 Among the limiting factors that will prevent full realization of the benefits of health reform, one is most pressing: the deficit of primary care providers (PCPs).
Among the limiting factors that will prevent full realization of the benefits of health reform, one is most pressing: the deficit of primary care providers (PCPs).
A comment in the April 21st 2010 Journal of the American Medical Association lays out the facts about the primary care shortage with several data points:
1. There are 900 million visits to physicians each year in the U.S. 50% of these go to 200,000 physicians who call themselves primary care clinicians.
2. Most of these visits deal with the super-sized conditions of diabetes, hypertension and obesity, along with infections and general exams.
3. Specialists see a growing number of patients with arthritis, epilepsy, depression, and other chronic conditions.
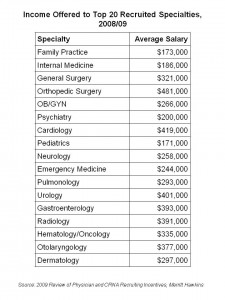
4. The salary differential between PCPs and specialists is huge: the average internist earns about $186,000; the average dermatologist brings home an annual paycheck of $297,000. The chart on the left illustrates the large pay gaps between PCPs and specialties.
No wonder, then, that in 2010, only 55% of 4,999 residency posts in internal medicine were U.S. med school graduates. 90% of specialty posts in brain surgery, orthopedic surgery, and dermatology were given to U.S. med school grads.
The Association of American Medical Colleges’ Center for Workforce Studies calculates a shortage of 46,000 primary care physicians and 41,000 general surgeons — even with the recruitment of international medical graduates.
The authors of the JAMA commentary lament: “Despite efforts to highlight the potential clinical and professional contributions of primary care physicians, interest int his path remains extraordinarily low among graduates of U.S. medical schools.”
Health Populi’s Hot Points: If this status quo continues, then primary care will become a boutique retail health service for those who can afford to pay a premium for it. In addition to this being an ironic kind of outcome, it’s also very harmful to the basic public health of the U.S. And with some 30 million people in the U.S. being added to the covered insured, the practical question is: will they be able to access a PCP?
So how to make primary care attractive to medical students and bring sexy back to being a PCP? It’s about money, sure — closing the gap between the Botoxers and the Brain Surgeons vs. the Marcus Welby’s.
But it’s also going to mean paying PCPs based on the huge value they bring to the health system, one patient at a time: preventing errors, being a rational allocater of expensive health resources (like hospital admissions, MRI scans and unnecessary surgical procedures), and finally, rewarding doctors for keeping people well.
“…The role of the primary care physician [must be] redefined in a powerful way,” the authors say.
Let’s not confuse coverage with access. It’s going to take more than a 10% bump up in Medicare reimbursement to bring sexy back to primary care.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.