 Mobile technology will change the delivery of health care, according to 2 in 3 health IT execs polled in the 2nd Annual HIMSS Mobile Technology Survey, sponsored by Qualcomm Life. Only 2% of health IT management says mobile won’t impact the delivery of health care in the future.
Mobile technology will change the delivery of health care, according to 2 in 3 health IT execs polled in the 2nd Annual HIMSS Mobile Technology Survey, sponsored by Qualcomm Life. Only 2% of health IT management says mobile won’t impact the delivery of health care in the future.
This week finds the mHealth Summit convening in Washington, DC, hosting some 3,000 interested stakeholders looking at the intersection of mobile devices and platforms and health and health care. The 2012 theme is Connecting the Mobile Health Ecosystem, and the exhibitor area of the Summit speaks to the broadening of that ecosystem, including health IT companies, innovative health providers, every major telecomms provider, apps developers and tech innovators, industry suppliers such as Johnson & Johnson and Pfizer, health lawyers (THINK: HIPAA, privacy and security), and government agencies all involved at the intersection of health and technology.
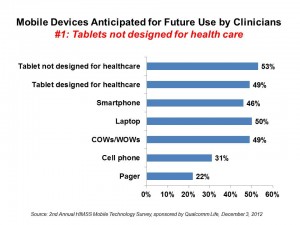
The topline finding is that 8 in 10 physicians use some mobile platform to delivery patient care: from smart phones and laptop computers to tablets (both generic and those designed for health care) and workstations on wheels, mobile has come to health care to stay. While laptops and workstations on wheels are currently most widely used by clinicians, tablets are seen as fast-growing. In particular, the segment of tablet computers not designed for health care (THINK: iPad and Samsung Galaxy among others) are seen to grow most quickly — not tablets purposely designed for health care.
The pager is outdated: the device, once “the” sold mobile device seen on the belts of doctors, falls to last place in the HIMSS/Qualcomm survey, where only 44% of health IT execs say pagers will be dealt with in a mobile technology policy. It’s the other devices named in the previous paragraph that are getting attention these days.
The areas where mobile is expected to yield the most significant benefits are pharmacy management, continuity of care, resource utilization (e.g., access to supplies or medication utilization), and preventive support (e.g., wellness management).
mHealth is hot right now: this survey isn’t painting a Kubrickesque futuristic scenario. A plurality of health IT execs is looking to acquire various mobile platforms over the next year: 43% are looking at cell phones in next six months, 36% at tablets, 65% for laptops, and 28% for smartphones.
App development is firmly focused on tools for clinicians, not so much for consumers/patients. The most common use of clinical apps are looking up patient information (65% of those who use apps) or non-PHI information such as clinical guidelines (64% of those who use apps). Clinical notifications, like lap personnel receiving STAT lab data (52%), tracking work lists (45%), collecting data at the bedside (45%), and use for education and training (45%) are also the most used functions for mobile apps among clinicians.
The most commonly-cited constraints to using mobile platforms in health are lack of funding and budget (71%), lack of IT staff (51%), immaturity of vendors in the market (49%), inadequate privacy and security (43%), lack of standards and interoperability (42%), and limited incentives (42%).
For clinicians, privacy ranks as the top concern for using mobile tech in patient care, along with the speed of accessing data. But many benefits are also articulated by clinicians for using mobile tech:
- Improving access to patient information, 82%
- Improving access to reference information (e.g., Epocrates), 76%
- Ability to view/interact with date remotely, 73%
- Ability to enter/modify patient information using the device, 59%
- Ability to access clinical decision support tools, 54%.
The online and phone survey was conducted in October and November 2012 among 180 U.S. health IT executives working in hospitals, healthcare systems, ambulatory care, long-term care and military care facilities.
Health Populi’s Hot Points: As was the case with the phrase “eBusiness,” which is simply now “business” and communications transacted naturally across the world wide web, the phrase “mHealth” may soon be relegated to last year’s dictionary. That’s because “m” as a platform is becoming ubiquitous in health care. While mobile requires special attention be paid to issues of privacy, security and interoperability, the benefits of going mobile in health are becoming clearer: clinicians untethered by immobile desktop technology, the ability to pivot the screen towards the patient, and have more meaningful dialogue in the exam room with a patient. This supports a visual conversation, greater patient engagement, and potentially greater trust between provider and patient.
For patients, who aren’t directly addressed in the HIMSS/Qualcomm survey, the benefits of “m” are profound: empowering, distributed, democratic. Mobile health platforms help providers deliver care to underserved populations, as Dr. Patricia Mechael of the mHealth Alliance discussed in this morning’s keynote address. What she has seen successfully work in remote parts of Africa can translate to medically-underserved areas, from east Los Angeles to Appalachia.
Mobile can scale health delivery. The technologies are here and the developments continue. It’s the cultural, political, and professional issues that will constrain the adoption and growth of mHealth in the U.S.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...