 With mobile health consumer market projections for ranging from $7 billion to $43 billion, according to PricewaterhouseCoopers, a casual reader might think that a plethora of health citizens are tracking their health, weight, food intake, exercise, and other observations of daily living by smartphones and tablets.
With mobile health consumer market projections for ranging from $7 billion to $43 billion, according to PricewaterhouseCoopers, a casual reader might think that a plethora of health citizens are tracking their health, weight, food intake, exercise, and other observations of daily living by smartphones and tablets.
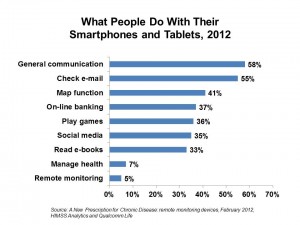
But as the chart shows, health self-trackers number around 1 in 20 U.S. adults, according to a survey conducted for HIMSS Analytics and sponsored by Qualcomm Life.
HIMSS Analytics’ report, A New Prescription for Chronic Disease: remote monitoring devices, was published in conjunction with the annual HIMSS conference which highlights the latest health information technology products and education. Last week’s meeting, held in Las Vegas, also included an exhibit with Qualcomm and several dozen health monitoring application companies.
HIMSS Analytics conducted 125 interviews with consumers in January 2012 to ascertain their views on mobile communications, health care and concerns about remote health monitoring via mobile. The concept of remote health monitoring was defined in this poll as, “a device worn by a person that transmits data into a database. An example might include a device you wear on your arm or wrist that measures your blood pressure and heart rate while running.”
 90% of the people said they have a smartphone and/or tablet computer. As the chart shows, the most popular uses of these devices are communication, e-mail, and map functions (think: personal GPS). Even though only 7% of people use the devices to “manage health” and 5% to monitor health, most people appear to be comfortable with the idea of using mobile devices for health-related purposes. Based on a scale of “1” to “7,” with 1 being not at all comfortable and 7 being very comfortable, HIMSS Analytics constructed indices for the following functions:
90% of the people said they have a smartphone and/or tablet computer. As the chart shows, the most popular uses of these devices are communication, e-mail, and map functions (think: personal GPS). Even though only 7% of people use the devices to “manage health” and 5% to monitor health, most people appear to be comfortable with the idea of using mobile devices for health-related purposes. Based on a scale of “1” to “7,” with 1 being not at all comfortable and 7 being very comfortable, HIMSS Analytics constructed indices for the following functions:
- Looking up health information, 4.89;
- E-mailing physicians, 4.61;
- Entering health information for personal use, 4.06; and,
- Entering health information for a physician, 4.02.
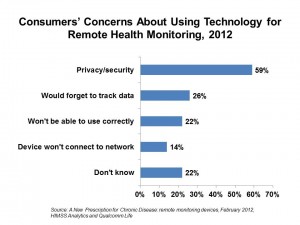
While these are half-way comfort indices, the survey learned that consumers have several concerns about using technology for remote health monitoring — most notably, concerns about privacy and security, cited by 59% of people. The second-most significant concern is one’s ability to remember tracking data, followed by doubts about using the device correctly.
Network concerns, whereby the device could communicate back to the clinical “mothership” and send data successfully through the cloud or other connection were noted by 14% of consumers. This connectivity concern was the most important barrier cited by health IT executives with whom HIMSS Analytics spoke.
Health Populi’s Hot Points: HIMSS Analytics is right to point out that, “for remote monitoring devices to be successful, patients need to be compliant and enter data/take measurements as prescribed by their caregiver.”
About one-half of doctors (65% of PCPs and 54% of specialists) would be interested in monitoring patients outside of the hospital, found by PwC in their 2010 physician survey. Thus, at least one-half of health providers are teed up, theoretically, to add remote health monitoring to their workflow.
What about consumers? While they tend to have seen monitoring technology for “jocks” (athletes), most people are still unfamiliar with quantified-self devices for the consumer market. One-half told PwC in 2010 they would not buy mobile health technology. 20% said they’d buy mobile tech to monitor fitness and wellbeing, and 18% of people would have their doctor monitor their condition remotely.
There’s a gap of knowledge among consumers, about half of whom could probably be persuaded to self-monitor, or allow their physician to monitor a health condition.
There’s also a health plan literacy gap, where American have been slow to connect the dots between the “nudges” their health plans are signalling to them through increasing co-pays and wellness incentives, and essentially owning their health status and outcomes.
When we can get to aligned incentives between patient-consumers and providers in accountable care, there will be greater teamwork both within the clinical care team and between that team and the patient – call it participatory health, participatory medicine, collaborative care.
Accountable care, whether write in capital letters or small, is on the way. That’s when payment will put providers and patients on the same page, fanning the adoption of remote health monitoring. This won’t happen overnight, but more patient-consumers will be nudged to use remote monitoring devices — and some will also have them prescribed by their physicians.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...