February may be American Heart Month, African-American History Month, and Marfan Syndrome Awareness Month. But based on the volume of studies and reports published in the past two weeks, ’tis also the season for talking mobile health and doctors. This Health Populi post trend-weaves the findings.
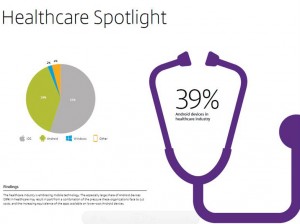 The big picture for mobile in health is captured by Citrix in its Mobile Analytics Report, dated February 2015. Everyday people are using mobile in work and daily living, blurring the distinctions between the various hats people wear. These roles, whether business or pleasure or life, happen 24×7, enabling through mobile platforms, Citrix found. The proportion of mobile health app subscribers using fitness apps doubled from 39% in 2013 to 78% in 2014, Citrix notes, with the busiest times for using between 5 and 7 pm. The top fitness apps in Citrix’s analysis were MyFitnessPal, RunKeeper, Runtastic, MapMyRun, LoseIt!, JEFIT Workout, Workout Trainer, and Nike. IoS platforms dominate mobile healthcare at 55%, with Android following at 39%.
The big picture for mobile in health is captured by Citrix in its Mobile Analytics Report, dated February 2015. Everyday people are using mobile in work and daily living, blurring the distinctions between the various hats people wear. These roles, whether business or pleasure or life, happen 24×7, enabling through mobile platforms, Citrix found. The proportion of mobile health app subscribers using fitness apps doubled from 39% in 2013 to 78% in 2014, Citrix notes, with the busiest times for using between 5 and 7 pm. The top fitness apps in Citrix’s analysis were MyFitnessPal, RunKeeper, Runtastic, MapMyRun, LoseIt!, JEFIT Workout, Workout Trainer, and Nike. IoS platforms dominate mobile healthcare at 55%, with Android following at 39%.

Looking further into the mobile health value chain, the MedData Group focused on physicians’ use of mobile in its report. 17% more physicians adopted mobile health tools between early 2014 and 2015. Physicians already using mobile platforms in health care have adopted them to primarily improve quality and continuity of care, save time, and improve patient communications. A lower priority for adopting mobile health are demands from patients (cited by 1 in 5 physicians), in Physician Adoption of Mobile in 2015, survey research from MedData Group. MedData polled 375 healthcare professionals in January 2015 to gauge their perspectives on mobile health.
The most-used health care apps physicians anticipate using in 2015 are ePrescribing (50%), accessing test results (48%), checking medication interactions (48%), using the EHR (38%), accessing diagnostic applications (31%), taking clinical notes (30%), and enabling telemedicine (21%). [Note: we are waiting to receive a correction from MedData for test results and medication interactions which were reported at 48% each in the company’s report, but medication interactions appears lower in the report’s chart on this datapoint]
In The Mobile Health Revolution, Smith & Jones report on the use of mobile tech by both patients and physicians. In a sidebar, the health care marketing agency recommends that health providers can engage patients of all ages by,
- Sharing health challenges via social networks like the provider’s Facebook or Twitter pages
- Asking patients to share daily exercise routines using hashtags on Twitter, and creating competitions for doing so, and
- Making tablets available in waiting rooms for calming patients, especially before procedures or challenging appointments.
Smith & Jones also suggest speaking to patients about the mobile apps they use and would recommend to other patients.
“Many smartphone applicatio![]() ns and wearable devices were accurate for tracking step counts,” asserted a letter to JAMA, published in the journal’s February 20, 2015, issue. The chart includes the two figures included in the article, based on research conducted among healthy adults 18 and over in August 2014. The devices tested included the Samsung Galaxy S4 Moves app; iPhone 5s apps for Moves, Health Mate, and Fitbit; Nike Fuelband; Jawbone Up24; Fitbit Flex, One and Zip; and the DigiWalker SW-200.
ns and wearable devices were accurate for tracking step counts,” asserted a letter to JAMA, published in the journal’s February 20, 2015, issue. The chart includes the two figures included in the article, based on research conducted among healthy adults 18 and over in August 2014. The devices tested included the Samsung Galaxy S4 Moves app; iPhone 5s apps for Moves, Health Mate, and Fitbit; Nike Fuelband; Jawbone Up24; Fitbit Flex, One and Zip; and the DigiWalker SW-200.
Health Populi’s Hot Points: It’s important to call out the fact that JAMA published two articles within one week of each other in February 2015 on mobile health: the week before the JAMA letter generally supporting wearable and app accuracy was published, the Journal published a viewpoint on mobile health titled Wearable Devices as Facilitators, Not Drivers, of Health Behavior Change. This was written by two of the researchers associated with the letter, along with a third author. In this opinion piece, their point is that, “If wearable devices are to be part of the solution [to driving health], they either need to create enduring new habits, turning external motivations into internal ones (which is difficult), or they need to sustain their external motivation (which is also difficult).”
The bottom line: most mobile health apps have not yet leveraged evidence-based health behavior theory. Changing health behaviors requires several steps: first, financing of the device; second, technical issues such as recharging batteries and remembering to wear them; third, ensuring the device accurately measures the behavior that it’s tracking, and then triggers a feedback loop of advice that can encourage the user; and, fourth, assuming accuracy, the feedback given the user would be designed to motivate and inspire them toward the behavior change, ongoing.
Citrix smartly points to the fact that people — which include doctors, and patients/consumers/caregivers — use mobile in living, working and playing. That the august Journal of the American Medical Association is covering digital and mobile health for its constituents to learn about, sitting side by side in the February 20, 2015 issue, with research on the treatment of asthma, displaying health care prices to physicians, choosing wisely, knowing HIV status in cancer treatment, educating patients on sickle cell disease, genetic testing and genomic medicine, and smoking cessation together point to the opportunity for mobile health to permeate health care. Patient care in every one of these areas will benefit from mobile platforms and digital health tools.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...