Cost is the major reason why Medicare Advantage plan beneficiaries switch plans, but people who switch also tend to have lower satisfaction scores based on non-cost factors. Those ratings have a lot to do with information and communication, according to J.D. Power’s 2019 Medicare Advantage Plan Study.
 The Study explores MA beneficiaries’ views on six factors:
The Study explores MA beneficiaries’ views on six factors:
- Coverage and benefits
- Provider choice
- Cost
- Customer service
- Information and communication, and
- Billing and payment.
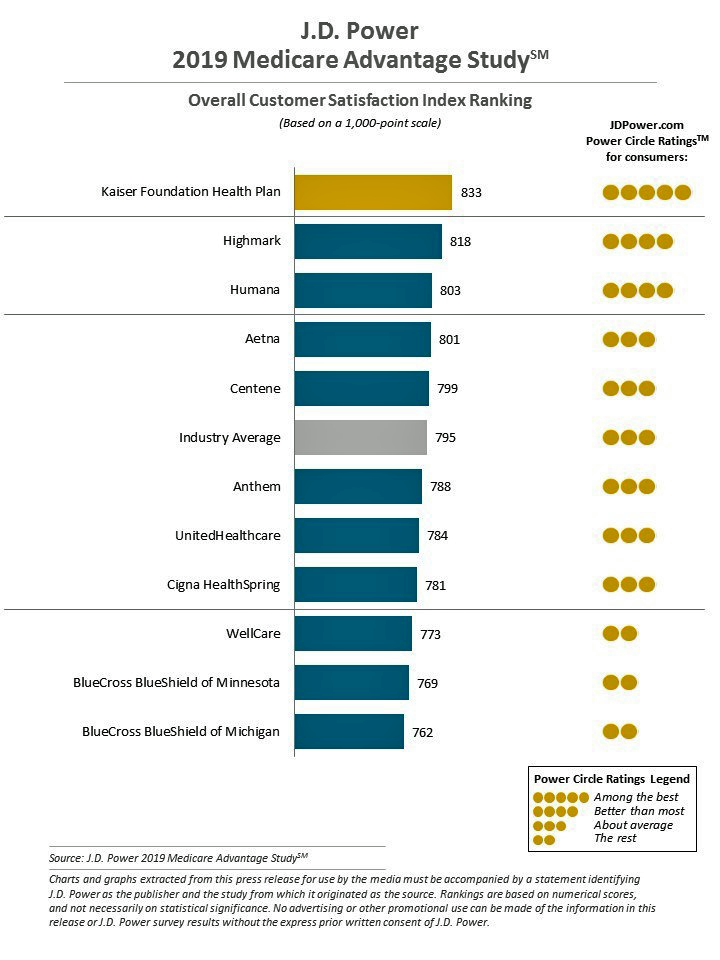
Kaiser Foundation Health Plan garnered the top spot for the fifth year in-a-row.
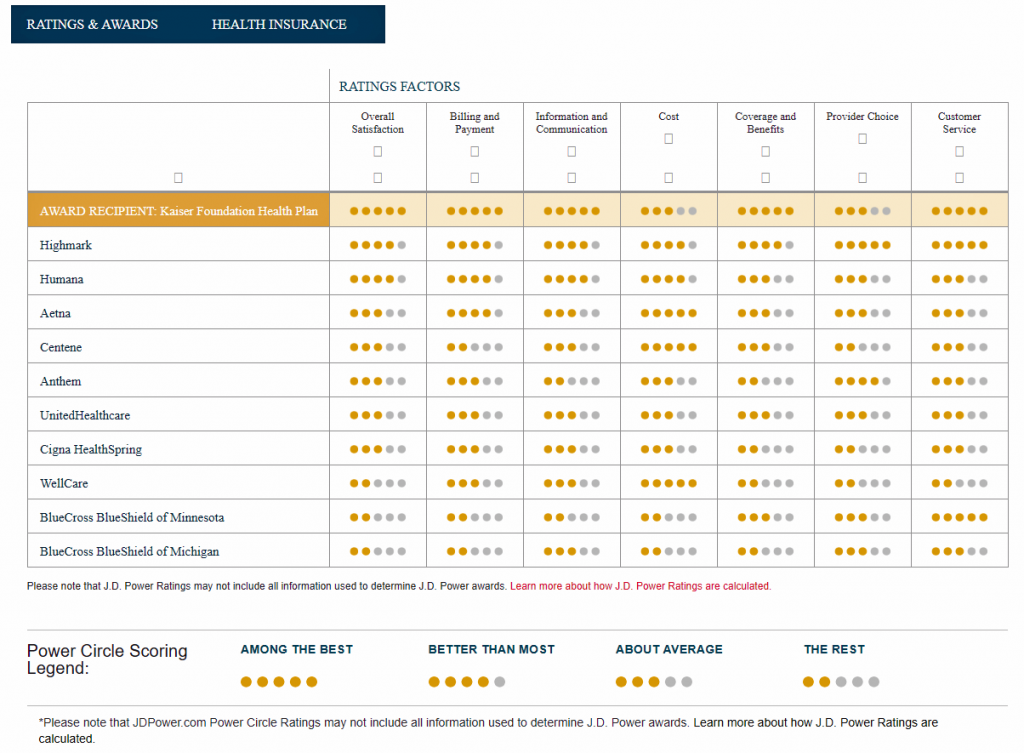
By feature, Kaiser achieved 5 “Power Circles” for all factors except for cost and provider choice, each of which earned only 3 Circles out of 5. The Power Circle detailed ratings are shown in the second chart from the J.D. Power study.
Highmark and Humana led the second tier of MA Plan satisfaction with four Power Circles. Each of these plans scored higher than Kaiser on cost, with Highmark the only plan studied earning five Circles, the maximum, for provider choice.
The plans studied in this 2019 report included Aetna, Anthem, BlueCross BlueShield of Michigan, BlueCross BlueShield of Minnesota, Centene, Cigna HealthSpring, Highmark, Humana, Kaiser Foundation Health Plan, UnitedHealthcare, and WellCare.
For the research, J.D. Power surveyed 3,233 members of Medicare Advantage plans in January through March 2019.
Health Populi’s Hot Points: “Even though health plans have been delivering a remarkably consistent customer experience, there is still room for improvement in the form of lower costs for seniors, proactive communication around explanation of benefits and helping members coordinate healthcare,” James Beem, J.D. Power’s Managing Director of Global Healthcare Intelligence, opined in the study’s press release.
J.D. Power defines the “information and communication” component as, “the usefulness of information, ease of understanding plan benefits and services, frequency of communications, and variety of communications.”
 Fewer than one in 10 Medicare Advantage beneficiaries told J.D. Power they have experienced the three sub-components that make up “information and communication.”
Fewer than one in 10 Medicare Advantage beneficiaries told J.D. Power they have experienced the three sub-components that make up “information and communication.”
As the J.D. Power study went public, so, too, did an announcement from AHIP, the advocacy organization for health insurance companies, launching a program called Project Link to address the social determinants of health.
A quote from Ghita Worcester, SVP Public Affairs and Chief Marketing Officer of UCare, points to the importance of and opportunity for personalization in health benefits to actually benefit an individual:
“At UCare, we know the health of our members is directly impacted by conditions where they are born, grow, work, play and age…We also recognize the need to tailor health improvement programs to meet the needs of all our members. Partnering with individuals and their diverse communities on solutions is fundamental to our mission of improving the health of our members through innovative services and partnerships across communities.”
Addressing the information and communications pillar, one of J.D. Power’s health plan satisfaction factors, is key to not only bolstering satisfaction but to that need to tailor health improvement programs that truly improve a beneficiary’s health. This isn’t just a matter of deploying information technology for technology’s sake, like a portal that isn’t based on how older people access, use and appreciate “information” or data. These platforms and programs have to be design-ful, inspired and built on peoples’ values, capabilities, natural life flows and goals.
Through AHIP’s Project Link, health plans may have another resource to inform and support efforts to improve communication that educates, informs and inspires older peoples’ health activation and sustained engagement, drives up satisfaction and — most importantly — improve the health of Americans as they age.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...