 In October 2012, Stage 2 of the HITECH Act’s meaningful use begins. That means that providers, both hospitals and physicians, who adopt electronic medical records systems and are looking to receive a financial incentive from the ARRA stimulus funds, must meet criteria defined as “meaningful use” (MU). Stage 2 will feature standards for providers to communicate health information to patients, based on the draft set of criteria issued by the U.S. Department of Health and Human Services.
In October 2012, Stage 2 of the HITECH Act’s meaningful use begins. That means that providers, both hospitals and physicians, who adopt electronic medical records systems and are looking to receive a financial incentive from the ARRA stimulus funds, must meet criteria defined as “meaningful use” (MU). Stage 2 will feature standards for providers to communicate health information to patients, based on the draft set of criteria issued by the U.S. Department of Health and Human Services.
Will providers be ready to put patients in the center of the EMR?
PricewaterhouseCoopers assesses the complex answer to this question in their report, Putting patients into “meaningful use, published in February 2011.
PwC’s key findings were that:
- Engaging external constituents may postpone achieving “meaningful use.” Providers who have adopted HIT and are deep into implementation have begun to understand just how much time is involved to meet MU.
- Patient awareness of and access to available health IT tools is low; social, expectation, and education hurdles exist. Currently just 14% of U.S. health consumers access medical records electronically according to PwC’s survey. Consumers are largely unaware of the technology, and adding to the confusion is the blurring between EHR, EMR, PHR, and patient portals.
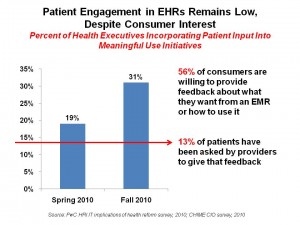
- Patient engagement in MU initiatives is low, despite consumer interest. While nearry 1/3 of health systems are using patient input in MU projects, an increase from 19% last year, only 13% of consumers say they’ve been asked to provide input.
- “Meaningful use” has yet to call for measuring the level of patient engagement. There’s no written standard to gauge how much patients are engaging in health IT. ONC, PwC says, intends to incorporate such a standard into Stage 2. David Harlow of the HealthBlawg noted to PwC that the Society for Participatory Medicine, among other organizations, has asked for more consumer-centricity in MU.
- Health systems need to compete for consumers in the PHR market. “There may be stiff competition for consumers’ attentions” for personal health records, PwC foresees. PHRs haven’t been adopted by most health consumers; only Kaiser Permanente and the VA (via MyHealtheVet) have significant traction among patients. Overall, commercial PHRs account for only 6% of the market (e.g., Google Health, Microsoft HealthVault, and others who share that slight slice of pie). But PHRs are a key building block for patient-centered meaningful use. And these need to be easy to use, well designed, and connected to providers’ EHRs so that patients don’t have to directly enter data themselves.
PwC offers several recommendations to make patients central to EMR adoption. First, the “face” of the EHR should be the patient or an advance-practice nurse in the primary care practice. Second, providers and patients need to agree on what “active participation” looks like in health care vis-a-vis health IT tools. Third, get the family involved. Fourth, design PHRs with patients.
Health Populi’s Hot Points: There’s a gap between what health-engaged consumers want and what providers are delivering at this early stage of HITECH/MU implementation, based on the data presented in the chart. While over one-half of U.S. adults would be willing to provide feedback into EMR design and use, only 13% of people have been asked to do so.
 This disconnects the ultimate consumer of health care, the patient, from the design of a consumer health portal or personal health record. Doing so most often results in a Field of Dreams effect, where even the most earnest of IT developers builds an application with the best of intentions, but without end-user input, the app is built and users don’t ‘come.’
This disconnects the ultimate consumer of health care, the patient, from the design of a consumer health portal or personal health record. Doing so most often results in a Field of Dreams effect, where even the most earnest of IT developers builds an application with the best of intentions, but without end-user input, the app is built and users don’t ‘come.’
Patient awareness of health IT tools remains low, so while meaningful use seeks patient-connectivity and -centricity, there’s a big job to be done in patient education on what EHRs, PHRs, and health data access for personal use and health engagement. The Keystone HIE project associated with the Geisinger Health System in Pennsylvania recently found that consumers in the community didn’t know much about the health information exchange; James Younkin, director of the HIE who is the IT director at Geisinger, said, “Most consumers don’t have a clue what HIE means. We need to clarify what we are doing to assure their privacy.” The HIE will enable patients and providers to communiciate via secure messaging once it’s in place.
The Consumer Partnership for eHealth and the Campaign for Better Care, which are coalitions of consumer, patient and labor organizations in the U.S., wrote ONC on February 25, 2011, their comments for Meaningful Use Stage 2. The letter articulate 4 areas where consumers will play key roles in “using information to transform our health system:”
- Acting as Agents of Change
- Making Informed Decisions
- Verifying Facts and Providing Context
- Integrating Better Health into the Full Context of our Lives.
A new component to consider, the coalition wrote, is the role of consumers as “sources of verification and contextual information.” This is where a person’s health engagement can really make a difference in ensuring the information in the health record is correct, and add personal observations of daily living which are not captured in clinical encounters in hospitals or doctor’s offices.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...