 The $N zillion question – whether translated into Euros, yen, pounds, lira, or pesos – is how to get more quality care and access in national health systems, while curbing health spending.
The $N zillion question – whether translated into Euros, yen, pounds, lira, or pesos – is how to get more quality care and access in national health systems, while curbing health spending.
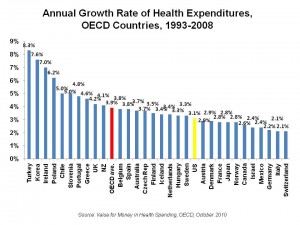
Health costs have increased faster than economic development in nearly all OECD countries in the past 15 years.
For the acronym-challenged, the OECD is the Organization of Economic Cooperation and Development – comprised of, generally, the most economically developed nations on Earth.
This week, health maestros from OECD nations are meeting to wrestle this intractable challenge. Health costs consume about 9% of OECD countries’ budgets. This proportion of national GDPs exceeds 10% in seven countries including the U.S., Germany, France, Switzerland, Austria, Canada and Belgium. To bolster understanding of the tough issues in finding VFM in health, OECD published Value for Money in Health Spending, a primer on the topic, this week.
The chart organizes per capita health cost increases between 1993 and 2008 for OECD nations, showing that the average increase in the interval was 3.9% for all OECD. The greatest increases in per capital health spending occurred in Turkey, Korea, Ireland, Poland, and Chile in the 15 year period.
The OECD points out that measures to restrict health spending in the short-term, such as capping wages on doctors and prices on hospitals, or allocating more out-of-pocket costs to health citizens, can exacerbate spending inflation in the long-run.
The solutions, OECD argues, are to (1) incorporate evidence-based medicine into clinical decision making and (2) expand health technology assessments, again to inform clinical and coverage decisions.
Health Populi’s Hot Points: While U.S. spending per person grew at a slower rate than other countries at 3.1%, the nation’s health spending as a percentage of total budget exceeds every developed nation, fast approaching 1 in 5 dollars.
There will be both art and science involved in stemming the growth of health costs, in and beyond U.S. borders. EBM and HTA ask the questions: “Does the [drug, therapy, procedure] work?” and “Is the [drug, therapy, procedure] ‘worth’ it?”
While EBM, HTA and Paying for Performance (P4P) are expanding in most OECD countries and many low-income nations, there’s not much evidence on these payment reforms…yet. Ironically, the best outcomes have been found, thus far, in World Bank administered public health initiatives paying for preventions such as cancer screening and HIV drug adherence programs in Rwanda and elsewhere.
The role of health IT in helping stem health cost growth cannot be undervalued. OECD rightly points out that the party that invests in HIT often doesn’t reap the benefits of HIT implementation. Thus, alignment of incentives is key to HIT adoption, and the HITECH incentives in ARRA attempt to get at this mis-alignment.
Furthermore, health citizens ‘ourselves’ have much to do with slowing health costs inflation, especially in avoiding unnecessary costs. The smarter the patient, the more engaged the patient, the better the outcome and, ultimately, the more rational the health spending. This calls for a new regime of participatory health for the world. OECD asserts, “The role of patients in the care process has also taken on much greater importance in recent years. Yet it has been very difficult to determine the best way to involve patients in their own care, not least because people vary greatly in their responsiveness to information, advice and treatment guidelines.”
Today I will be part of an afternoon of Patients 2.0, to kick of the mega Health 2.0 Conference in San Francisco. We will cover this very issue — by patients, for patients. More to follow on this in Health Populi tomorrow…




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...