Wellness and disease prevention were the meta-themes at Health 2.0’s Spring Fling held earlier this week in San Diego. where the discussions, technology demonstrations, and keynote speakers were all-health (as opposed to health care), all-the-time. Dr. Dean Ornish told the attendees in the standing-room-only ballroom space that the joy of living is a greater motivator than the fear of death. And the 1.0 version of managing health risks has been more the latter than the former. As a result, Ornish’s two decades of research have shown that health is more a function of lifestyle choices than it is drugs and surgery. In fact, people have a “spectrum” of choices to make based on their personal preferences — not a one-size-fits-all “diet,” Dr. Ornish has learned.
While genes are our predisposition, they are not our Fate: good news for every human being. Furthermore, he said that, “healthcare needs more connection and community. It’s as important as food and water.” He and other researchers have learned that a person’s greater social connectedness (friends, family, community) contributes to better health. People who are lonely and depressed have 3 to 7 times greater mortality, Ornish told us. The largest unmet need is for intimacy and connection.
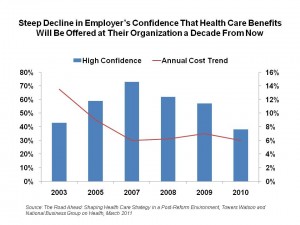 While Dr. Ornish’s research continues to demonstrate the power of lifestyle changes on health and longer, more joyful living, sponsors of health plans are now getting into a next generation of wellness and prevention in the context of value-based benefit design. With health premium increases that now have a family of four’s coverage indexed at nearly $20,000 per year based on the Milliman Medical Index, fewer employers are confident they’ll be able to cover employee health benefits a decade from now as the chart’s declining red line illustrates.
While Dr. Ornish’s research continues to demonstrate the power of lifestyle changes on health and longer, more joyful living, sponsors of health plans are now getting into a next generation of wellness and prevention in the context of value-based benefit design. With health premium increases that now have a family of four’s coverage indexed at nearly $20,000 per year based on the Milliman Medical Index, fewer employers are confident they’ll be able to cover employee health benefits a decade from now as the chart’s declining red line illustrates.
Thus, employers in 2011 are looking to link benefits with health and productivity, based on the Towers Watson and National Business Group on Health’s survey into employer-based benefits in the post-reform era. While companies will continue to offset increasing health costs to employees (with a 45% increase in employees’ share of health costs since 2006), they’re also using incentives more aggressively to motivate lifestyle behavior changes in a new-and-improved approach to wellness and prevention.
Employers’ priorities for worker health and wellness are first, to control costs; but second, to address emerging health risks and provide incentive programs to improve employee health and wellness, found by Towers Watson in last year’s report, Workforce Health Strategies. Addressing workers’ poor health habits, though, is the #1 challenge employers say they face to maintaining affordable health benefit cover, Towers says in the post-reform poll. 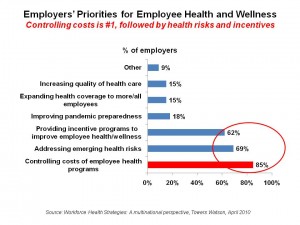 So they’re raising the bar on wellness incentives.
So they’re raising the bar on wellness incentives.
That’s the ‘supply side’ on wellness. What about consumers’ demand side — that is, will they indeed engage with their health and buy into lifestyle changes? Well, “buy into” may be the right phrase here, because employee’s contribution trends for health have hockey-sticked up from 2009, according to Aon Hewitt quoted in a Moody’s report on benefit plan changes from February 2011. Aon calculated that employees contributed $2,635 to average monthly premiums, deductibles, and out-of-pocket maximums in 2009; this increased to $4,149 in 2010, a 58% increase in one year.
In 2011, the value-based benefit design gurus are working hard to structure incentives that motivate workers to do the right thing by their health.
Health Populi’s Hot Points: It took Medicare 17 years to approve payment for Dr. Ornish’s program, which has hard data proving how to reverse heart disease through lifestyle — not via statins or stenting. This time lapse is not good news for either medical innovation, health economics, or peoples’ quality of life.
Will health benefit designers incorporate the learnings of Dr. Dean Ornish — that health is as much about social connectedness and joy as about picking the healthiest foods off of the spectrum of food choices and walking at least three times a week for 30 minutes? These psycho-social aspects have been a missing link in the health benefits world. Let’s hope it won’t take another 17 years for commercial health plans and employers to bundle in these important aspects into workers’ health benefits.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...