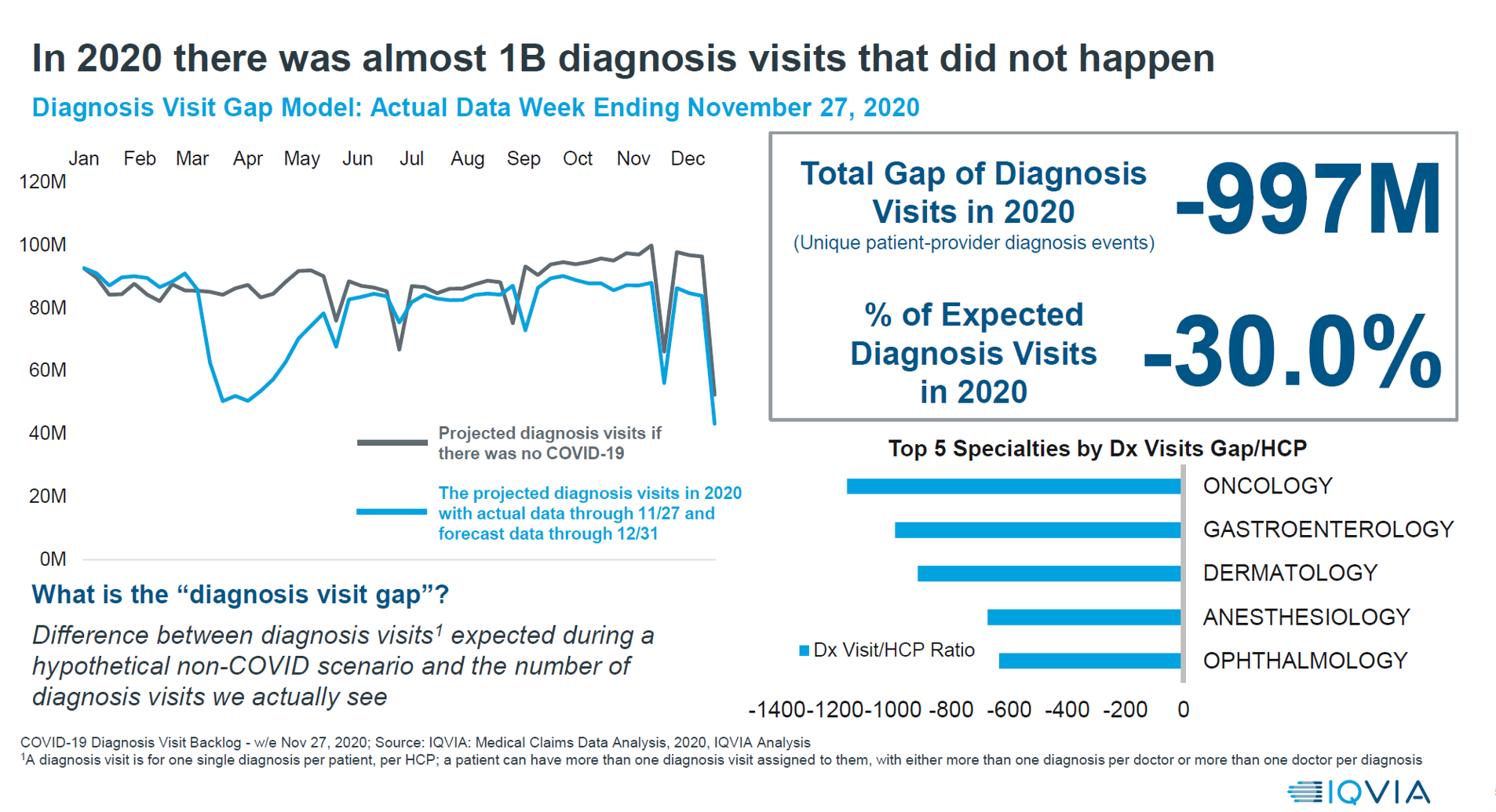
With a third vaccine approved by the FDA for licking COVID-19, brought to market by Johnson & Johnson, the U.S. can expect an uptick in vaccinations among fellow health citizens. That’s such welcome news and a positive outlook for a healthier 2021. But there’s another angle on 2021 for which health care providers and health citizens alike should prepare: that is the excess deaths that will happen due to patients postponing needed health care, diagnostic tests, and preventive services that stem from people avoiding care in doctor’s offices and hospitals. The chart here comes from IQVIA’s latest study into COVID-19’s
Americans Lost Future Life-Years in 2020: How Much Life Was Lost Depends on the Color of One’s Skin
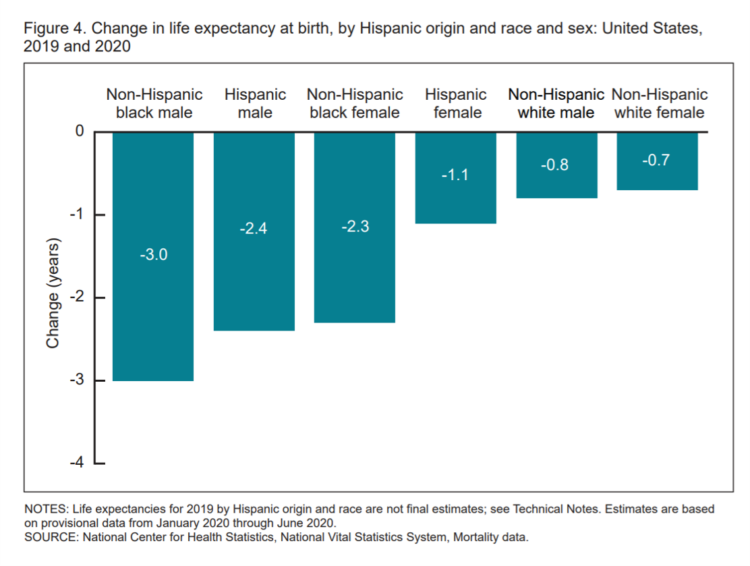
Some people remark about 2020 being a “lost year” in the wake of the coronavirus pandemic. That happens to be a true statement, sadly not in jest: in the U.S., life expectancy at birth fell by one full year over the first half of 2020 compared with 2019, to 77.8 years. In 2019, life expectancy at birth was 78.8 years, according to data shared by the National Center for Health Statistics (NCHS), part of the Centers for Disease Control and Prevention (CDC). Life expectancy at birth declined for both females and males, shown in the first chart. The differences between
Three in Four People Avoiding Health Care in the Pandemic Have Had Chronic Conditions
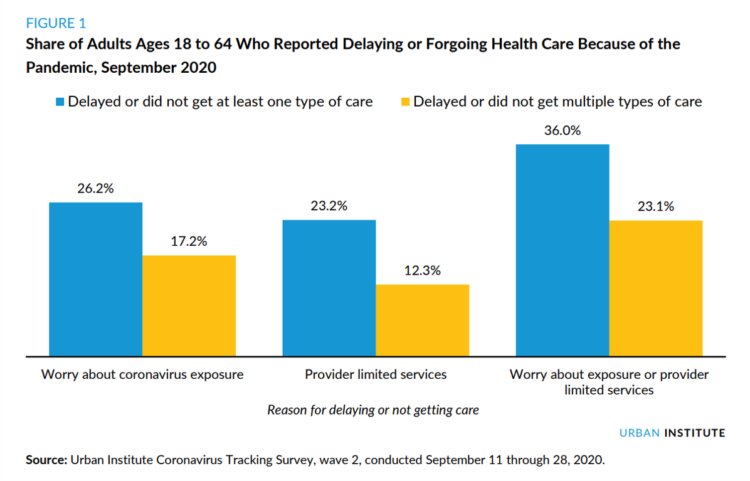
By the autumn of 2020, U.S. physicians grew concerned that patients who were avoiding visits to doctor’s offices were missing care for chronic conditions, discussed in in Delayed and Forgone Health Care for Nonelderly Adults during the COVID-19 Pandemic from the Urban Institute. More than three-fourths of people who delayed or forewent care had at least one chronic health condition. The pandemic may have led to excess deaths from diabetes, dementia, hypertension, heart disease, and stroke, as well as record drug overdoses in the 12 months ending in May 2020. In their JAMA editorial on these data, Dr. Bauchner and
The 2021 Shkreli Awards: Lown Institute Counts Down the Top 10 Healthcare Industry Abuses in the Coronavirus Pandemic

The first year of the coronavirus pandemic in America was a kind of stress test on the U.S. health care system, revealing weak links and opportunities for bad behavior. “These are not just about individual instances or bad apples,” Dr. Vikas Saini, President of The Lown Institute, explained, referring to them as “cautionary tales” of the current state of U.S. health care. Dr. Saini and his colleague Shannon Brownlee released the annual Lown Institute 2020 Shkreli Awards this week, highlighting their ten most egregious examples of the worst events in U.S. health care that happened in the past year —
The 2021 Health Populi TrendCast – Health Care, Self-Care, and the Rebirth of Love in Public Health

In numerology, the symbolic meaning behind the number “21” is death and re-birth. In tarot cards, 21 is a promise of fulfillment, triumph, and victory. How apropos that feels right now as we say goodbye and good riddance to 2020 and turn the page for a kinder, gentler, healthier New Year. It would be sinful to enter a New Year as challenging as 2021 promises to be without taking the many lessons of our 2020 pandemic life and pain into account. For health care in America, it is a time to re-build and re-imagine a better, more equitable landscape for
How COVID-19 Mobilized Participatory Health and the Importance of “Correct” Personal Health Records
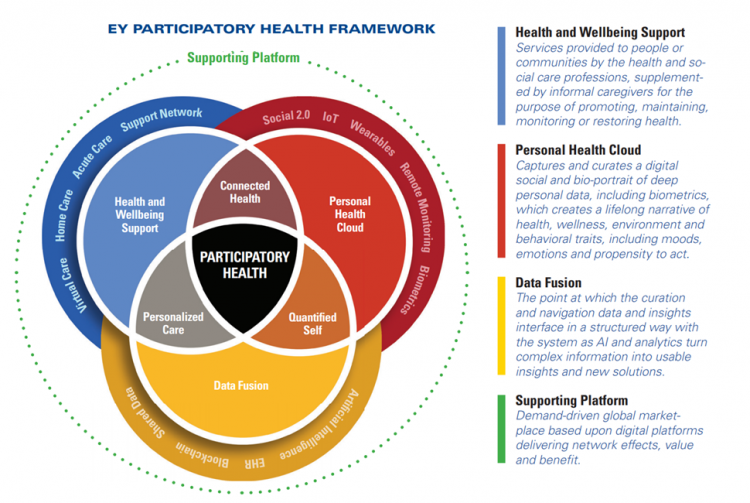
explained in a new report from EY co-sponsored by the American Hospital Association (AHA) and the AHA Center for Health Innovation. Digital Transformation – Anywhere Care envisions “health care with no address, or bringing care to the consumer or patient rather than expecting the patient to go to the hospital” as a “vital sign” of health care’s changes going into the new year of 2021. COVID-19 accelerated a movement in which I’ve been involved for over a decade, known as “participatory health.” In its early phase in the U.S., Dr. Tom Ferguson identified the emerging role of the internet in
The COVID Healthcare Consumer – 5 Trends Via The Medecision Liberation Blog
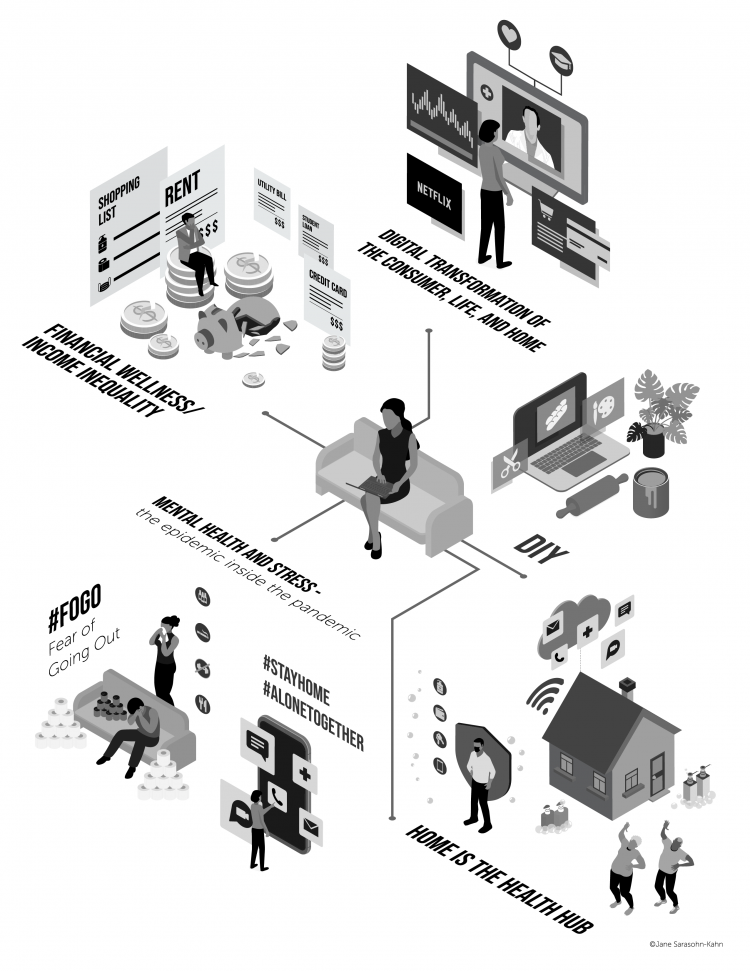
The first six months into the coronavirus pandemic shocked the collective system of U.S. consumers for living, learning, laboring, and loving. I absorbed all kinds of data about consumers in the wake of COVID-19 between March and mid-August 2020, culminating in my book, Health Citizenship: How a virus opened hearts and minds, published in September on Kindle and in print in October. In this little primer, I covered the five trends I woven based on all that data-immersion, following up the question I asked at the end of my previous book, HealthConsuming: when and how would Americans claim their health
Only in America: The Loss of Health Insurance as a Toxic Financial Side Effect of the COVID-19 Pandemic

In terms of income, U.S. households entered 2020 in the best financial shape they’d been in years, based on new Census data released earlier this week. However, the U.S. Census Bureau found that the level of health insurance enrollment fell by 1 million people in 2019, with about 30 million Americans not covered by health insurance. In fact, the number of uninsured Americans rose by 2 million people in 2018, and by 1.9 million people in 2017. The coronavirus pandemic has only exacerbated the erosion of the health insured population. What havoc a pandemic can do to minds, bodies, souls, and wallets. By September 2020,
My ABCovid-19 Journal – Day 3 of 5, Letters “K” through “O”
Welcome back to my ABCovid-19 Journal, which I created/curated in the early weeks of the coronavirus pandemic. This week, I’m sharing all the letters of the alphabet with you which reminded me keywords and themes emerging as we were learning about this dastardly public health threat beginning early in 2020. In today’s Health Populi blog I bring you letters “K” through “O,” continuing through the rest of the alphabet tomorrow and Friday while I’m on a lake-side holiday that’s good for mind, body, and spirit. K is for Kirkland, Washington state In the U.S., one of the earliest hotspots for
The Median Hospital Charge In the U.S. for COVID-19 Care Ranges From $34-45K
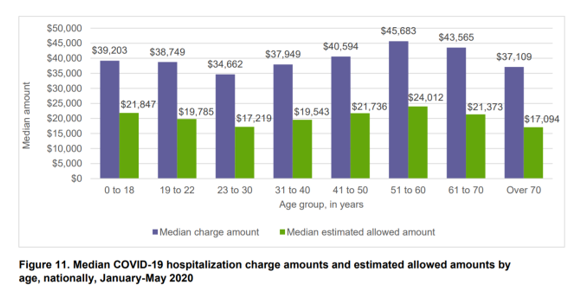
The median charge for hospitalizing a patient with COVID-19 ranged from $34,662 for people 23 to 30, and $45,683 for people between 51 and 60 years of age, according to FAIR Health’s research brief, Key Characteristics of COVID-19 Patients published July 14th, 2020. FAIR Health based these numbers on private insurance claims associated with COVID-19 diagnoses, evaluating patient demographics (age, gender, geography), hospital charges and estimated allowed amounts, and patient comorbidities. They used two ICD-10-CM diagnostic codes for this research: U07.1, 2019-nCoV acute respiratory disease; and, B97.29, other coronavirus as the cause of disease classified elsewhere which was the original code
Juneteenth 2020: Inequality and Injustice in Health Care in America
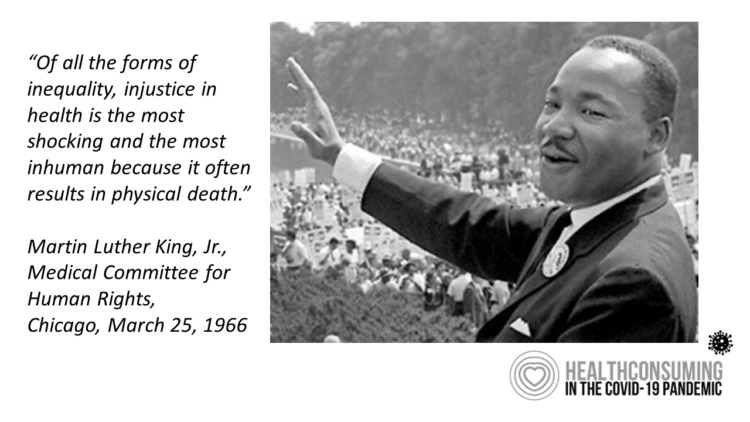
“Of all the forms of inequality, injustice in health is the most shocking and the most inhuman because it often results in physical death,” Martin Luther King, Jr., asserted at the second meeting of the Medical Committee for Human Rights in Chicago on March 25, 1966. This quote has been shortened over the five+ decades since Dr. King told this truth, to the short-hand, “Of all the forms of inequality, injustice in health care is the most shocking and inhumane.” Professor Charlene Galarneau recently enlightened me on Dr. King’s original statement in her seminal essay, “Getting King’s Words Right.” Among
How COVID-19 Is Driving More Deaths of Despair
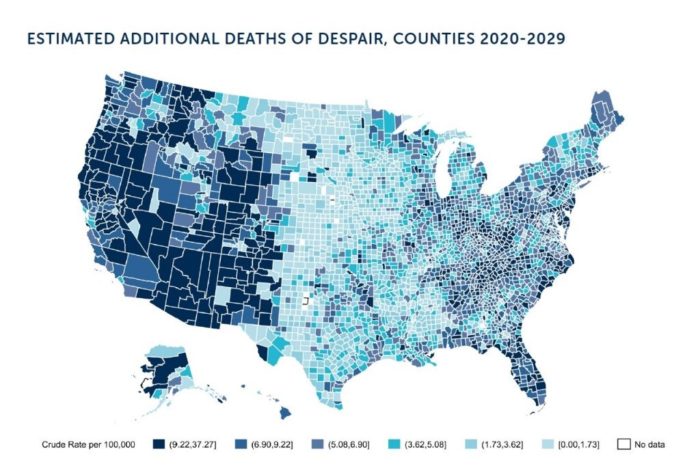
In the current state of the COVID-19 pandemic, we all feel like we are living in desperate times. If you are a person at-risk of dying a Death of Despair, you’re even more at-risk of doing so in the wake of the Coronavirus in America. Demonstrating this sad fact of U.S. life, the Well Being Trust and Robert Graham Center published Projected Deaths of Despair from COVID-19. The analysis quantifies the impact of isolation and loneliness combined with the dramatic economic downturn and mass unemployment with the worsening of mental illness and income inequity on the epidemic of Deaths of
Healthy Thinking: Inside the Mind of the COVID-19 Consumer
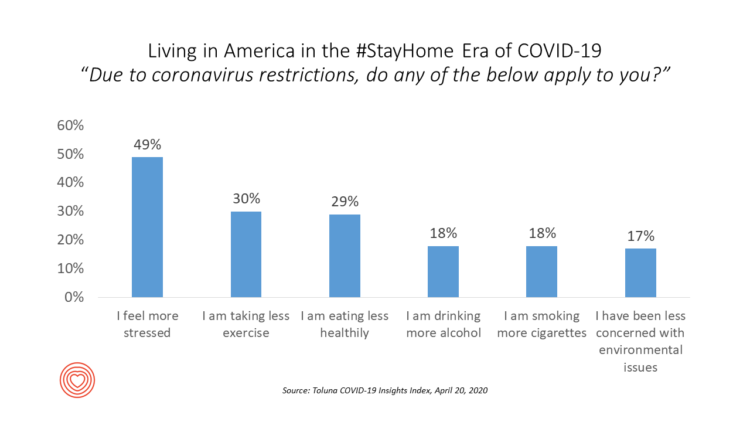
Stress is up, smoking increasing, drinking more alcohol….Americans are tapping into a variety of coping mechanisms in the coronavirus outbreak, with health on their collective minds. Toluna and Harris Interactive are collaborating on the COVID-19 Barometer, publishing biweekly data on consumers’ views on the coronavirus pandemic. The data here are a snapshot of consumers taken through the Toluna-Harris poll conducted among 1,047 U.S. adults between 9-20 April 2020. The first chart shows various life-flows Americans have adopted in April, all risk factors impacting peoples’ overall health status and mental well-being. There were demographic differences across these factors: more women felt
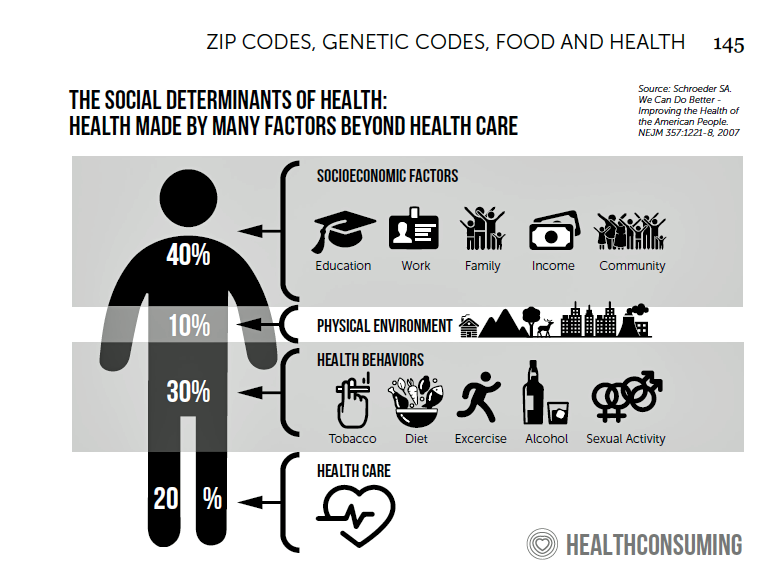
The Unsurprising Surprise of Social Determinants in COVID-19 Mortality
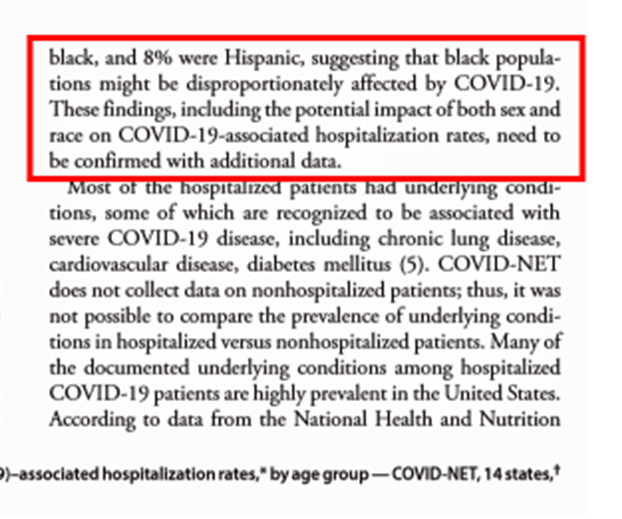
“Covid-19 exposes America’s racial health gap,” asserts The Economist, the weekly news magazine based in London, UK, in an advanced essay dated 11 April 2020. The subtitle of the piece: “African-Americans appear more vulnerable to the virus.” The phrase, “your ZIP code is more important than your genetic code” has become the common mantra for public health people communicating the concept of the social determinants of health: those factors outside of medical services that shape peoples’ overall health and well-being. Two days ago, the Centers for Disease Control (CDC) published data that showed African-Americans were dying from complications of the
The Coronavirus Impact on American Life, Part 2 – Our Mental Health
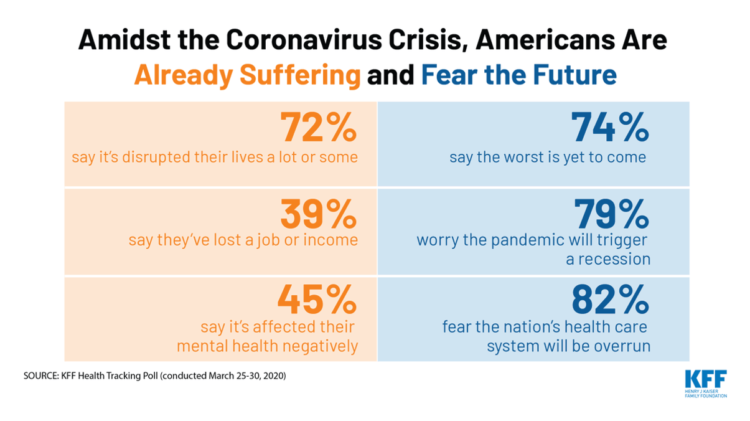
As the coronavirus pandemic’s curve of infected Americans ratchets up in the U.S., people are seeking comfort from listening to Dolly Parton’s bedtime stories, crushing on Dr. Anthony Fauci’s science-wrapped-with-empathy, and streaming the Tiger King on Netflix. These and other self-care tactics are taking hold in the U.S. as most people are “social distancing” or sheltering in place, based on numbers from the early April 2020 Kaiser Family Foundation health tracking poll on the impact of the coronavirus on American life. While the collective practice of #StayHome to #FlattenTheCurve is the best-practice advice from the science leaders at CDC, the NIAID
Steps Count: More Steps Are Self-Care Goodness in the COVID-19 Lifestyle
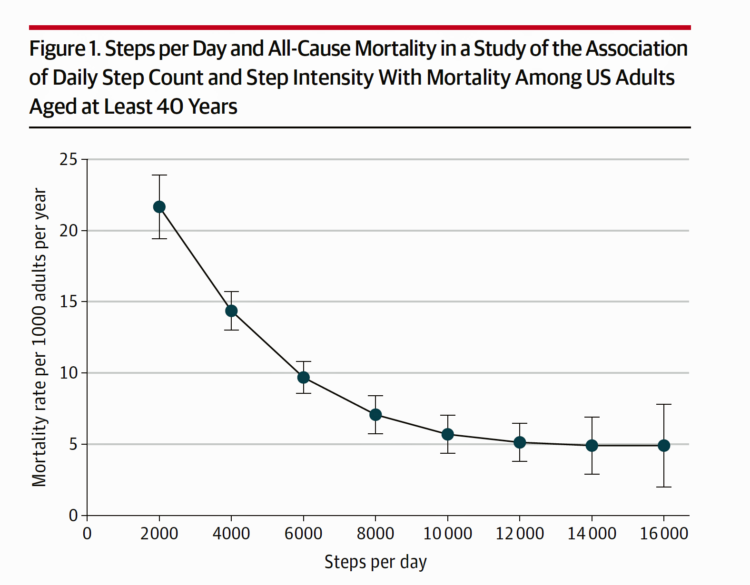
There’s evidence in this week’s JAMA of a dose-response relationship between peoples’ steps and lower mortality. In other words: more steps done daily is statistically significantly associated with death from all causes. Furthermore, step intensity didn’t make a difference in mortality rates, shown in the JAMA-published study, Association of Daily Step Count and Step Intensity With Mortality Among US Adults. The publication of this study is incredibly well-timed given the fact that hundreds of millions of people around the world are in lockdown, #StayHome lifestyles this week, and will be for many weeks to come. Going outside for fresh air
In the US COVID-19 Pandemic, A Tension Between the Fiscal and the Physical

“Act fast and do whatever it takes,” insists the second half of the title of a new eBook with contributions from forty leading economists from around the world. The first half of the title is, Mitigating the COVID Economic Crisis. The book is discussed in a World Economic Forum essay discussing the economists’ consensus to “act fast.” As the U.S. curve adds new American patients testing positive for the coronavirus, the book and essay illustrate the tension between health consumer versus the health citizen in the U.S. For clinical context, as I write this post on 24th March 2020, today’s U.S.
In A Nation “At War” with the C19 Virus, Partisan Healthcare Differences Persist
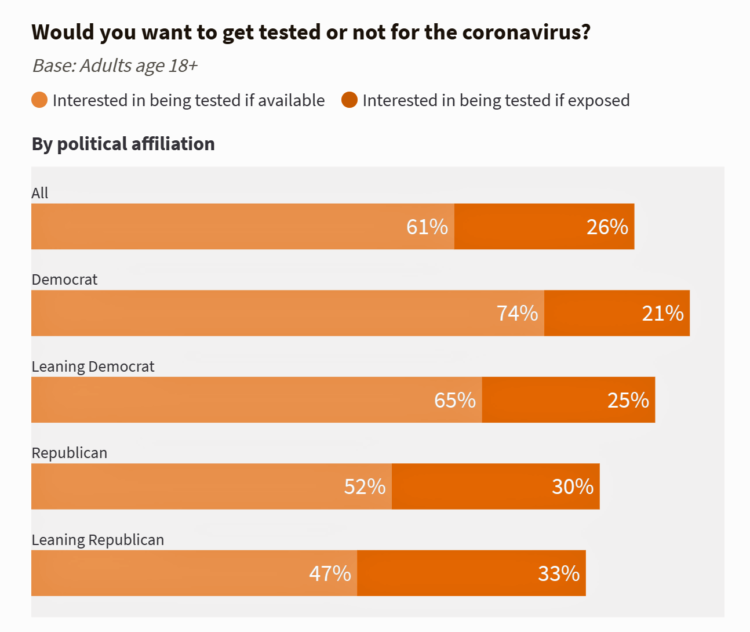
More Democrats would want to get tested for the coronavirus (C19) than would Republicans. And, more women than men believe that a vaccine to address the COVID-19 pandemic believe that treatment would be offered at no-or-low-cost under a Democratic president versus President Trump. These are two key insights gleaned from a look into U.S. adults’ perspectives on the C19 virus in the second week of March 2020. What Are Americans’ Views on the Coronavirus Pandemic? asks and answers an NBC News/Commonwealth Fund Health Care Poll published on 20th March 2020. NBC News and the Commonwealth Fund polled 1,006 people 18
The Book on Deaths of Despair – Deaton & Case On Education, Pain, Work and the Future of Capitalism
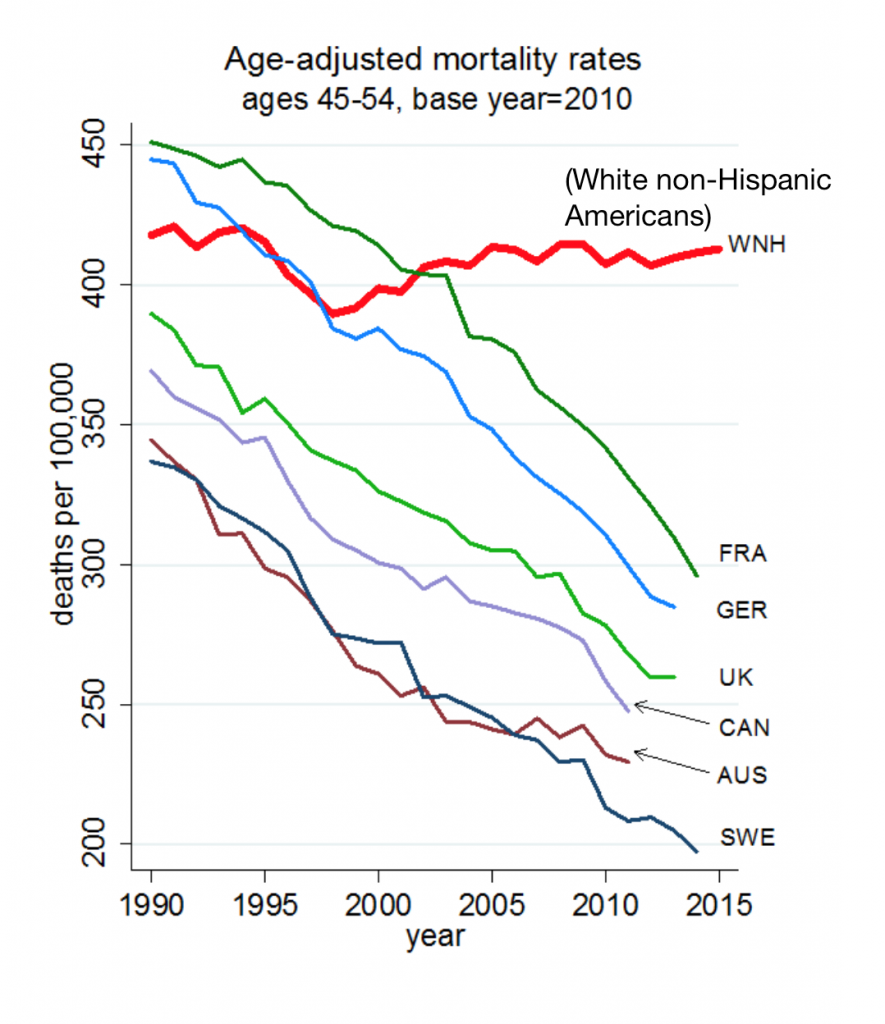
Anne Case and Angus Deaton were working in a cabin in Montana the summer of 2014. Upon analyzing mortality data from the U.S. Centers for Disease Control, they noticed that death rates were rising among middle-aged white people. “We must have hit a wrong key,” they note in the introduction of their book, Deaths of Despair and the Future of Capitalism. This reversal of life span in America ran counter to a decades-long trend of lower mortality in the U.S., a 20th century accomplishment, Case and Deaton recount. In the 300 pages that follow, the researchers deeply dive into and
The 2020 Social Determinants of Health: Connectivity, Art, Air and Love
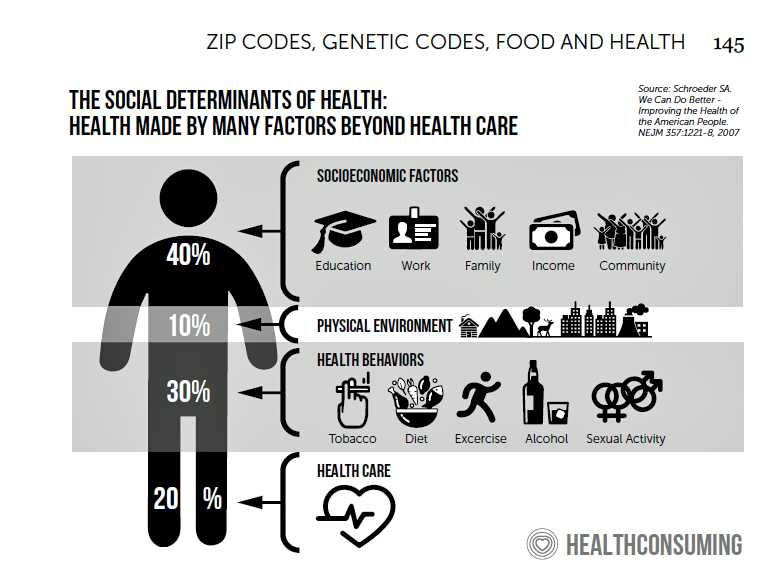
Across the U.S., the health/care ecosystem warmly embraced social determinants of health as a concept in 2019. A few of the mainstreaming-of-SDoH signposts in 2019 were: Cigna studying and focusing in on loneliness as a health and wellness risk factor Humana’s Bold Goal initiative targeting Medicare Advantage enrollees CVS building out an SDOH platform, collaborating with Unite US for the effort UPMC launching a social impact program focusing on SDoH, among other projects investing in social factors that bolster public health. As I pointed out in my 2020 Health Populi trendcast, the private sector is taking on more public health
Social Determinants of Health – My Early Childhood Education and Recent Learnings, Shared at the HealthXL Global Gathering
My cousin Arlene got married in Detroit at the classic Book Cadillac Hotel on July 23, 1967, a Sunday afternoon wedding. When Daddy drove us back out to our suburban home about 30 minutes from the fancy hotel, the car radio was tuned to WWJ Newsradio 950, all news all the time. As soon as Daddy switched on the radio, we were shocked by the news of a riot breaking out in the city, fires and looting and gunshots and chaos in the Motor City. Two days later, my father, who did business with Mom-and-Pop retail store owners in the
Art As Medicine – WHO Weaves the Evidence for Arts’ Role in Improving Health

“What’s the evidence on the role of the arts in improving health and well-being?” asks a report from the World Health Organization‘s Europe region team (WHO-Europe). There’s a lot of proof supporting arts-as-medicine, WHO details in this paper, which synthesizes research published in over 3,000 studies. The first chart illustrates the logic model that bridges arts to health in three segments: “Components” of arts programs, including but not limited to cognitive stimulation (e.g., learning a new arts skill such as painting, drawing or journaling), social interaction (e.g., participating in theatre), physical activity (e.g., dance), and evocation of emotion (e.g., listening
Making Health Care Better, from the N of 1 to the Public’s Health – Trend-Weaving Medecision Liberation 2019
Health and our health information are deeply personal. Changing health care and inspiring positive health behaviors is hard to do. But we must and we will, a group of inspiring and inspired people who work across the health/care ecosystem affirmed this week in Dallas at the conference of Medecision Liberation 2019. I was engaged at this conference to wear several hats — as a keynote speaker, a sort of “emcee,” and, finally, to trend-weave the many talks and discussions happening throughout the meeting. This post is my synthesis of the summary I delivered live at the end of the conference,
Health Care Bills’ Financial Toxicity – Remembering the Jones’ of Whatcom County, WA
“In an extreme example of angst over expensive medical bills, an elderly Washington couple who lived near the U.S.-Canadian border died in a murder-suicide this week after leaving notes that detailed concerns about paying for medical care,” USA Today reported on August 10, 2019. Five years ago, financial toxicity as a side-effect was noted by two Sloan Kettering Medical Center in a landmark report on 60 Minutes in October 2014. Epidemiologist Peter Bach and oncologist Leonard Saltz told CBS’s Lesley Stahl, “A cancer diagnosis is one of the leading causes of personal bankruptcy…We need to take into account the financial
Gaps in Health Equity in America Are Growing

There’s been a “clear lack of progress on health equity during the past 25 years in the United States,” asserts a data-rich analysis of trends conducted by two professors/researchers from UCLA’s School of Public Health. The study was published this week in JAMA Network Open. The research mashed up several measures of health equity covering the 25 years from 1993 through 2017. The data came out of the Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System looking at trends by race/ethnicity, sex and income across three categories for U.S. adults between 18 and 64 years of age.





 I'm once again pretty gobsmackingly happy to have been named a judge for
I'm once again pretty gobsmackingly happy to have been named a judge for  Stay tuned to Health Populi in early January as I'll be attending Media Days and meeting with innovators in digital health, longevity, and the home-for-health during
Stay tuned to Health Populi in early January as I'll be attending Media Days and meeting with innovators in digital health, longevity, and the home-for-health during  Jane collaborated on
Jane collaborated on