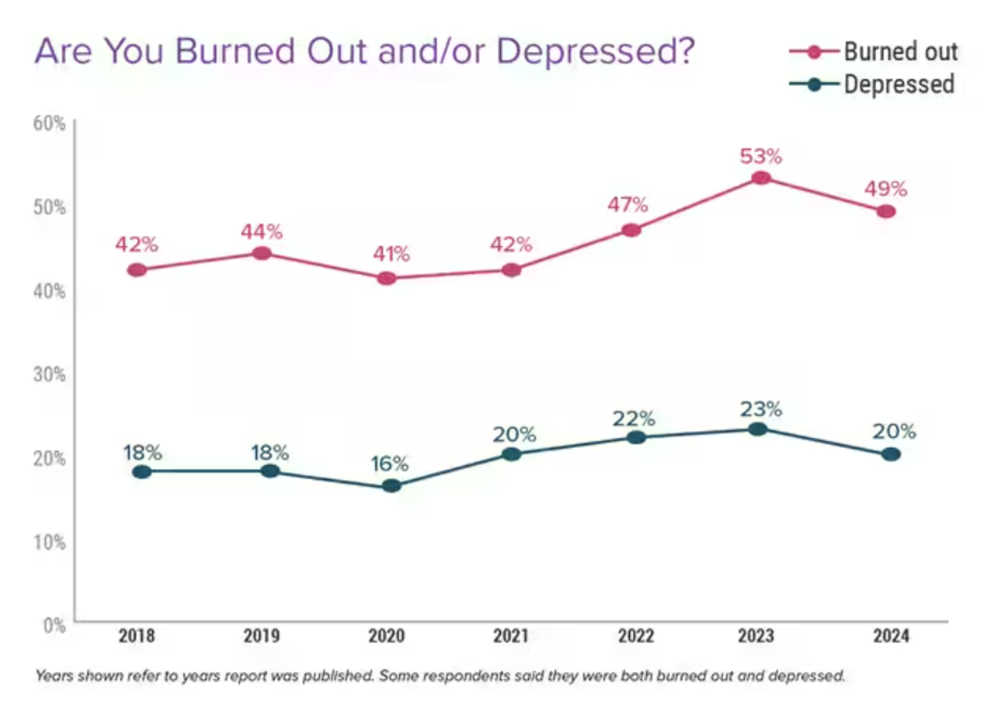
One-half of U.S. physicians report feeling burned out, and 3 in 5 of those doctors say they have felt burned out for over two years, according to the Physician Burnout & Depression Report for 2024 from Medscape. While the study’s press release asserts there may be “progress” given the percent of doctors citing burnout fell by 4 percentage points from 53% of doctors in 2022 to 49% in 2023, it is obvious the U.S. physicians need greater support and less taboo concerning their mental health which impacts both their professional and personal lives.

For this annual study, Medscape polled 9.226 U.S. practicing clinicians online between July and October 2024. The clinicians represented 29+ specialties.
The specialty with the greatest percentage of physicians reporting burnout were in emergency medicine, 63% of whom said they fell into the burnout zone. Following emergency doctors, 50% plus of the following specialties reported burnout: Ob/Gyn, Oncology, Pediatrics, Family Medicine, Radiology, Pulmonary Medicine, Anesthesiology, Gastroenterology, and Internal Medicine.
The least likely to feel burned out, according to Medscape, were plastic surgeons (37%), ophthalmologists (39%), and psychiatrists (39%).
Burnout is more prevalent than depression: 49% of physicians cited burnout in 2024 versus 20% of clinicians saying they were depressed.
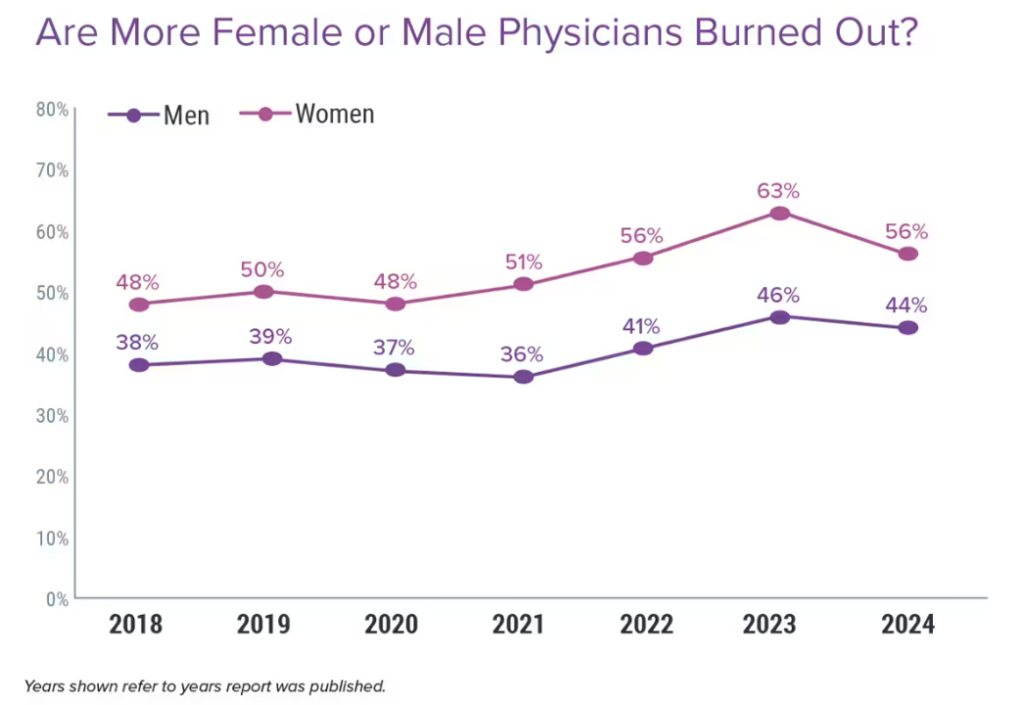
Underneath the burnout statistic, women physicians were more likely to say they felt burnout compared with male doctors — by a rate of 56% of women versus 44% of men practicing medicine.
Regardless of whether the doctor was male or female, equal percentages of them said their burnout or depression was due to job stress — for both genders, 30% said “all” of the burnout/depression was due to work and 53% said most of the mental health issues were due to job stress.
42% of physicians said they had felt burned out for over two years.
What underpins clinicians feelings of burnout? What factors have most contributed?
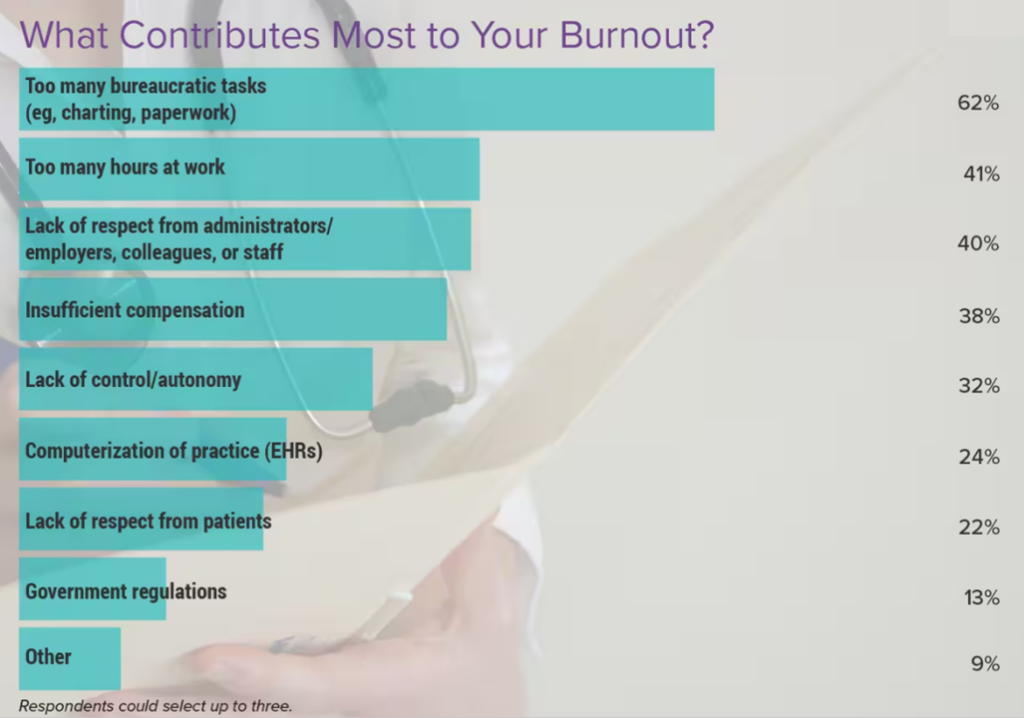
By far the #1 cause contributing to burnout was too many bureaucratic tasks — such as charting and paperwork (a burden that has been well-documented especially following the implementation of electronic health records).
Following dealing with bureaucracy, clinicians feeling burnout point to too many hours at work; lack of respect from administrators, employers, colleagues or staff; and, insufficient control and lack of autonomy.
Burnout has also impacted physicians’ personal relationships: “somewhat” among 73% and “a lot” for 13%.
Notwithstanding their self-awareness about burnout and/or depression, most physicians have not reached out for professional help for their conditions current or in the past. Only 15% of doctors feeling burnout had ever reached out for professional help, and only 11% of physicians citing depression did so. Why would doctors not tell anyone about their feelings of depression?
The top reasons were,
- That people might doubt my abilities as a physician, among 44% of the clinicians
- That the Medical Board or employer could find out (for 42%), and,
- That it makes a negative statement about me personally, for 40% of the doctors.
Physicians who maintain happiness and mental health cited several strategies and lifestyle choices, with most turning to spending time with family and friends, activities and hobbies (like reading, cooking, and gardening), exercise, getting enough sleep, and eating healthy.
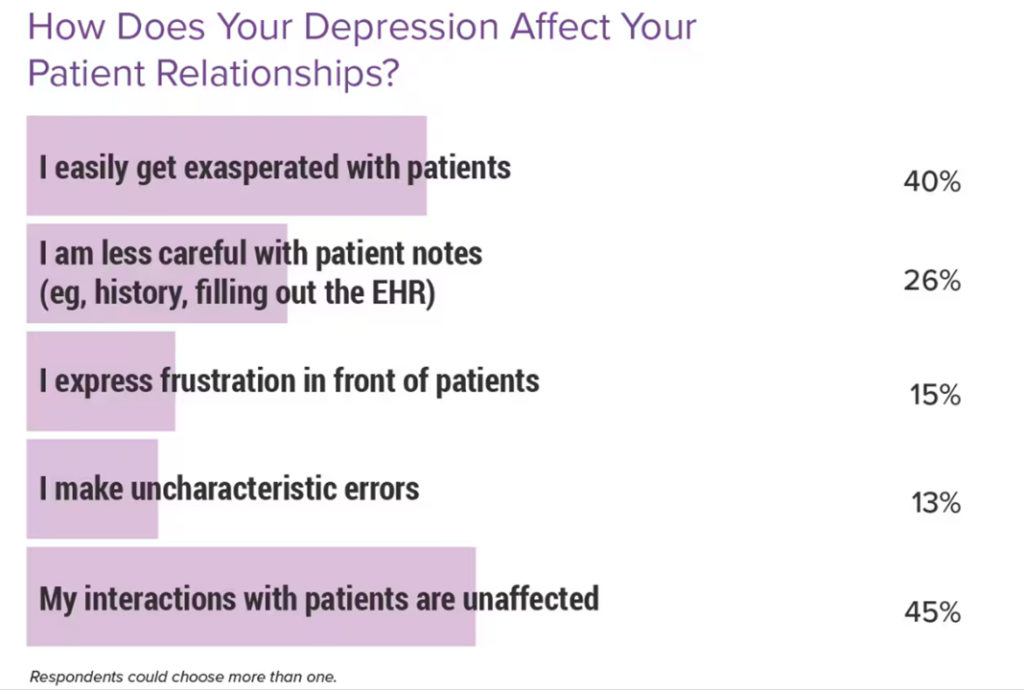
Health Populi’s Hot Points: While physicians admitted their personal relationships are negatively impacted by burnout and/or depression, they also are self-aware that their mental health impacts their patient relationships.
40% of doctors said they easily get exasperated with patients. Another 26% admit to being less careful with patient notes, and 15% express frustration in front of patients.
While nearly 50% of doctors said their interactions with patients are “unaffected,” this translates to 55% of physicians whose interactions with patients are impacted by burnout or depression.
How to address the observed sources of stress on clinicians? In terms of staffing deficiencies and lack of support, the most immediate relief can be further implementing team-based care, respecting licensed professionals working at the top of their license and supporting these clinicians across-the-board with technology that’s well-designed with their involvement.
Further supporting productivity and autonomy would be bringing telehealth and omnichannel care fully to health care, enabling patient-physician consultations cross-state borders and paying for visits that may be asynchronous — that is, not in real-time — giving time back to both physicians and patients but ensuring continuity-of-care and access.
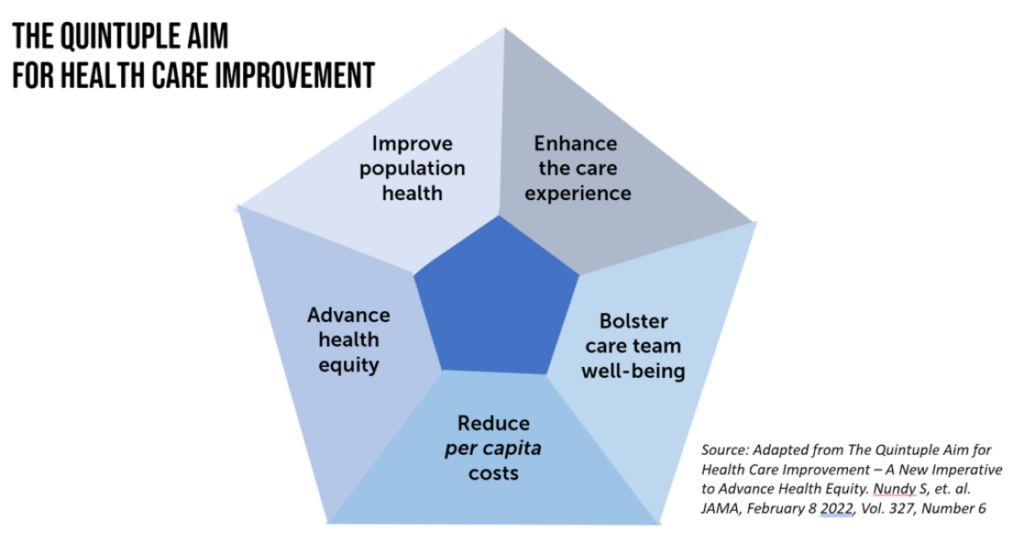
The annual Medscape study into physicians’ feelings of burnout, which underpins depression in the report, reminds us to embrace the pillars of the Quintuple Aim — especially to support clinicians’ well-being and to enhance the patient’s health care experience. Attending the other three factors — addressing cost per capita/patient, bolstering population health outcomes, and dealing with health equity also feed into a virtuous cycle of improving health care for all.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...