 About 50% of women and men in the U.S. are projected to be obese by 2030. The majority of people in America concur that the nation has an obesity problem. What’s been unknown and underestimated is just how much the epidemic is costing the nation in both health and financial terms. On a life-cycle basis, the cost is much greater than previously estimated.
About 50% of women and men in the U.S. are projected to be obese by 2030. The majority of people in America concur that the nation has an obesity problem. What’s been unknown and underestimated is just how much the epidemic is costing the nation in both health and financial terms. On a life-cycle basis, the cost is much greater than previously estimated.
Assessing the Economics of Obesity and Obesity Interventions from the Campaign to End Obesity looks at the evidence on the size of the obesity challenge, spending, and interventions available to combat this public health behemoth.
“Obesity is not just about added costs to our already-straining health budgets,” the report states. “Obesity also creates real challenges to our overall economy, to the public health, and to our national security.”
“National security?” you ask? The military and Pentagon spend $1 billion dealing with weight issues among personnel. This creates recruitment and retention challenges for the service. So, yes, obesity is also a national security problem.
The authors of the paper write, “the more we look into the costs of obesity, the more daunting they appear.”
The economics of obesity impact worker and company productivity, and the long-term fiscal health of the nation. The Congressional Budget Office (CBO), which advises U.S. policymakers on the financial implications of policy, hasn’t taken into account costly downstream complications that result from obesity beyond the 10-year timeframe that CBO uses in budget projections. Thus, the “health deficit” portion of the U.S. long-term budget deficit could be even deeper than previously calculated. This is why the report recommends that the CBO expand their forecast period to 25 years — 15 years beyond the current 10-year paradigm.
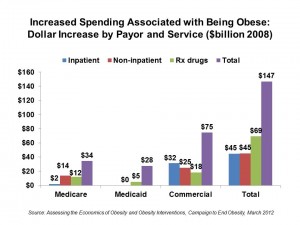
In current terms, the medical burden of obesity has risen to 10% of all medical spending, estimated at $147 billion in 2008, as the charge shows. What’s most stunning on this graph is the prescription drug line-item, where obesity added $69.3 billion to the U.S. health care bill in 2008. Cawley and Meyerhoefer found that prescription drug spending is 249% higher in obese individuals than for people of normal weight.
Health Populi’s Hot Points: The economic bottom-line (pardon the pun) on obesity is: consider life-cycle costs throughout a person’s life. Downstream health consequences of being extremely overweight translates into very poor health, multiple morbidities, disability, and greater downstream costs…not to mention sub-optimal quality of life for individuals and their families.
How to solve the problem and end obesity? The paper points out five intervention approaches: school-based interventions, community-based, pharmaceutical, surgical, and workplace. Each of these has examples of sound evidence-based models that can be deployed in the U.S., if funding can be artfully designed to motivate providers and patients to be on the same page in addressing the obesity epidemic.
This approach speaks to health, where people live, work, play and pray. The obesity epidemic isn’t only about food: it’s about How We Live in America. Health providers must join in their community health ecosystems, beyond “care” processes into schools, workplaces, churches, pharmacies, grocery stores, and urban and transport planners to migrate, over time, toward becoming Healthy Communities.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...