explained in a new report from EY co-sponsored by the American Hospital Association (AHA) and the AHA Center for Health Innovation.
Digital Transformation – Anywhere Care envisions “health care with no address, or bringing care to the consumer or patient rather than expecting the patient to go to the hospital” as a “vital sign” of health care’s changes going into the new year of 2021.
 COVID-19 accelerated a movement in which I’ve been involved for over a decade, known as “participatory health.” In its early phase in the U.S., Dr. Tom Ferguson identified the emerging role of the internet in health care as a way to democratize health information and bring together patients with providers in a “participatory” mode of shared decision-making, empowering both sides of the relationship to bolster the patient’s health outcomes and the physician’s clinical (and emotional/social) success.
COVID-19 accelerated a movement in which I’ve been involved for over a decade, known as “participatory health.” In its early phase in the U.S., Dr. Tom Ferguson identified the emerging role of the internet in health care as a way to democratize health information and bring together patients with providers in a “participatory” mode of shared decision-making, empowering both sides of the relationship to bolster the patient’s health outcomes and the physician’s clinical (and emotional/social) success.
The bulk of this report speaks about three shifts toward digital transformation in health care, toward:
- Delivering convenient care anywhere, anytime
- Moving from digital to “smart” (meaning data-driven analytics to improve care, user experience, and operations)
- Managing social determinants and not just clinical care.
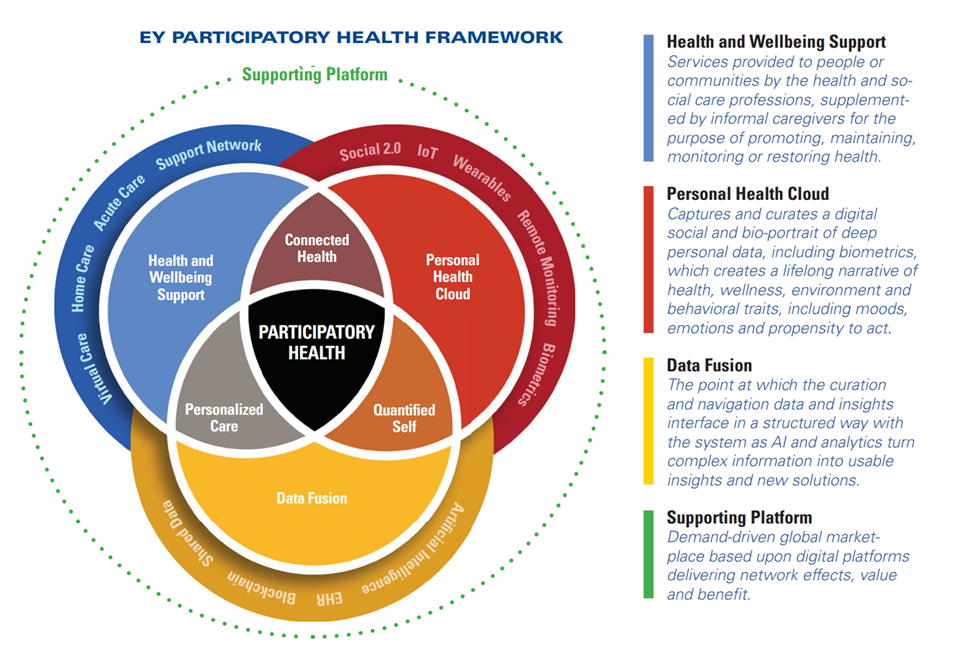
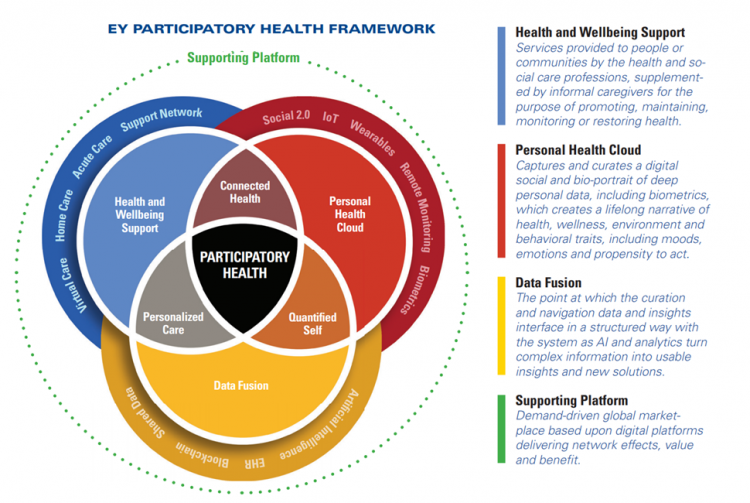
But the start of the report rightly focuses on EY’s Participatory Health Framework, which is the not-so-secret in the sauce to making virtual care clinically, operationally, and economically successful.
The Venn diagram connects health and wellbeing support, personal health clouds, and “data fusion” (the “curation and navigation” of data and insights that inform medical decisions) across the continuum of care which is “everywhere:” from home to hospital to our bodies via wearable tech and implantable sensors.
The new-new thing here for participatory health is the personal health cloud, which curates and captures our data — not just medical claims information, but the stuff of life, everyday — about our health, wellness, environment, behavioral choices, moods, sex-drugs-rock-and-roll. All of these bits and bytes paint our personal life pictures beyond what the pharmacy and hospital and lab know about us.
 Health Populi’s Hot Points: Dr. Charles Safran testified to Congress way back on June 17, 2004. At the time of the testimony, Dr. Safran was President of the American Medical Informatics Association (AMIA). The last paragraph of his statement to the Ways and Means Subcommittee on Health read:
Health Populi’s Hot Points: Dr. Charles Safran testified to Congress way back on June 17, 2004. At the time of the testimony, Dr. Safran was President of the American Medical Informatics Association (AMIA). The last paragraph of his statement to the Ways and Means Subcommittee on Health read:
In our country, patients are the most underutilized resource, and they have the most at stake. They want to be involved, and they can be involved. Their participation will lead to better medical outcomes at lower cost with dramatically higher patient and customer satisfaction. We should remember that the real goal of improved health information systems is not better hospitals or better physician practices but better quality of care and healthier citizens.
The timing of EY’s Participatory Health call-out couldn’t be better planned if ePatient Dave DeBronkart tried to make happen. That’s because today at 1 pm Eastern time, the HL7 Standards Committee will convene a planning meeting online to prepare for the January 13-15, 2021, patient medical records “Correctathon.”
Here’s the link to the event and background.
I’ll summarize that background for context and clarity about why this development is so important to U.S. health care and Americans’ health citizenship. HL7 is a standards-setting convening group that provides a framework for HL7 and its members provide a framework and standards for exchanging, integrating, sharing, and retrieving electronic health information. These standards are critical for the ability to make our health data “liquid,” able to move where it needs to go to ensure safe and effective medical care. Standards and the workflows they empower enable interoperable data. That’s been elusive from the start of implementing electronic health records, even today in the age of wearable tech and smartphones.
In case the concept of “interoperability” feels too wonky and distant to you, note that Bruce Broussard, CEO of Humana the health insurer, recently wrote about the importance of interoperability to fight the COVID-19 public health crisis.
HL7 recently created a Patient Empowerment workgroup with an eye on creating a FHIR Implementation Guide for Patient Request for Correction patients’ records that have the wrong information in them.
This real problem is a long-time patient safety problem which, literally, can be the source of a life-or-death outcome.
EY’s call-out of participatory health is critical to our health citizenship: our right to health care, the criticality of digital citizenship and consumer data control, while empowering and supporting patients to engage in self-care and shared decision making.




 Thank you,
Thank you,  As a proud Big Ten alum, I'm thrilled to be invited to
As a proud Big Ten alum, I'm thrilled to be invited to  I was invited to be a Judge for the upcoming CES 2025 Innovation Awards in the category of digital health and connected fitness. So grateful to be part of this annual effort to identify the best in consumer-facing health solutions for self-care, condition management, and family well-being. Thank you, CTA!
I was invited to be a Judge for the upcoming CES 2025 Innovation Awards in the category of digital health and connected fitness. So grateful to be part of this annual effort to identify the best in consumer-facing health solutions for self-care, condition management, and family well-being. Thank you, CTA!