 If you’re meeting with a physician in the next week or two, put on your empathy hat: chances are, they are feeling burned-out.
If you’re meeting with a physician in the next week or two, put on your empathy hat: chances are, they are feeling burned-out.
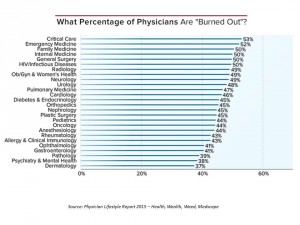
Overall 46% of physicians report they were burned out in 2014, up from just under 40% last year. Medscape’s Physician Lifestyle Report 2015 finds that at least one-half of physicians are burned-out who work in critical care, emergency medicine, family medicine, internal medicine, general surgery, and infectious disease (including HIV). And, at least 37% of physicians are burned-out working in all other specialties, shown in the first chart.
Medscape gauges doctors’ self-assessments of burnout with a lens on “health, wealth, and weed,” the report’s subtitle. Burnout is defined here as the loss of enthusiasm for work, feelings of cynicism, and a low sense of personal accomplishment — all of which can work against a physician delivering quality care.
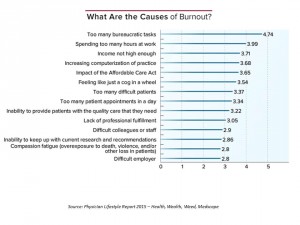
What’s causing this high incidence of job and lifestyle burnout? Physicians say its bureaucratic tasks, too many work-hours, insufficient income, “increasing computerization” of practice (THINK: health IT and EHR implementations), impact of the Affordable Care Act (which fell as a top burnout factor this year), feeling like a cog in a wheel, too many difficult patients, too many appointments in a day, and the inability to provide patients with quality care. Major stressors do not include being able to keep up with current research, or “compassion fatigue” (defined in this study as overexposure to death, violence, or loss of patients).
Some physicians appear to mitigate the risk of burnout with outside activities. Volunteering appears to have a positive impact on physician burnout: more doctors who admit to “never” volunteering are burned out. On the other hand, fewer physicians burn out who volunteer with religious organizations, do pro-bono clinical work, engage in tutoring/counseling, and perform international mission work. Exercise on a regular basis, too, yields lower incidence of burnout, according to the physician self-reports. It stems from this data point that more physicians with higher BMI (over 25) feel burnout.
It helps to be married, remarried, or widowed when it comes to burnout: more doctors who are single and living alone, or separated and living alone, feel burned out.
On the “weed and alcohol” front, it does not appear that burnout is correlated with daily substance use. Among those physicians who do use marijuana, the greatest proportion falls into the 56-65 year age cohort, with 25% of doctors 35 or under using weed.
Financial stress is an overall health risk, and doctors are real people, too. So it’s no surprise that more physicians who have minimal savings to unmanageable debt (39% with burnout versus 28% without) feel burnout compared with doctors who have adequate savings and more (66% without burnout versus 56% with).
 Health Populi’s Hot Points: Physicians’ feeling loss of autonomy in their work is a key factor for burnout, encompassed in the high-ranking causes of bureaucratic tasks, hours working, income not considered high enough, feeling like a cog in a wheel, too many patients in a day, and too many “difficult” patients.
Health Populi’s Hot Points: Physicians’ feeling loss of autonomy in their work is a key factor for burnout, encompassed in the high-ranking causes of bureaucratic tasks, hours working, income not considered high enough, feeling like a cog in a wheel, too many patients in a day, and too many “difficult” patients.
The implications for the growth of shared decision-making and prospects for partnering with increasingly health-engaged patients are significant – and not encouraging, based on the results of Medscape’s 2015 report. One-half of physicians feel burned out, stressed, unappreciated. Thus the aptness of the New Yorker cartoon by Robert Weber: “please try not to upset him,” your physician, the nurse requests of the patient.
Yet “upset” patients will: Dr. Eric Topol titles his latest book, The Patient Will See You Now, envisioning an uber-engaged health consumer disrupting physician workflow as we know it today. Of course, this is already happening: that physicians note EHR implementing as a key factor for burnout in 2015 is just one aspect of patient engagement, because real engagement happens once health data goes digital, liquid, and gets into patients’ hands. Checking off the “patient engagement” criterion for Meaningful Use is a data point. Engaging in shared decision-making and meaningful health engagement with patients-as-partners — that’s culture-and-workflow changing.
On the positive side, note that physicians who feel gratified with their relationships with patients have greater job satisfaction. Beth Israel Deaconess Medical Center’s OurNotes project, growing out of OpenNotes, is a step in this direction. We are at a fork-in-the-road in the doctor-patient relationship, with information technology enabling this new-and-improving relationship.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...