 “The impending Medicaid expansion will be the single biggest change in the program since its inception in 1965,” according to an analysis in the New England Journal of Medicine dated November 24, 2010.
“The impending Medicaid expansion will be the single biggest change in the program since its inception in 1965,” according to an analysis in the New England Journal of Medicine dated November 24, 2010.
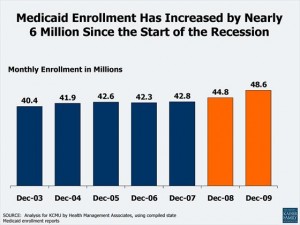
The Patient Protection and Affordable Care Act (PPACA, or ACA for short) will newly-insure 32 million Americans through dual strategies of (1) mandating uninsured people to buy into a health plan, via subsidies and health insurance exchanges; and, (2) expanding Medicaid to cover uninsured people with lower incomes. The CBO estimates that each of these tactics will add 16 million, for the total of 32 million people entering insurance plans and, presumably, the health care delivery system.
The NEJM perspective is titled, Medicaid Expansion – The Soft Underbelly of Health Care Reform? Why “soft underbelly?” For 3 reasons, Summers and Epstein, the authors, say:
1. Current participation rates in Medicaid are only 2 in 3 eligible, meaning that 1 in 3 people eligible to receive health benefits under the Medicaid program are not enrolled in it.
2. Across the 50 states, participation is highly variable, from a low of 44% in Oklahoma, Oregon and Florida, to highs in Washington DC (88%) and Massachusetts (80%).
3. States with the largest number of newly-eligible people have proven less effective at getting them to enroll, and retaining these enrollees, in Medicaid.
The factors behind these reasons are many, and some unknowable today. Among the driving forces shaping the ‘underbelly of Medicaid’ are administrative obstacles to enrolling in the program, provider reimbursement rates (i.e., low), and outreach and public education are some of the factors we know about.
Health Populi’s Hot Points: Summers and Epstein anticipate that, all things being equal – that is, if the current sort of administrative and paperwork challenges, along with education efforts about Medicaid availability and eligibility, continue — enrolling the newly-eligible people into Medicaid will go slowly. This effort will require using the tools of social marketing and innovative approach to behavior change in health. With 3 years between ‘now’ and when Medicaid expansion hits the 50 states, there’s time to think creatively and innovate outreach and education programs that bring new eligible people into the health insurance fold. That’s the consumer-facing aspect.
On the business workflow front, there’s the challenge of states and the health insurance exchanges: how will these mechanisms ensure that people don’t fall through the cracks, the analysis asks. There will be a grey area between the population that’s mandated to buy insurance who are currently uncovered, and those at or near the 133% federal poverty level. That’s some fuzzy math that may elude a lot of uninsured people, requiring a different kind of outreach and education from the state exchanges. The ACA talks about insurance navigators, and these market/access channelers will be important shepherds to overcome this particular challenge.
Without full enrollment of the 32 million who have the promise of health insurance through the ACA, the full realization of that promise — and the ability to get people into medical homes and continuity of care, thus driving better health outcomes and lower costs over the long term — will continue to elude the U.S. health system and taxpayers.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...