 The Affordable Care Act (ACA), aka health reform, will move 32+ million Americans to the insured population, and looks to the primary care ‘front-end’ of health care delivery to take in these newly-covered patients.
The Affordable Care Act (ACA), aka health reform, will move 32+ million Americans to the insured population, and looks to the primary care ‘front-end’ of health care delivery to take in these newly-covered patients.
Today’s USA Today reports on the primary care shortage in America. How to reconcile the influx of new patients in the U.S. health system with the deficit of primary care providers?
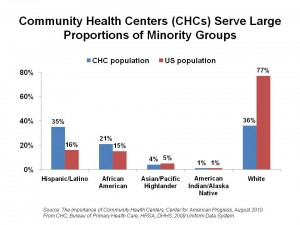
First, the Community Health Center is one part of the solution to the primary care supply challenge. Furthermore, CHCs are integrated into ACA, seen as a key component for redesigning American health care delivery to improve quality, lower cost, and expand access to people who’ve not benefited from a regular medical home. CHCs will receive additional $9.5 billion worth of funding in the next five years to expand services for operating costs, and an additional $1.5 billion for new construction.
A report from the Center for American Progress (CAP), The Importance of Community Health Centers, presents the evidence that CHCs drive economic growth and job creation in their local markets.
CAP calculates that investing in CHC yields economic benefits for their local communities. They found that the $2 billion of stimulus funding generated $3.2 billion worth of economic activity, with CHCs generating $20 billion of economic activity. As a result, some additional 284,000 jobs accrue on top of the expected 173,289 jobs without ACA stimulus funding).
Health Populi’s Hot Points: Notwithstanding the funding of CHCs, there’s a primary care physician shortage in the U.S., as detailed in today’s USA Today (linked above). The economic value of CHCs is obvious, and the concept has received bipartisan support since George W. Bush’s presidency. But primary care workforce shortages aren’t solvable by 2015, so the intent of covering the uninsured especially for patient centered medical homes and primary care access doesn’t translate into actual access for all-comers into the system.
What can play important roles to expand access are technologies, such as broadband for telemedicine and mobile health technologies, whether via feature phones or smartphones. As discussed in Health Populi on August 13, 2010, expanding broadband to underserved communities can expand health citizens’ access to seeking health information online. A second sort of communications technology ‘prescription’ will also be useful: that is, extending services via mobile phone between providers, including CHCs, and patients, especially for simple primary care questions and for managing chronic conditions.
The key to making this scenario work will be designing interfaces and applications that are very useable and engaging to patients, and that fit into the workflow of the clinician and health center.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...