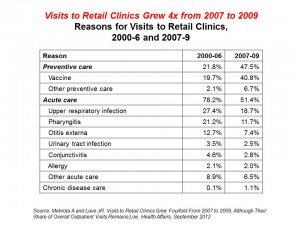
 There were nearly 6 million patient visits to retail health clinics in 2009. Such visits to retail clinics rose four-fold between 2007 and 2009, according to a RAND study published in the September 2012 issue of Health Affairs. Visits for prevention versus acute care in 2009 were roughly evenly split, with 47.5% and 51.4% of people over 18 seeking prevention vs. acute care from retail clinics, respectively. The most common acute care complaints in the retail setting were upper respiratory infections, pharyngitis, otitis externa, conjunctivitis, urinary tract infections, and allergies.
There were nearly 6 million patient visits to retail health clinics in 2009. Such visits to retail clinics rose four-fold between 2007 and 2009, according to a RAND study published in the September 2012 issue of Health Affairs. Visits for prevention versus acute care in 2009 were roughly evenly split, with 47.5% and 51.4% of people over 18 seeking prevention vs. acute care from retail clinics, respectively. The most common acute care complaints in the retail setting were upper respiratory infections, pharyngitis, otitis externa, conjunctivitis, urinary tract infections, and allergies.
What’s underneath the impressive rise is important to parse out because it’s not all acute care visits that are growing. The retail health clinic is becoming a major focus for immunizations, other preventive encounters, and chronic disease care.
Also underneath the big growth finding is a pattern of use that’s particularly striking for older adults over 65 years of age: 82% of the visits to retail clinics among older Americans, 65 years of age and older, were for vaccines — namely, the influenza shot. Only 13% of visits among older people were for acute care reasons.
For younger people, though, under 18 years of age, retail clinics appear to function like medical homes for many young health citizens. 60% of visits to retail clinics among younger people were for acute care complaints, notably pharyngitis, urinary tract infections, upper respiratory infections, and sinusitis. There were similar patterns of retail health visits among people 18 to 64.
Health Populi’s Hot Points: Mehrota and Lave, the savvy researchers who produced this study, note that a significant proportion of retail clinic visitors lack a medical home, or have a weak tie to a primary care provider (PCP). What will happen when the Affordable Care Act begins to cover the uninsured? Will retail clinics fail or flourish?
It’s a good bet that retail clinics will grow in the short run as the ACA rolls out, and in the longer run due to convenience, access, and the community-based nature of retail clinics. As health consumers take on greater roles in paying for and selecting health care channels, services and tools, they want to access care that’s as convenient and engaging as products they demand wearing their “consumer” hat for travel, financial services, retail, and other aspects of daily life management.
Primary care can no longer be sited solely in the PCP’s office. There is a shortage of primary care providers that begs for new models of distributed primary care where people live, work, play and pray. For more on this issue, see my paper published by California HealthCare Foundation, Primary Care, Everywhere.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...