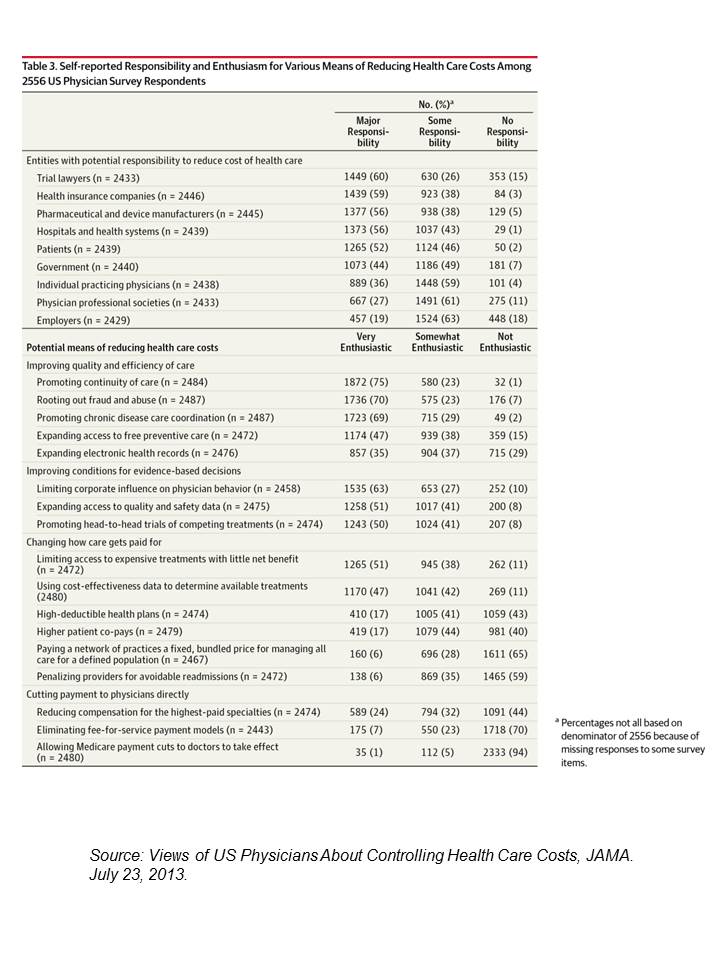
 When it comes to who’s most responsible for reducing the cost of health care in America, most doctors put the onus on trial lawyers, health insurance companies, pharma and medical device manufacturers, hospitals, and even patients.
When it comes to who’s most responsible for reducing the cost of health care in America, most doctors put the onus on trial lawyers, health insurance companies, pharma and medical device manufacturers, hospitals, and even patients.
But physicians themselves ? Not so much responsibility – only 36% of doctors polled said doctors should assume major responsibility in reducing health care costs.
And, in particular, most U.S. physicians have no enthusiasm for reducing health care costs by changing payment models, like penalizing providers for hospital re-admissions or paying a group of doctors a fixed, bundled price for managing population health.
Limiting access to expensive treatments that demonstrate little benefit, and using cost-effectiveness data to determine available treatments, are more palatable to physicians as methods to reduce health care costs.
In addition, doctors favor expanding access to quality and safety data, promoting head-to-head trials of competing treatments, along with rooting out fraud and abuse, and promoting chronic disease care coordination and continuity of care.
The bottom line: for doctors practicing in the U.S., managing health care costs is everyone else’s problem — even patients — not the physicians’, according to survey results published in JAMA, Views of US Physicians About Controlling Health Care Costs. This article is free and not behind the JAMA paywall and is required reading for people who want to understand ‘where’ physicians are in the health economics debate in America.
Health Populi’s Hot Points: There is a disconnect in physicians’ minds revealed in this survey in a question with which the physician respondent could agree or disagree: “Trying to contain costs is the responsibility of every physician.” 85% of the 2,556 doctors responding to this poll agreed, either strongly or moderately, with this statement.
But putting personal/professional skin in that game? That’s the province of patients, health plans, hospitals, lawyers…but not doctors themselves.
For physicians, managing costs is everyone else’s business…not theirs. “Physicians hold nuanced views about their perceived responsibility for health care costs,” the authors write. “Nuanced?” That’s an understatement.
There are big tensions in the profession today about:
- The organization and business model for physicians – how and whether to stay independent versus joining up in a larger group or become a hospital employee
- The nature of the work – is it more caring or more business and medical records implementation, less laying on of hands and cognitive skills versus more web-search and ePrescribing based on online formularies and clinical decision support systems
- The identity of the physician – do I deliver individual patient care or public health through population health management?
This survey clearly illustrates the current crisis in the medical profession. I facilitated an expert panel earlier this week (focused on health IT) where some physicians were at the table. When I elicited from the group current trends in physician practices, one doctor quickly offered, “physicians feel beaten up.”
In the transition from volume-to-value in health care payment in America, physicians will need support, on all fronts, to morph into this new world of payment. This may involve forging new identities, as well.
Postscript 7/24 1030am – Here’s an example of a health system that wants to reward, financially, physicians who coordinate care. So change can be rewarding as incentives re-align for value: Highmark’s Accountable Care Alliance.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...