
One in two doctors is burned out. Physicians are seeing more patients in a day and spend less time with each of them. This leads to job burnout, and greater probability for medical errors and eventual liability challenges, along with feeling pushed toward early retirement.
In a study published in August 2012 in the Archives of Internal Medicine, Mayo Clinic researchers learned that physicians are more burned out than workers in any other profession. And those at greatest risk of “being on a hamster wheel,” as Dr. Jeff Cain, president-elect of the American Academy of Family Physicians describes the scenario, are primary care doctors.
With the implementation of the Affordable Care Act, primary care doctors will be on the front line of absorbing newly-enrolling patients into the U.S. health system. With primary care doctors already at greater risk of physician burnout, this sets the stage for further stress on this already-stretched and –scarce workforce.
Doctors in the U.S. are working an average of 10 hours more per week and are nearly two times likely to be dissatisfied with their work-life balance, according to the research.
While a severe personal problem for each of these physicians, the bird’s eye view over this finding reveals a problem with and for the U.S. health system. Greater administrative burdens, higher proportions of patient bad-debt, health plan scrutiny over clinical decisions, and more demanding patients challenging physician hegemony converge to drive doctors toward exhaustion.
Dr. Thomas Bodenheimer, professor at UCSF School of Medicine and a longtime analyst of the U.S. health system physician workforce, believes that the optimal number of patients for a physician practice panel should number 1,800 at a maximum. Yet the average PCP in the U.S. today is responsible for 2,300 patients. This drives physicians toward shorter patient visits, less time for evaluation and most importantly, less opportunity for engaged dialogue between patients and their most trusted partner in health: physicians. “When you have only 15 minutes per patient…you feel like you’re on a hamster wheel,” Dr. Bodenheimer told The Daily Beast/Newsweek in April 2012.
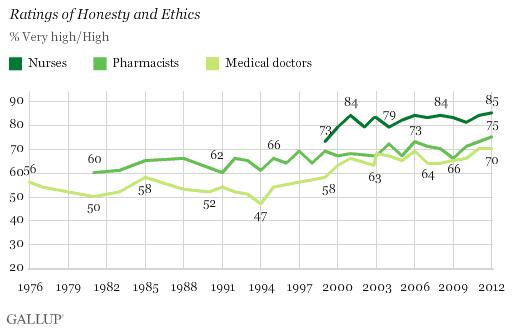 Gallup’s annual poll on honesty and ethics was released this week and finds that the top 3 most trusted professions are nurses, pharmacists, and physicians. Because trust is a precursor to health engagement, patients are pre-disposed to positive relationships with their physicians. But the exam room time-crunch militates against that objective. (For more on the Gallup poll, see Health Populi here).
Gallup’s annual poll on honesty and ethics was released this week and finds that the top 3 most trusted professions are nurses, pharmacists, and physicians. Because trust is a precursor to health engagement, patients are pre-disposed to positive relationships with their physicians. But the exam room time-crunch militates against that objective. (For more on the Gallup poll, see Health Populi here).
The result is sub-optimal patient care and compromised health literacy. A study by the Markle Foundation found that patients and doctors agreed that 30% of the time doctors forget information that patients told them. This is a concern because there is a direct relationship between how well the doctor and patient communicate and a patient’s overall health.
Health Populi’s Hot Points: Solving the time challenge for physicians and nurses – in particular, primary care providers – will require a multi-pronged solution that brings together:
– Payment that rewards clinicians organizing a medical practice that is patient-centric, promoting health literacy and patients’ good health choices (like medication adherence, lifestyle behavior changes and getting recommended clinical and diagnostic tests). Emerging models of care such as the patient-centered medical home and accountable care organizations will provide incentives for patient engagement and “slowing down” the clinical conversation when it’s necessary to do so.
– Team-based care, freeing the doctor’s time to see the sickest patients who require “laying on of hands and eyes” and the doctor’s diagnostic capabilities in real-time. This team reorganization will also drive greater shared decision making, which will also enhance patient engagement and greater clinical collaboration.
– Technology that bolsters efficiency, productive workflows, interoperable medical records, increasingly via mobile platforms at the point-of-care.
A critical aspect of that technology solution that supports the first two tactics is delivering high quality information at the point-of-care and at times when the clinician wants it. “With the use of mobile devices, physicians are able to multitask and integrate reliable information with their practice right at their fingertips,” observed Deborah Taylor, Assistant Professor and Acquisitions Library at the University Of Tennessee Health Science Center who recently tried out the ClinicalKey system from Elsevier. “Accessing information in this way leaves less room for speculation and lower risk of errors, increasing patient safety aspirations and goals,” she told me.
Time is the scarcest resource for physicians, so technologies that streamline helping them find the clinical answers they’re looking for will enhance work/life balance. Joseph Payne, Collection Development Librarian at Ohio State University Health Science Library, said that, “If users trust the source and they can find an answer quickly that matches their needs, they can move on faster. I hear all the time from researchers that, ‘I’ve been looking up these journal articles and I don’t have time find them all—it needs to be easier or I move on.’” Joseph chose ClinicalKey for the OSU Health Science Library to help clinicians, researchers and students gain fast access to the information they need – stat.
Stay tuned to my final Health Populi post on ClinicalKey in mid-December, when I’ll put all of the themes together that I’ve addressed in this special series of blogs, which has been sponsored by Elsevier. All opinions included are mine, based solely on my own knowledge and experience.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...