A Month Until #CES2026 – The Journey to Our Personal Health Operating Systems

In a month, I’ll board a plane for Las Vegas to spend a week at CES 2026, the annual electronics conference that last year brought together over 140,000 global technology stakeholders to display, demonstrate, and sell the latest in consumer-facing tech. This will be my fourteenth CES (including the virtually convened meeting held in 2021). If you want to time travel, here’s a link to an early CES post featuring “The Battle of the (Wrist)bands.” Indeed, the digital health aisle at the time had many wrist-worn activity trackers, largely amped-up pedometers, with the likes
How Consumers’ Access to Telehealth Impacts Medical Real Estate and Design Decisions
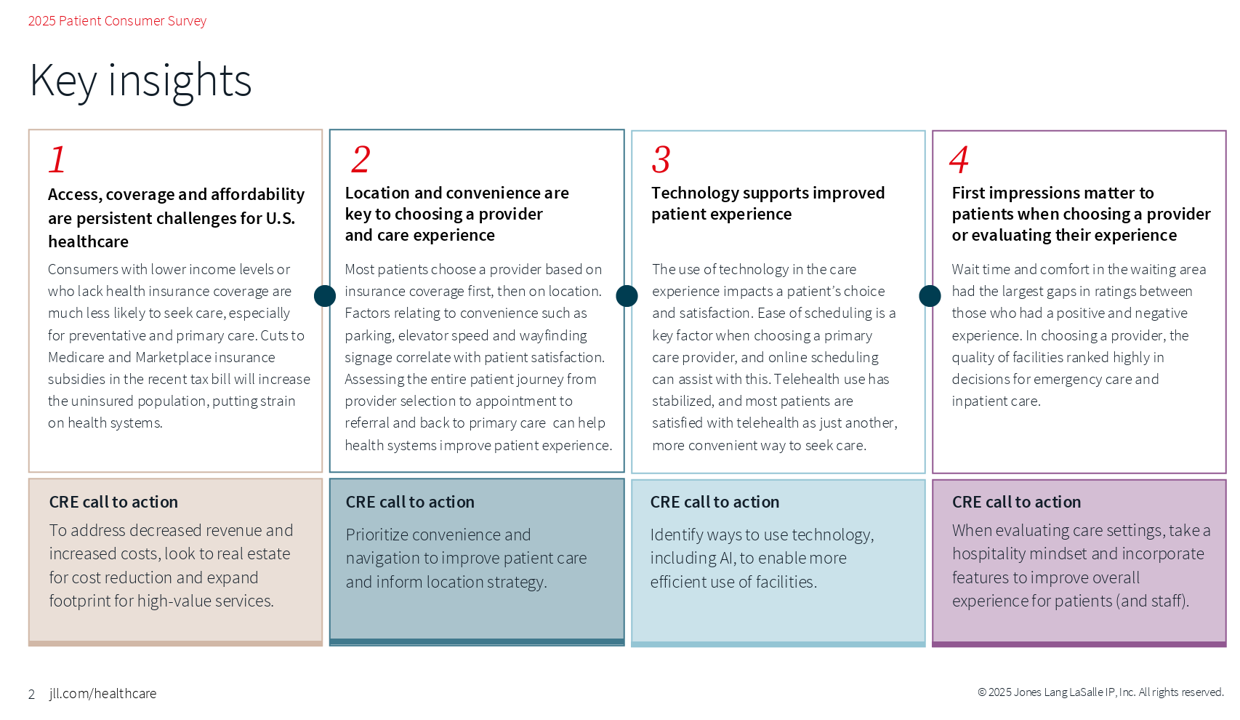
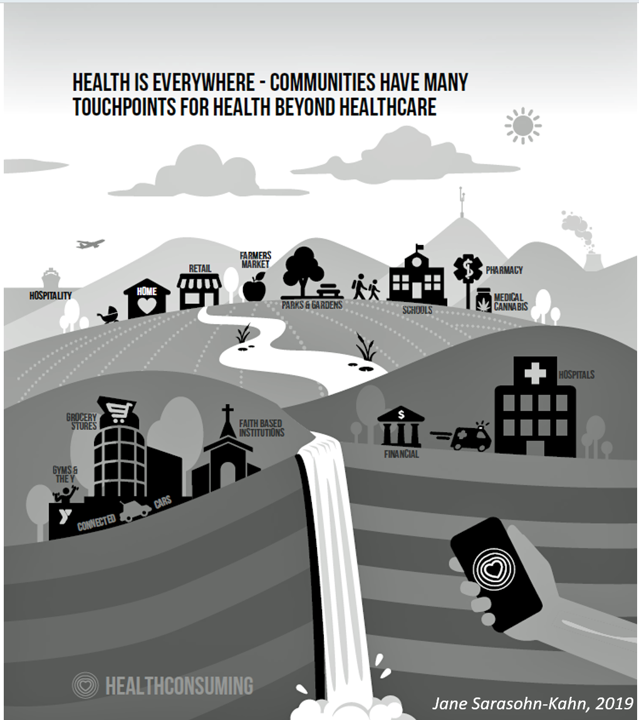
The idea of “hospitality” in health care is not new, but the nature of how patients-as-consumers are dealing with health care choices based on what looks and feels good is changing the nature of what hospitality means in technology-enabled health care delivery, we learn from the 2025 Patient Consumer Survey conducted by JLL. Jones Lang LaSalle Inc. (JLL) is one of the largest global commercial real estate firms with a strong portfolio of medical buildings. So it is worthwhile to track what the company is learning about health care delivery distributed both inside and outside of brick-and-mortar medical buildings.
In 10 Years, Health Care Will Happen Where Life Happens – PwC’s Tea Leaves into 2035
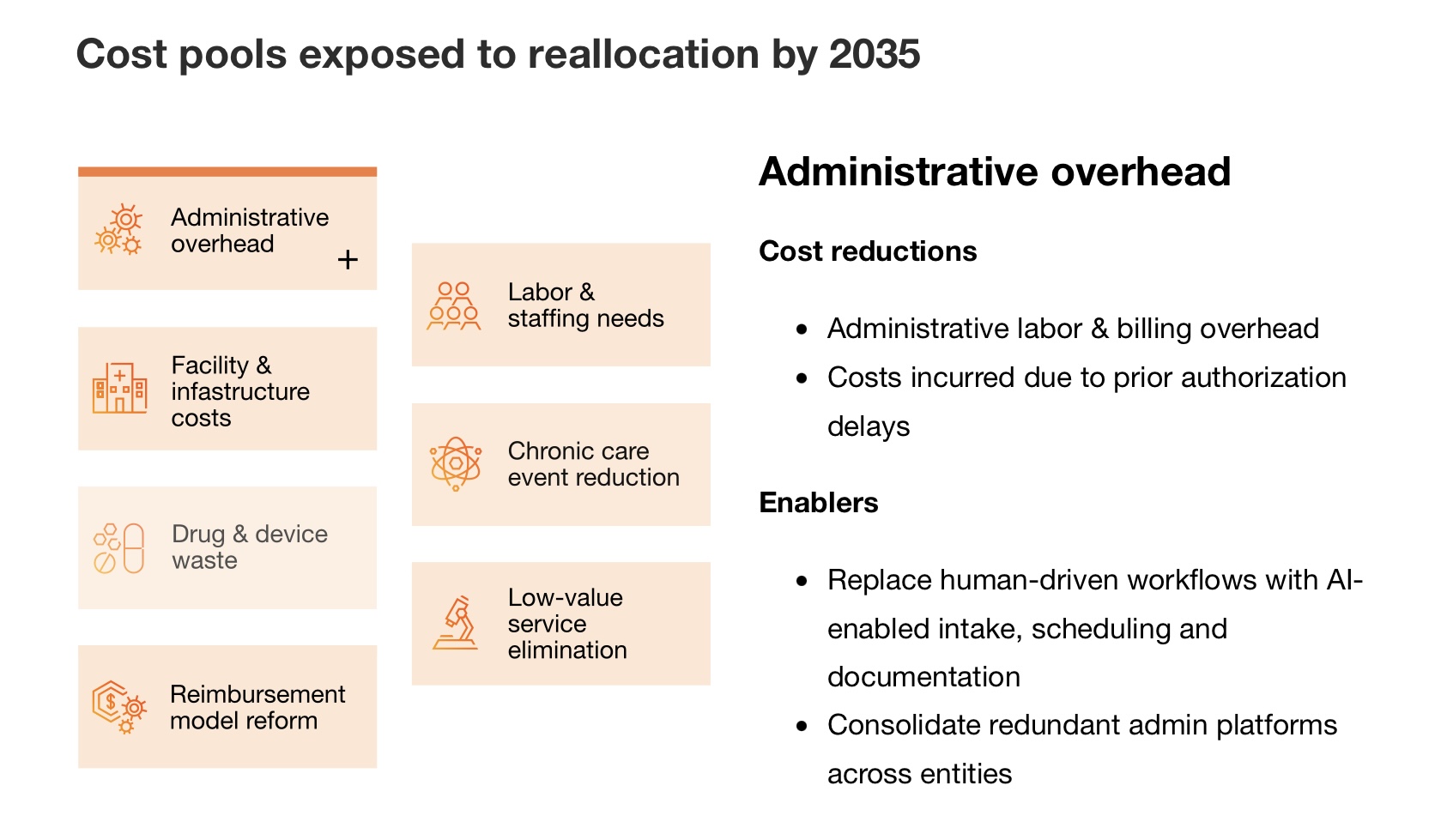
The costs of medical care are breaking the system, PwC asserts at the start of its new report on the $1 trillion opportunity to reinvent healthcare. The past 3 years of 8+% U.S. national health expenditure increases are “untenable,” PwC says, with 90% of that spending going toward patients with chronic and mental health conditions. What will transform the system and move us from “breaking point to breakthrough?” Biology and technology, PwC explains, with technology moving exponentially and simplifying care at scale, and biology decoding the “human operating system” enabling precision at scale. This
Expect Double-Digit Prescription Drug Trend Increases in 2026 – The Update from HUB International
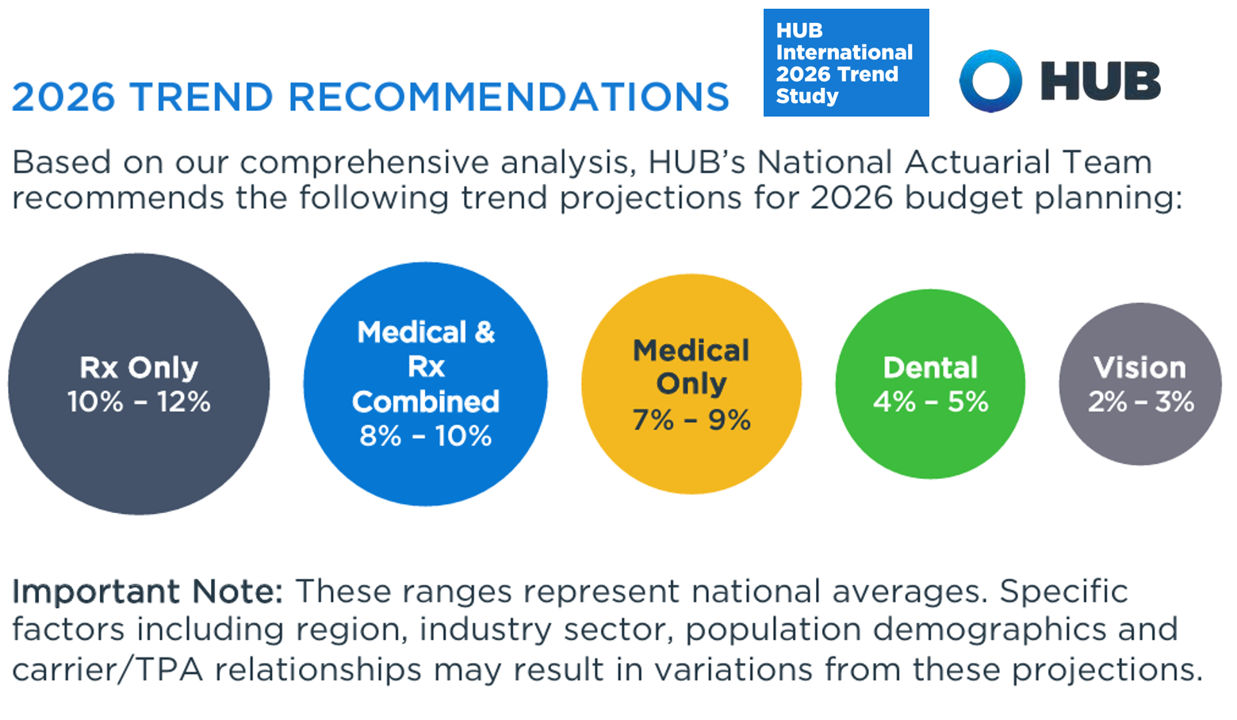
Prescription drug price trend for 2026 will be between 10% and 12% according to the 2026 Trend Study from HUB International, a global insurance and financial services firm. Here’s HUB’s line chart of the combined medical and Rx trend, illustrating nearly double trend growth since 2022 following the peak of 10.1% (combined) in 201 as patients returned to health care services and encounters when feeling safe in the fading out of the COVID-19 pandemic. That precipitous low-point in 2022 of 3.4% was the peak of the coronavirus stay-at-home period, representing the “medical distancing” felt across
National Health Spending in the U.S. in 2033: What 20.3% of the GDP Will Be Spent On
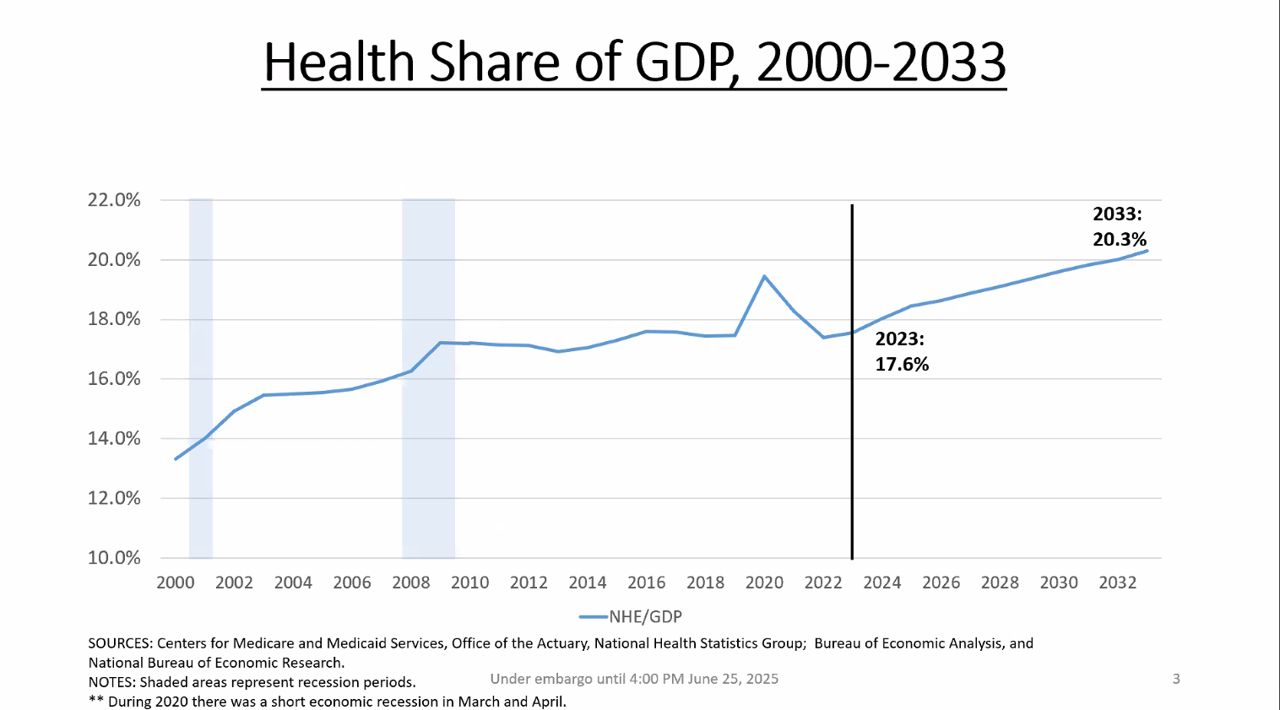
By 2033, national health spending will comprise 20.3% of the U.S. GDP, based on the latest national health expenditure projections developed by researchers from the Centers for Medicare and Medicaid Services (CMS). This growth will be happening as CMS projects coverage of insured people to decline over the period. Earlier today, I attended a media briefing hosted by Health Affairs to receive the CMS team’s top-line forecast of NHE from 2024 to 2033 discussing these findings. Fuller details on the projections will be released in the July issue of Health Affairs on 7
That Big Beautiful Bill’s Healthcare Proposals Aren’t So Pretty in the Views of Most People in the U.S. – Including Josh Hawley (R-Mo.) – Listening to the Kaiser Family Foundation June Health Tracking Poll

Across all U.S. voters, the so-called “Big Beautiful Bill” Act (BBB) is seen unfavorably by nearly a 2:1 margin. Underneath that top-line, Democrats, Independents, and non-MAGA Republicans oppose it, while MAGA supporters favor it. But favorability erodes when people hear about possible health impacts, we learn in the June 2025 Health Tracking Poll from the Kaiser Family Foundation. The details on views of the BBB Act are shown in the first bar chart, with overwhelming disfavor among Democrats and Independents, and majority unfavorability among non-MAGA GOP supporters. Next check into partisans’ lenses
A Toyota RAV4 Hybrid, a Playground Set, or Healthcare for a Family of 4: What $35,119 Can Buy in 2025 According to Milliman
If you went shopping for something that cost $35,119 in 2025, which would you most value? A new 2025 Toyota RAV4 Hybrid with some extras on board? A Canyon BYO playground set for your yard, school, or social-athletic club? Or, Healthcare coverage for a family of 4 in the form of a PPO? Welcome to this year’s 20th anniversary edition of the Milliman Medical Index (MMI), which I’ve looked forward to reviewing for most of its two-decade history. [You can read my annual takes on the MMI here in Health Populi by searching “MMI” and the year of publication in
Health Insurance Coverage Among Smaller U.S. Businesses Is Eroding: A Signal From JPMorganChase
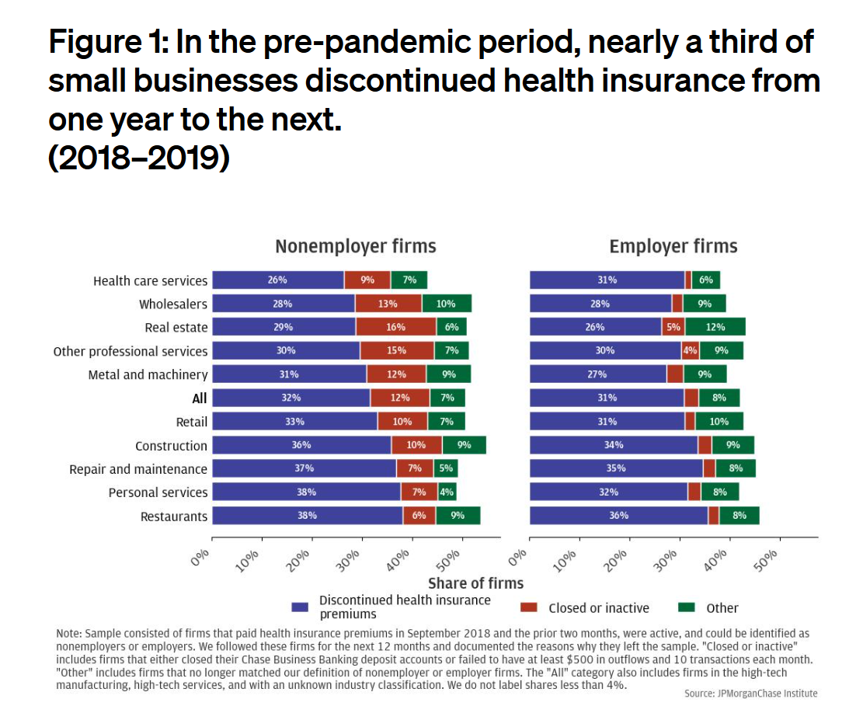
Working-age people in the U.S. depend on their employers to provide health insurance; just over one-half of people in America receive employer-sponsored health insurance. But a concerning signal has emerged that calls into question how sustainable the uniquely American employer-sponsored health plan model is: that is that one in 3 small businesses in the U.S. stopped covering health insurance after the worst of the pandemic health effects in 2023 as the companies payroll expenses continued to increase, a statistic raised in The consistency of health insurance coverage in small business: industry challenges and insights, a report from the JPMorganChase Institute
U.S. Health Care in 2025 Requires Scenario Planning: The Uncertainties (AI!?) That Inspire DIY Healthcare

As Weight Watchers prepares to initiate bankruptcy proceedings, I file the news event under “thinking the unthinkable.” “Thinking about the unthinkable” is what Herman Kahn, a father of scenario planning, asked us to do when he pioneered the process. In this book, for Kahn, “the unthinkable” was thermonuclear war, and the year was 1962. The book was tag-lined as “must reading for an informed public” and in it, Kahn I’ve been drawn back to this book lately because of a more intense workflow using
Are We Liberated Yet? Tariffs Can Impact Financial Health (Riffing on MoneyLion’s Health Is Wealth Report)
Americans’ financial health was already stressing consumers out leading up to Liberation Day, April 2nd, when President Trump announced tariffs on dozens of countries with whom the U.S. buys and sells goods. A new report from MoneyLion and Mastercard called Health is Wealth is well-timed for today’s Health Populi blog. The study was fielded by The Harris Poll online among 2,092 U.S. adults 18 and older between February 28 and March 4, 2025, so it was completed a month before the tariffs came to hit peoples’ 401(k) savings and employers’ company stock market caps.
Health Care Nation – How to Inspire a Rosa Parks Moment for Healthcare in America?
Tom Lawry may be best-known as a leading voice on AI in health care; after all, he’s written two very well-selling books on the topic, speaks all over the world on the subject, and in his most recent company-based gig helped lead Microsoft’s efforts in AI in health care and life sciences. When his publisher asked him to write a third book on AI in health care – still a hot topic in publishing – Tom said he’d rather turn to a subject long on his mind: the state of health care in America and how to change the conversation
Consumers Are Financially Stressed – What This Means for Health/Care in 2025
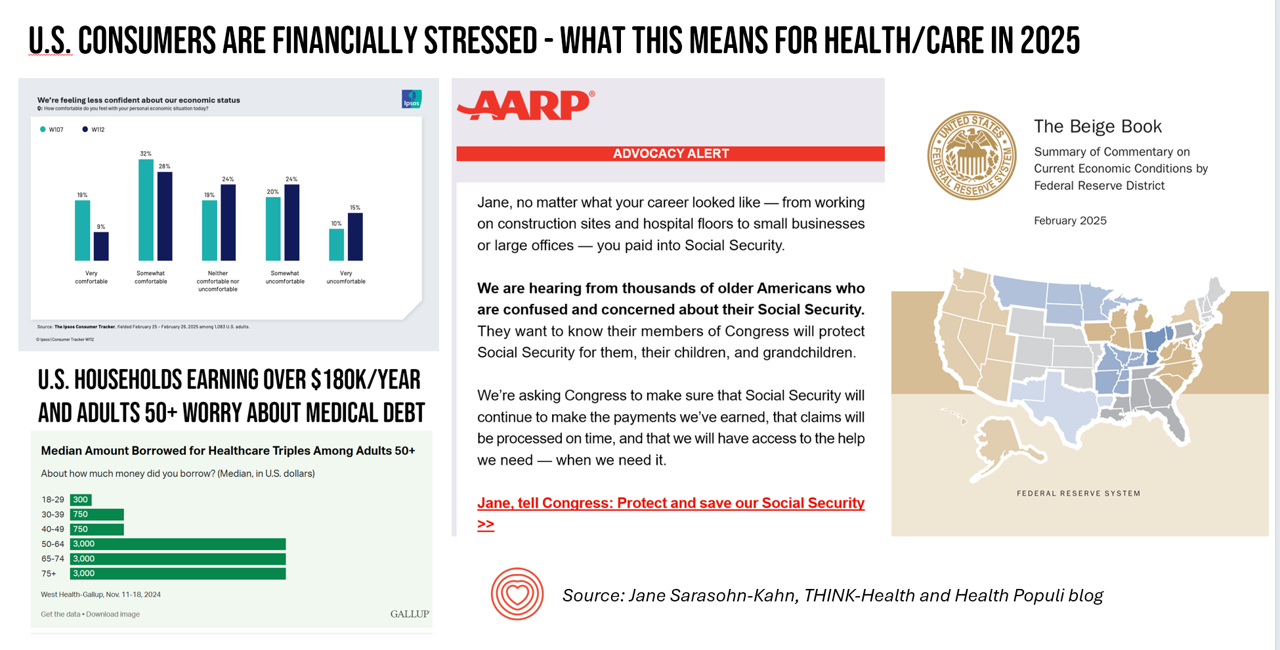
People define health across many life-flows: physical health, mental health, social health, appearance (“how I look impacts how I feel”) and, to be sure, financial well-being. In tracking this last health factor for U.S. consumers, several pollsters are painting a picture of financially-stressed Americans as President Trump tallies his first six weeks into the job. The top-line of the studies is that the percent of people in America feeling financially wobbly has increased since the fourth quarter of 2024. I’ll review these studies in this post, and discuss several potential impacts we should keep in mind for peoples’ health and
Think Quintuple Aim This Week at #HIMSS25
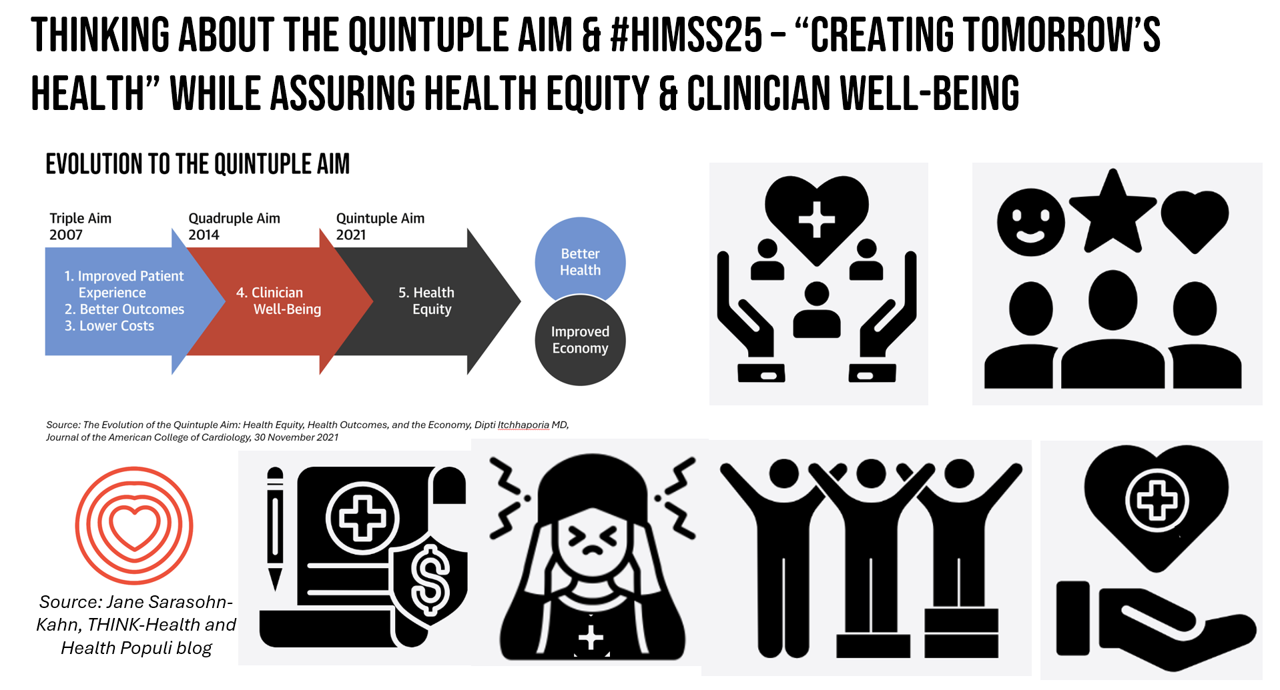
As HIMSS 2025, the largest annual conference on health information and innovation meets up in Las Vegas this week, we can peek into what’s on the organization’s CEO’s mind leading up to the meeting in this conversation between Hal Wolf, CEO of HIMSS, and Gil Bashe, Managing Director of FINN Partners. If you are unfamiliar with HIMSS, Hal explains in the discussion that HIMSS’s four focuses are digital health transformation, the deployment and utilization of AI as a tool, cybersecurity to protect peoples’ personal information and its use, and, workforce development. I have my own research agenda(s) underneath these themes
Telehealth, Right Here, Right Now: Calling on Congress to Vote for America’s Health and Well-being
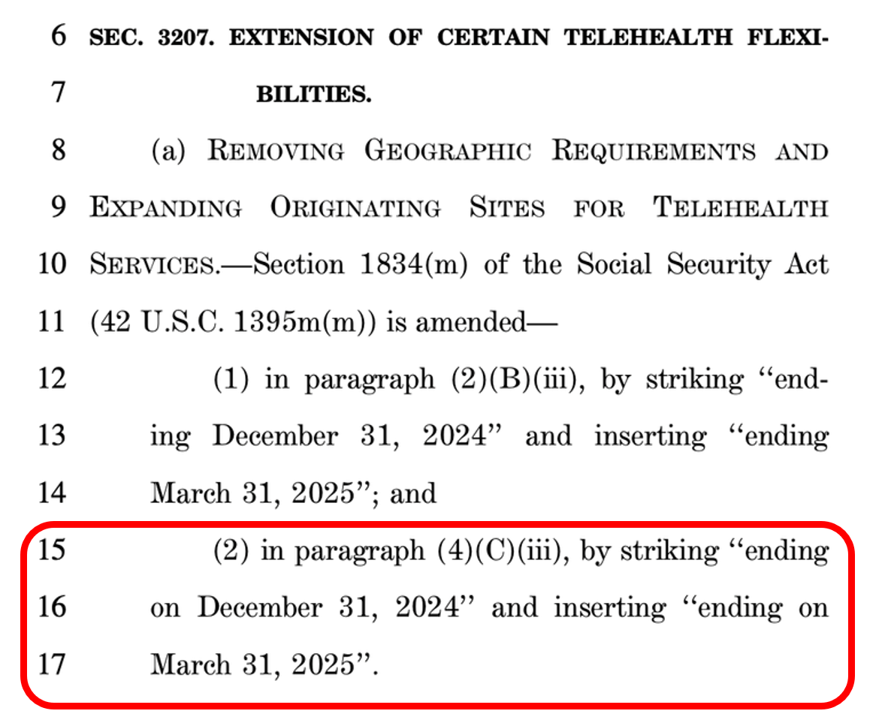
In the U.S., there are some issues that still unite most Americans in 2025. We can agree that, • The cost of eggs is too high • AI can be both exciting and promising at the same time as concerning • It sucks to have your personal data cyberattacked and breached, and, • Having access to telehealth is important. While I would be really sad to give up my omelets, I’m sticking a mindful toe into AI for some simple workflows, and I’m still dealing with the aftermath of the Change Healthcare data breach, it’s the looming telehealth deadline that’s
Some Bipartisan Concurrence on Health Care Issues in the U.S. – But Trust in Health Care Isn’t Bipartisan – KFF’s January 2025 Polls
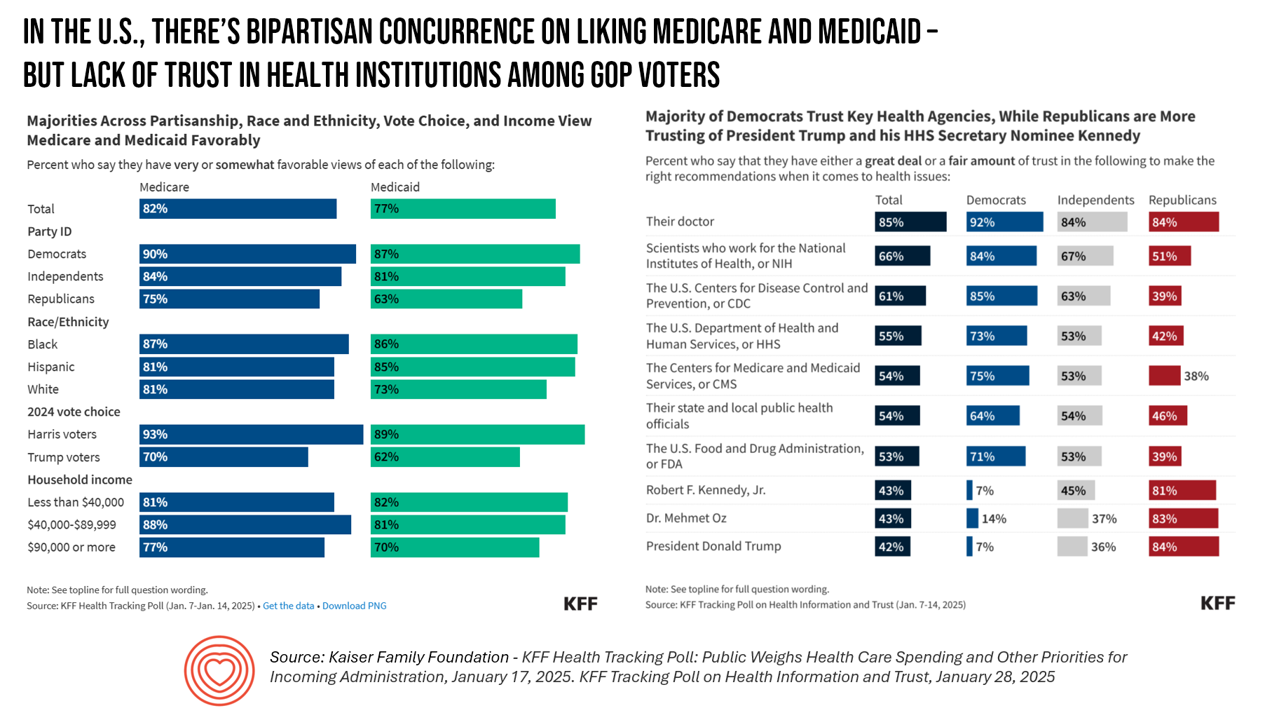
Two polls from one poll source paint at once a bipartisan and bipolar picture of U.S. health citizens when it comes to health care issues versus health care institutions in America. The Kaiser Family Foundation has hit the 2025 health policy ground running in publishing the January 2025 Health Tracking Poll last week and a poll on health care trust and mis-information yesterday. First, the health tracking poll which finds some concurrence between Democrats and Republicans on several big issues facing Americans and various aspects of their health care. As
Nurses Rank Highest in Honesty and Ethics in Professions Far Above All Other Work Roles in America – The Gallup Annual Survey 2025

While nursing has ranked top of U.S. professions for honesty and ethics for over a decade, U.S. adults speak even more assuredly in 2025 that nurses far outrank other professions in America. according to the latest Gallup Poll. The study summary report is titled, “Americans’ Ratings of U.S. Professions Stay Historically Low.” The data speak for itself — in 2025, the margin of people who put nurses on top of all other professions in America is much wider than in past years — and physicians have fallen further down
The Rough Guide to Health/Care Consumers in 2025: The 2025 Health Populi TrendCast
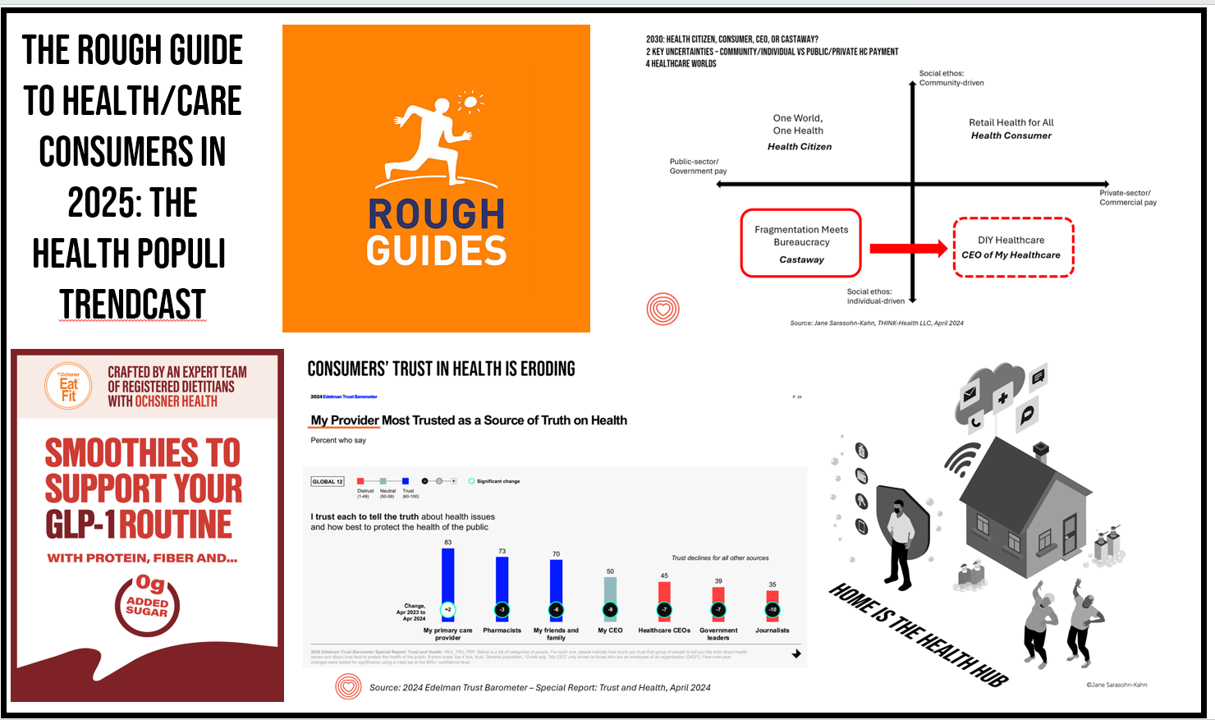
At this year-end time each year, my gift to Health Populi readers is an annual “TrendCast,” weaving together key data and stories at the convergence of people, health care, and technology with a look into the next 1-3 years. If you don’t know my work and “me,” my lens is through health economics broadly defined: I use a slash mark between “health” and “care” because of this orientation, which goes well beyond traditional measurement of how health care spending is included in a nation’s gross domestic product (GDP); I consider health across the many dimensions important to people, addressing physical,
National Healthcare Spending in the U.S. Was Nearly $5 Trillion (with a “T”) in 2023 – New Data from CMS
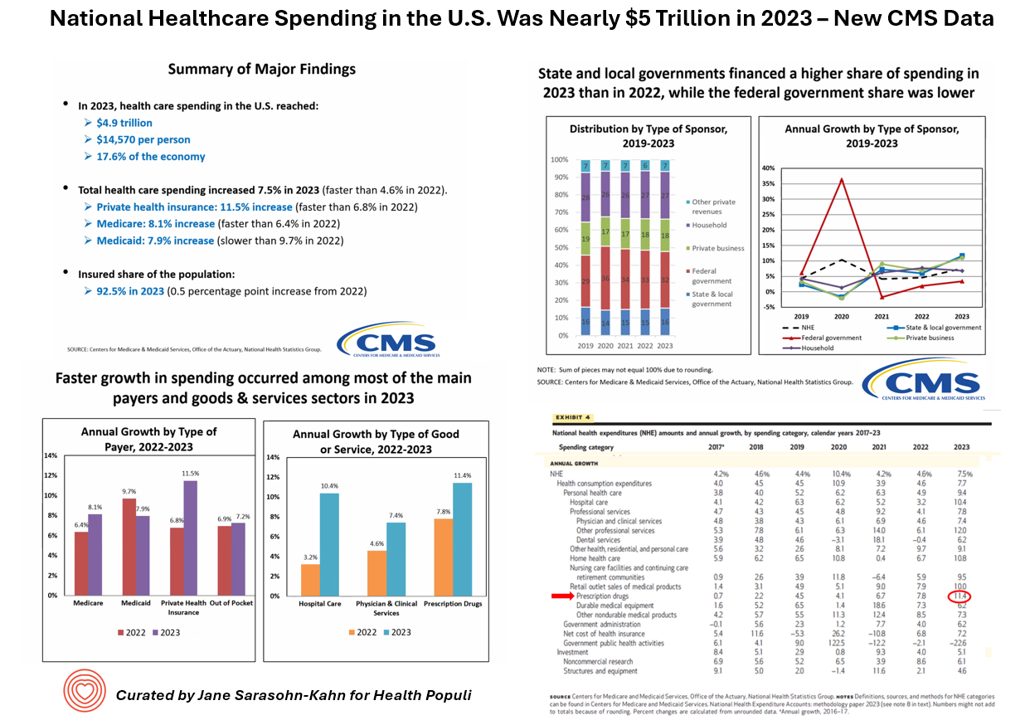
What would $5 trillion be valued around the world or on the stock market? The economy of Germany was gauged around $5 trillion in 2024. India could be the world’s 3rd largest economy by 2026 valued at $5 trillion. Nvidia could be a $5 trillion company in 2025, as could Amazon. But today we report out the latest data from the Centers for Medicare and Medicaid Services (CMS) that national health spending in America reached $4.9 trillion in 2023. The full report on national health expenditures (NHE) in the U.S. was published today in Health Affairs, which came off embargo
3 in 4 U.S. Patients Say the Healthcare System is Broken — But Technology Can Help
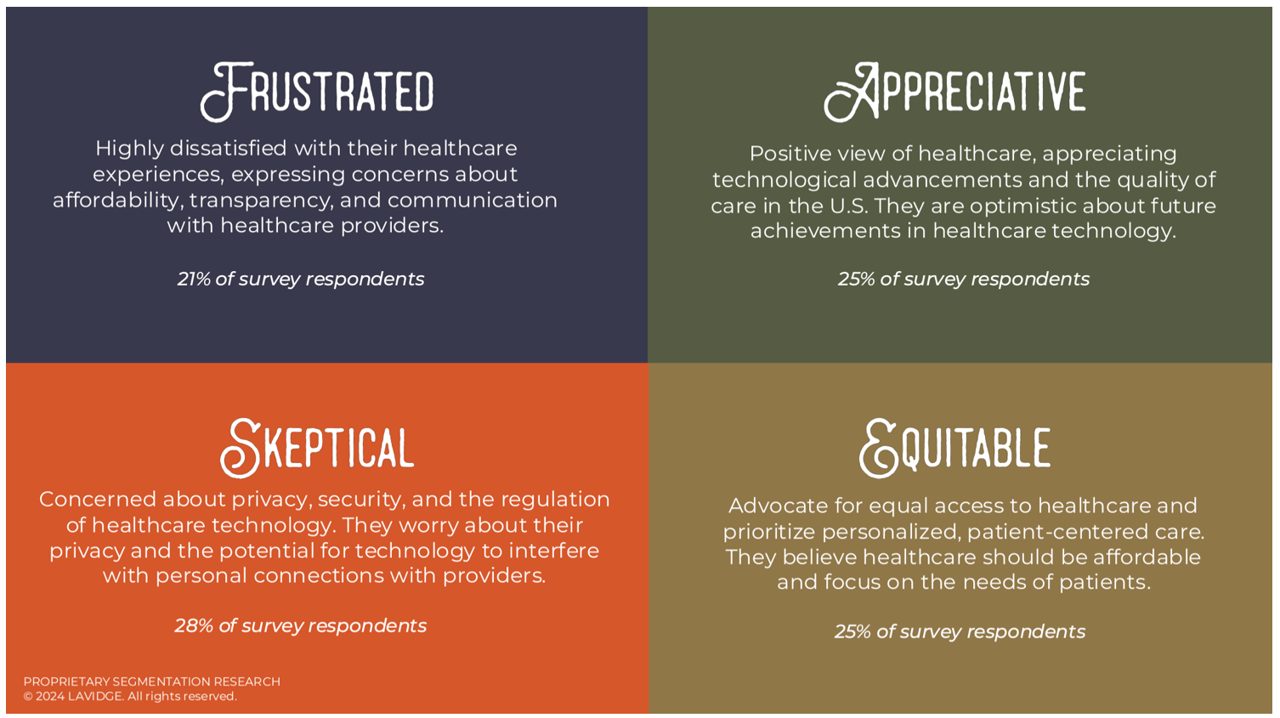
Patients “yearn” for personalized services and relationships in health care — optimistic that technology can help deliver on that hope — we learn in Healthcare’s Future: Balancing Progress and Perception, a health consumer survey report from Lavidge. Lavidge, a communications/PR/marketing consultancy, polled U.S. patients’ attitudes about health care and technology in June 2024, publishing the report earlier this month. Start with over-arching finding that, “Three out of four patients believe the U.S. healthcare system is broken and there is a strong sense of distrust,” Lavidge asserts right at the top of
Best Buy Health’s Latest Insights into Technology and Care at Home

In the U.S., aging in and staying at home is a priority for most people over the age of 45 — and for nearly one-half of younger people between 18 and 44 — we learn in Best Buy Health’s Research Brief discussing the company’s survey of 1,000 U.S. consumers. Best Buy Health, the health-focused operation which is part of the electronics retailer Best Buy, worked with Sage Growth Partners to assess 1,000 U.S. consumers, 18 years and over, on their perspectives on health care, technology, aging in place, and caregiving. The research was fielded
How Voting Plays Into Health, Health Equity, and Community Well-Being

“Voter registration in hospitals is the new frontier in health care.” That’s the headline in a WBUR story last week detailing the efforts of health care professionals in “amplifying” their patients’ voices inside and outside of the hospital walls by advocating for their health citizenship — through voter registration and public health policy advocacy. I’m a long-time evangelist for health citizenship and the role that a person’s engagement in the civic commons plays in one’s own health, the health of their communities and of the nation as a whole. I’m not alone
Health Information Security – My Interview with Richard Kaufmann, CISO of Amedisys, Part 3: The Futures of Cybersecurity in Healthcare
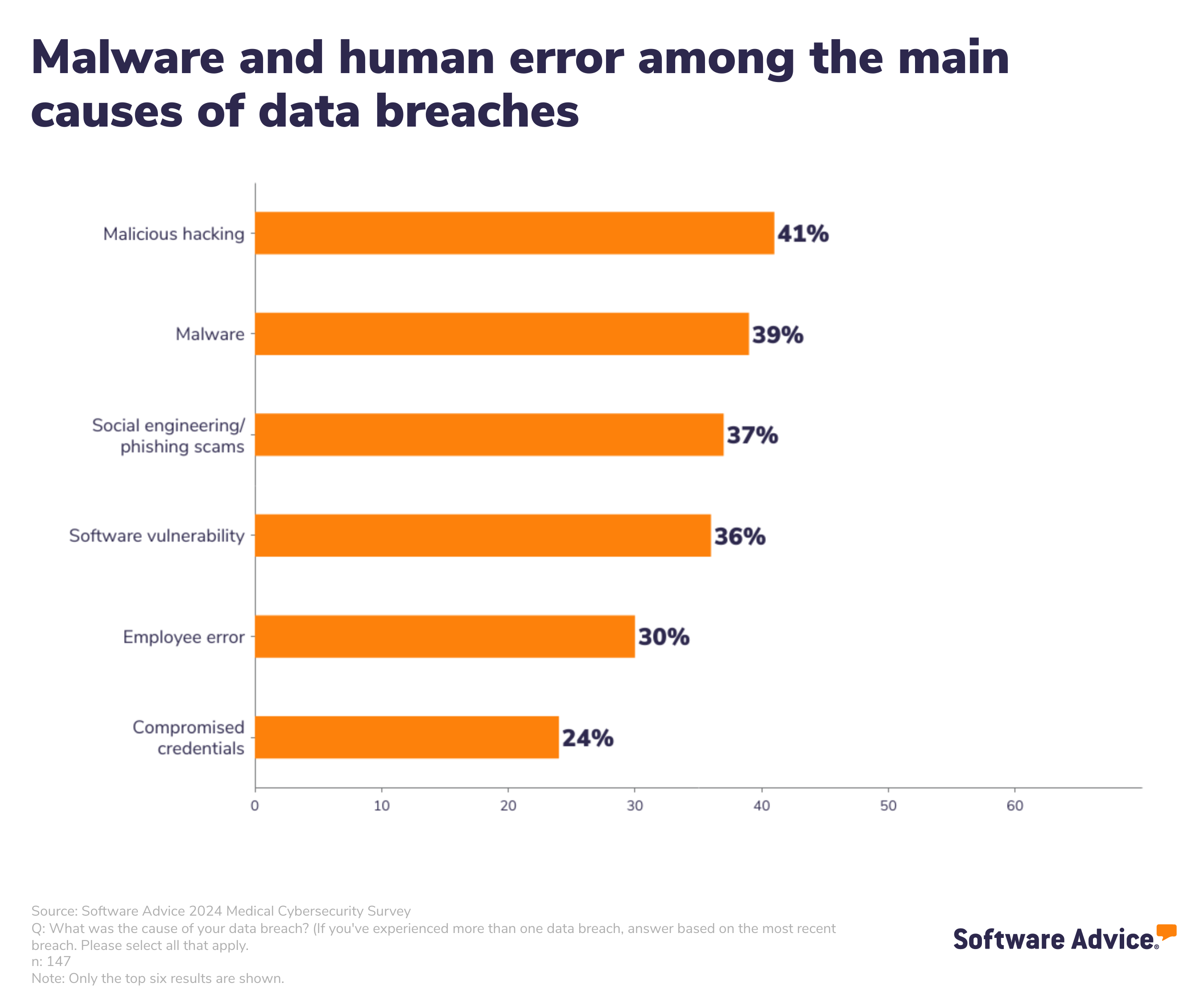
At least one-half of U.S. health care organizations have experienced a data breach, one-third in the last 3 years, according to Software Advice’s 2024 Healthcare Data Security Survey released in May 2024. Of the health care organizations who experienced ransomware attacks, one-third did not recover patient data from the cyber-attackers, Software Advice learned. Clearly, cyberattacks are impacting patient care. And the growth of home care, hospital-to-home, and greater self-care are also increasing risks for cybersecurity. The growing adoption of digital technologies in healthcare, from the hospital to the doctor’s office to the home,
Medical Debt, Aflac on Eroding Health Benefits, the CBO’s Uninsured Forecast & Who Pays for Rising Health Care Prices: A Health Consumer Financial Update
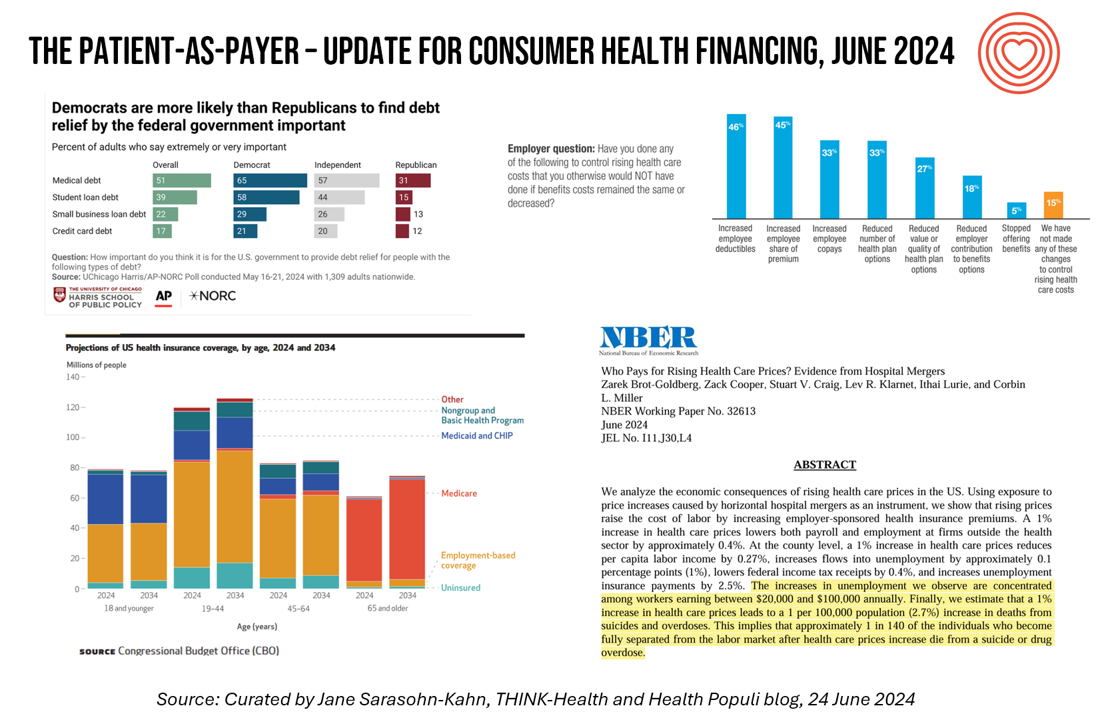
On June 11, Rohit Chopra, the Director of the Consumer Financial Protection Bureau (CFPB) announced the agency’s vision to ban Americans’ medical debt from credit reports. He called out that, “In recent years, however, medical bills became the most common collection item on credit reports. Research from the Consumer Financial Protection Bureau in 2022 showed that medical collections tradelines appeared on 43 million credit reports, and that 58 percent of bills that were in collections and on people’s credit records were medical bills.” Chopra further explained that medical debt on a consumer credit report was quite different than other kinds
How to Get Better Care to More People? Address Burnout, Bridge Insights with AI, Embed Sustainability – the Philips Future Health Index 2024

Health care access is a challenge in rural and urban areas, cities and suburbs, and across more demographic groups than you might realize, as we see wait times grow for appointments, primary care shortages, and delays in screening plaguing health systems around the world. In the Future Health Index 2024, Philips’ latest annual report presents a profile of the state of health care focused on how to provide better care for more people. For the report, Philips surveyed a total of 2,800 healthcare leaders consisting of 200 respondents in 14 countries: Australia, Brazil, China,
A 2025 Subaru Forester, a Year at U-New Mexico, or a Health Plan for a Family of Four: the 2024 Milliman Medical Index
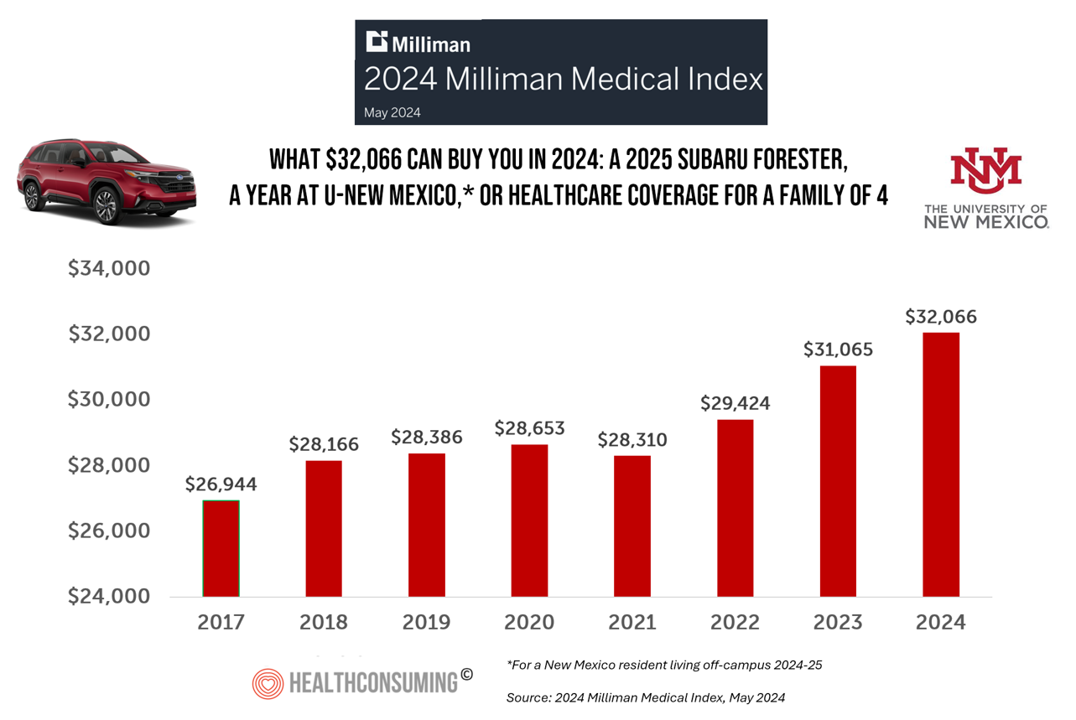
Health care costs for an “average” person covered by an employer-sponsored PPO in the U.S. rose 6.7% between 2023 and 2024, according to the 2024 Milliman Medical Index. Milliman also calculated that the largest driver of cost increase in health care, accounting for nearly one-half of medical cost increases, was pharmacy, the cost of prescription drugs, which grew 13% in the year. The big number this year is $32,066, which is the cost of that employer-sponsored PPO for a family of 4 in 2024. I’ve curated the chart of the MMI statistic for many
Is There an Easy-Button for AI In Healthcare Team Well-Being? Exploring a New PC with Embedded AI

“The greatest opportunity offered by AI is not reducing errors or workloads, or even curing cancer: it is the opportunity to restore the precious and time-honored connection and trust,” Dr. Eric Topol wrote in his 2019 book, Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again. In the five years since Dr. Topol looked for AI to bolster the human-touch in health care, we’ve lived, worked, and muddled our way through the COVID-19 pandemic and witnessed the growing epidemic of burnout among clinicians, the front-line of medical care. I recalled Dr. Topol’s assertion on AI’s promise for humanizing health
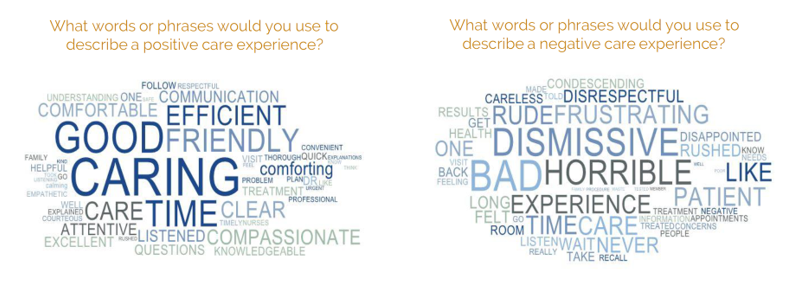
The ROI on Patient Experience = Loyalty, Trust and Revenue – Listening to Accenture
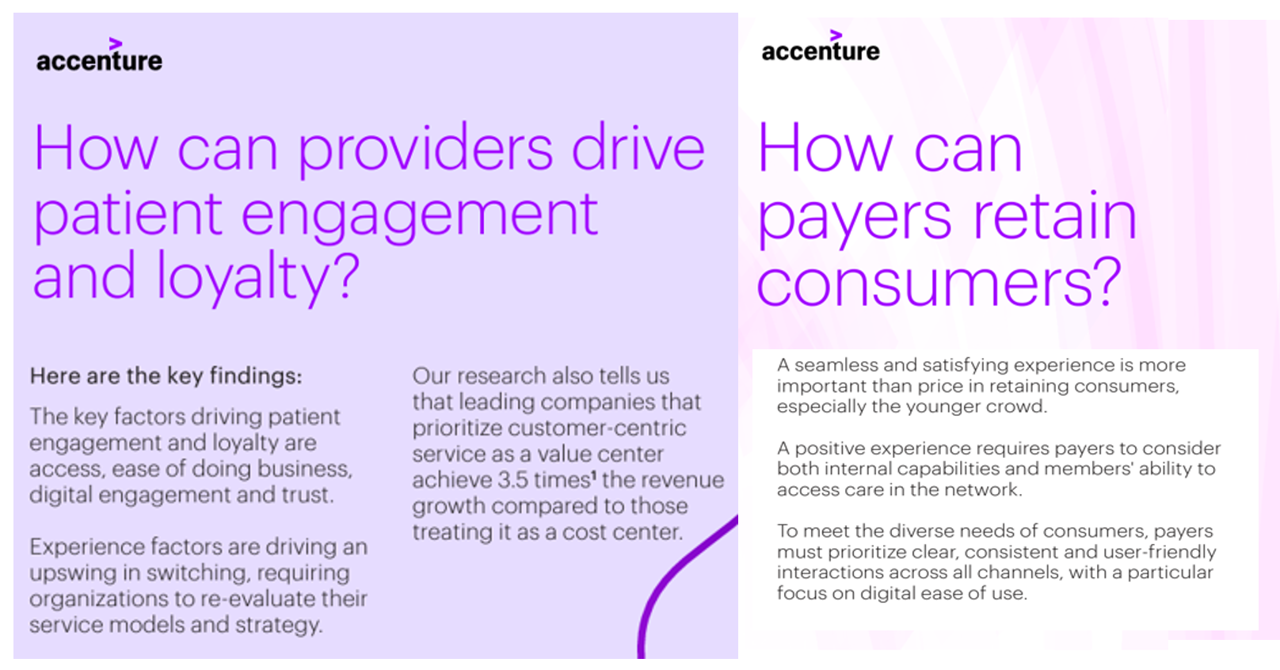
When health care providers and payers make patients’ lives easier, there’s a multiplying factor for loyalty and revenue growth, according to Accenture’s latest look into the value of experience in The Power of Trust: Unlocking patient loyalty in healthcare. Accenture conducted two surveys for this research, assessing nearly 16,000 U.S. adult consumers’ views on healthcare providers and health insurance plans. Several factors underpin patients’ selection of a new health care provider, especially: Access (70%), with a convenient location, quickly available appointments, digital/mobile/social interactions, and virtual care availability; and, The provider being a trusted source
Inflation, Health, and the American Consumer – “The Devil Wears Kirkland”
The Wall Street Journal reported yesterday that surging hospital prices are helping to keep inflation high. Hospital costs rose 7.7% last month, the highest increase in 13 years. This chart from WSJ’s reporting illustrates the >2x change in the CPI for hospitals vs the overall rate of price increases. Hospitals are not alone in price cliffs, with health insurance premiums spiking last year at the fastest rate in a decade, the Labor Statistics data showed. “For patients and their employers, the increases have meant higher health-insurance premiums, as well as limiting wage
Hospital at Home: Prospects and Challenges, and Learnings from Best Buy Health
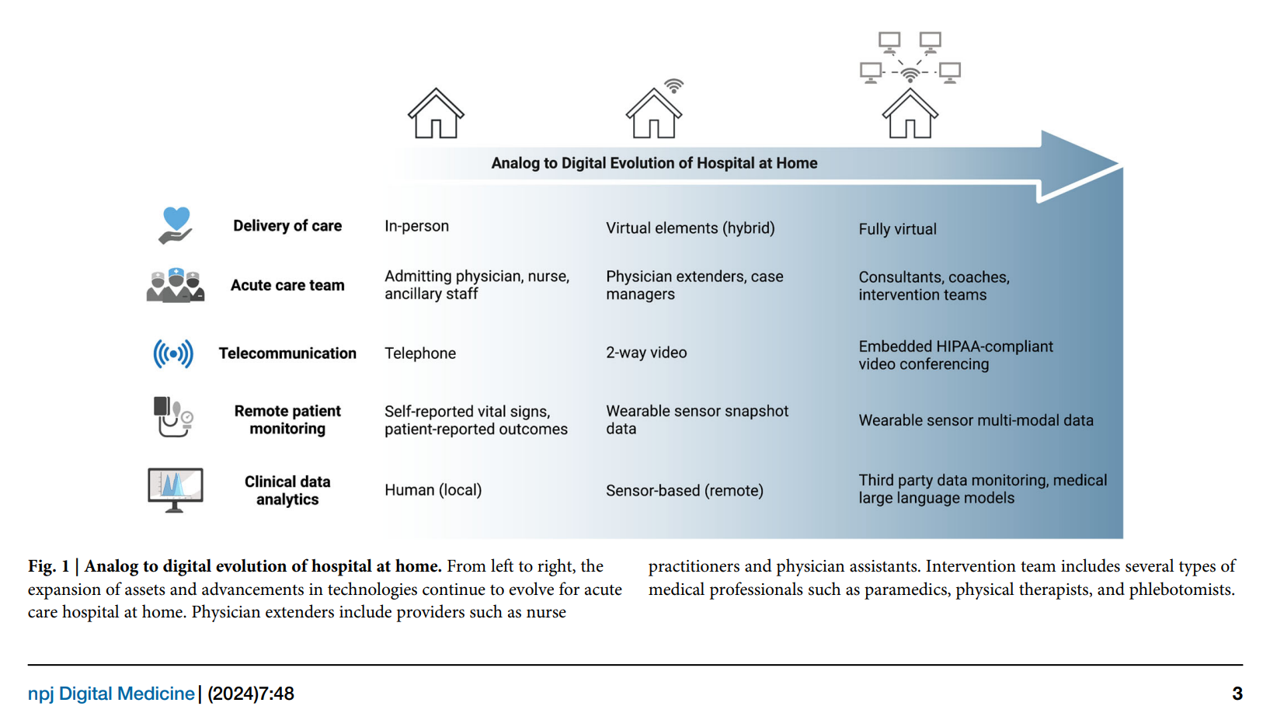
With the urgent need to identify more efficient and lower-cost health care delivery models, we look to growing evidence for digital health technologies that support the Hospital at Home (HaH) model, considered in a new review article published in late February in npj Digital Medicine, The hospital at home in the USA: current status and future prospects. Clinicians from Scripps Research and Johns Hopkins School of Medicine collaborated on this work, calling out the relatively fast adoption of HaH programs during the peak of the COVID-19 pandemic. In some parts of the world, such as Australia and Norway, “in-person at-home
A Health Consumer Bill of Rights: Assuring Affordability, Access, Autonomy, and Equity
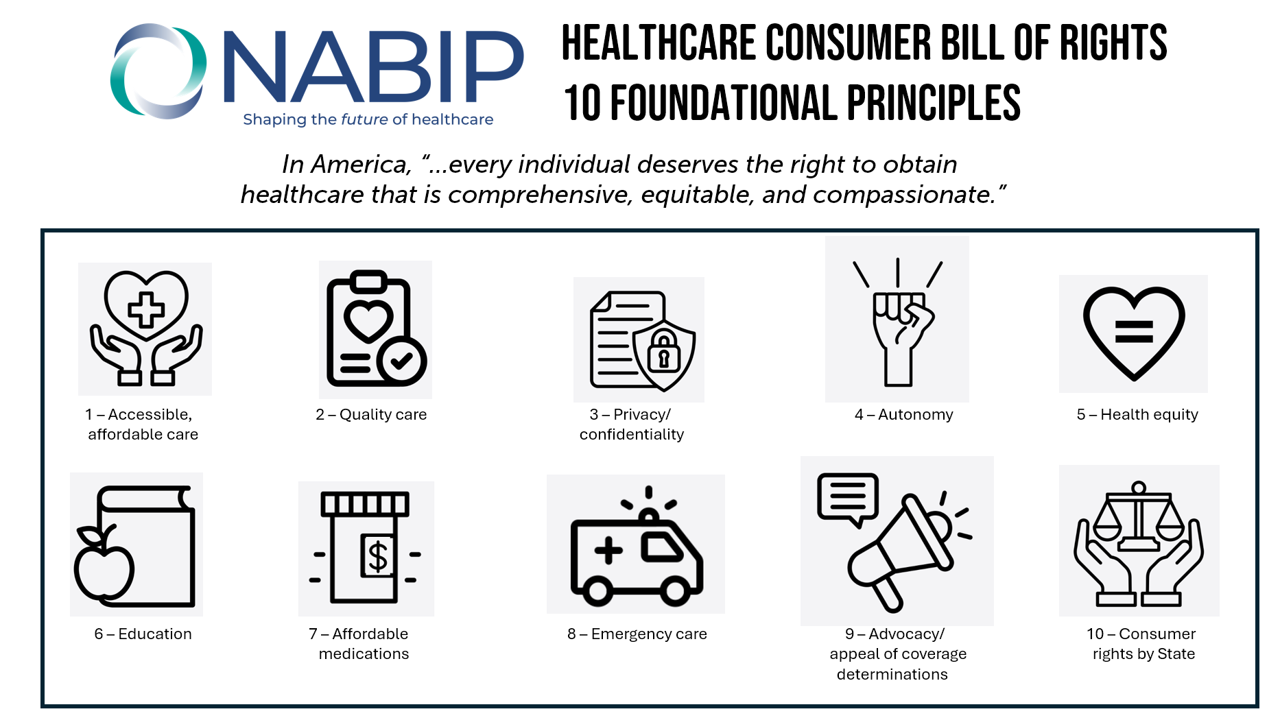
Let’s put “health” back into the U.S. health care system. That’s the mantra coming out of this week’s annual Capitol Conference convened by the National Association of Benefits and Insurance Professionals (NABIP). (FYI you might know of NABIP by its former acronym, NAHU, the National Association of Health Underwriters). NABIP, whose members represent professionals in the health insurance benefits industry, drafted and adopted a new American Healthcare Consumer Bill of Rights launched at the meeting. While the digital health stakeholder community is convening this week at VIVE in Los Angeles to share innovations in health tech, NABIP
People With Medical Debt Are Much More Likely to Be in Financial Distress in America
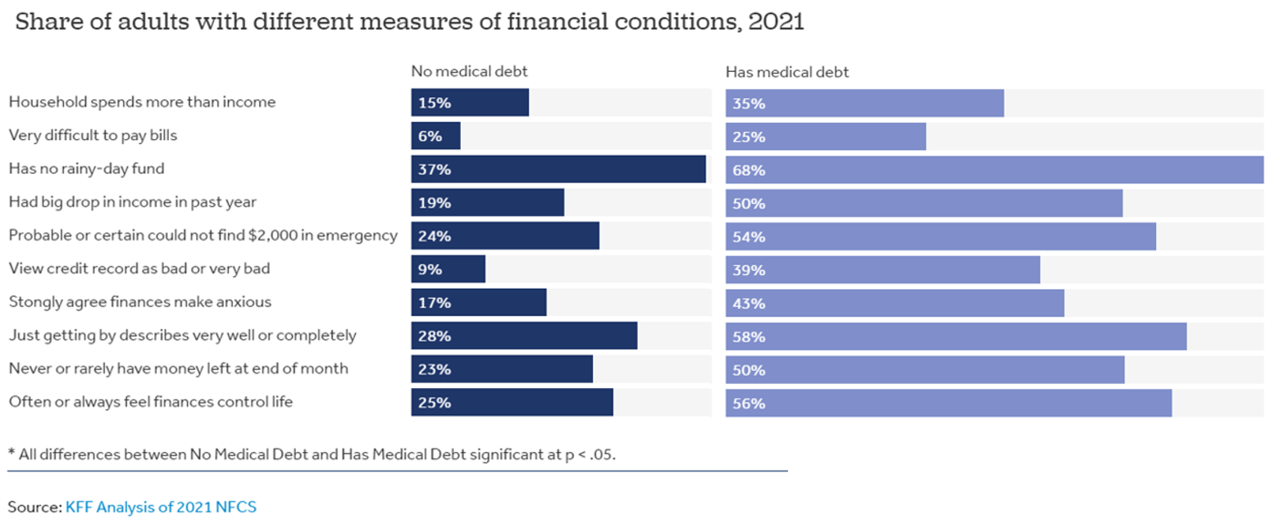
How financially vulnerable are people with medical debt in the U.S.? Significantly more, statistically speaking, we learn from the latest survey data revealed by the National Financial Capabilities Study (NFCS) from the FINRA Foundation. The Kaiser Family Foundation and Peterson Center on Healthcare analyzed the NFCS data through a consumer health care financial lens with a focus on medical debt. Financial distress takes many forms, the first chart inventories. People with medical debt were most likely lack saving for a “rainy day” fund, feel they’re “just getting by” financially, feel their finances control their life, and
From Evolution to Innovation, from Health Care to Health: How Health Plans With Collaborators Are Re-Defining the Industry
As a constant observer and advisor across the health/care ecosystem, for me the concept of a “health plan” in the U.S. is getting fuzzier by the day. Furthermore, health plan members now see themselves as medical bill payers, seeking value and consumer-level services for their health insurance premium investment. Weaving these ideas together is my mission in preparing a session to deliver at the upcoming AHIP 2024 conference in June, I’m thinking a lot about the evolving nature of health insurance, plans, and the organizations that provide them. To help me define first principles, I turned to the American father
What If We Built a Consumer-Enchanting Health System in the Context of HLTH 2023? Building Blocks for the Scenario

What if….you were given the opportunity to build a health system from scratch in this new era of platforms, cloud computing, AI and machine learning, curious-digital-empowered consumers, and collaborators in retail and community settings operating close to peoples’ homes and workplaces? With the HLTH 2023 Conference meeting up in Vegas these past couple of days, this “what if” scenario can be constructed with announcements coming out of the meeting, coupled with recent developments in the larger health/care ecosystem. Start with General Catalyst’s news of engaging Dr. Marc Harrison, most recently CEO of Intermountain Health,
The Omnichannel Imperative for Healthcare: Supporting Telehealth Awareness Week 2023
“What omnichannel really means: hearing the customer wherever they are and making them feel heard, valued, and understood.” That statement comes from Qualtrics’ explanation of omnichannel experience design. The very human needs of feeling one is heard, is valued, and is understood, underpin the rasion d’etre of omnichannel marketing. And these very values are those that underpin the trust between patients and providers and the large healthcare ecosystem. It’s Telehealth Awareness Week, led by the ATA. I celebrate and support the effort; this Health Populi post explains the Association’s mantra that Telehealth is Health, and that
Slip Slidin’ Away: the Reputations of Pharma and Healthcare in the U.S. Decline in the Latest Gallup Poll
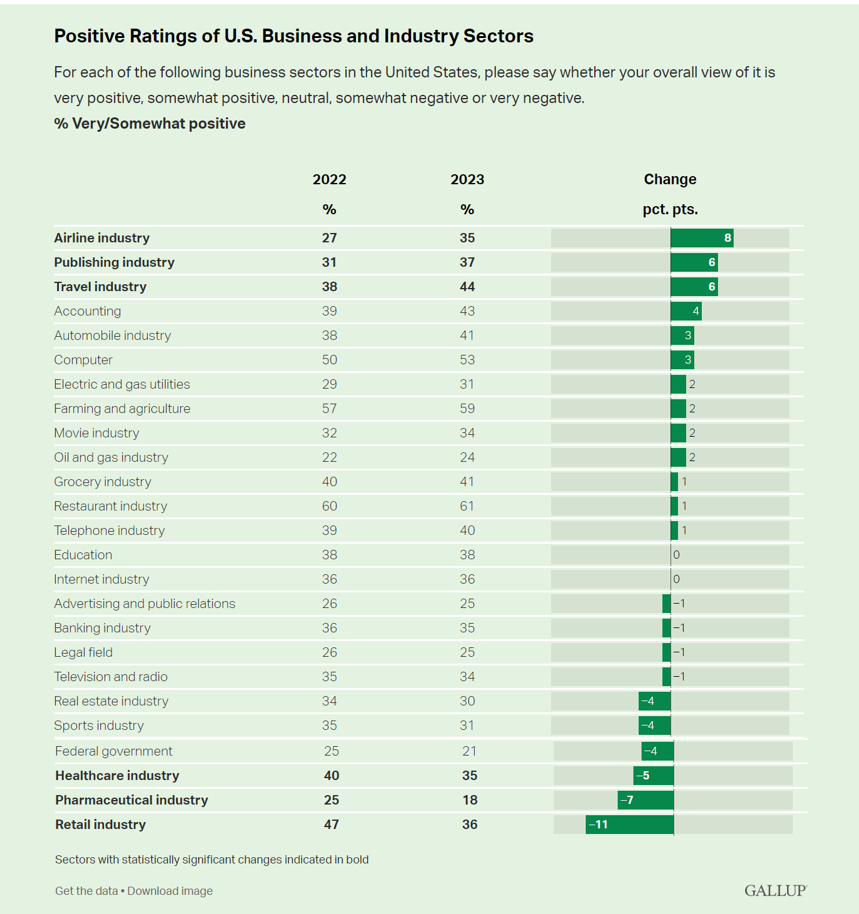
Oh, how quickly people forget…and slow to forgive. U.S. consumers’ positive views for healthcare, pharma and retail have significantly fallen in just one year, the latest annual Gallup poll of industry rankings in America found as of August 2023. This stat for the pharma industry was the lowest Gallup ever recorded for the sector since 2001. I can’t help hearing Paul Simon’s lyrics to Slip Slidin’ Away….”you know the nearer your destination, the more you’re slip slidin’ away” when it comes to health citizens’ perceptions of pharma and the healthcare
Location, Location, Location – Understanding Health Consumers’ Evolving Definition of Convenience
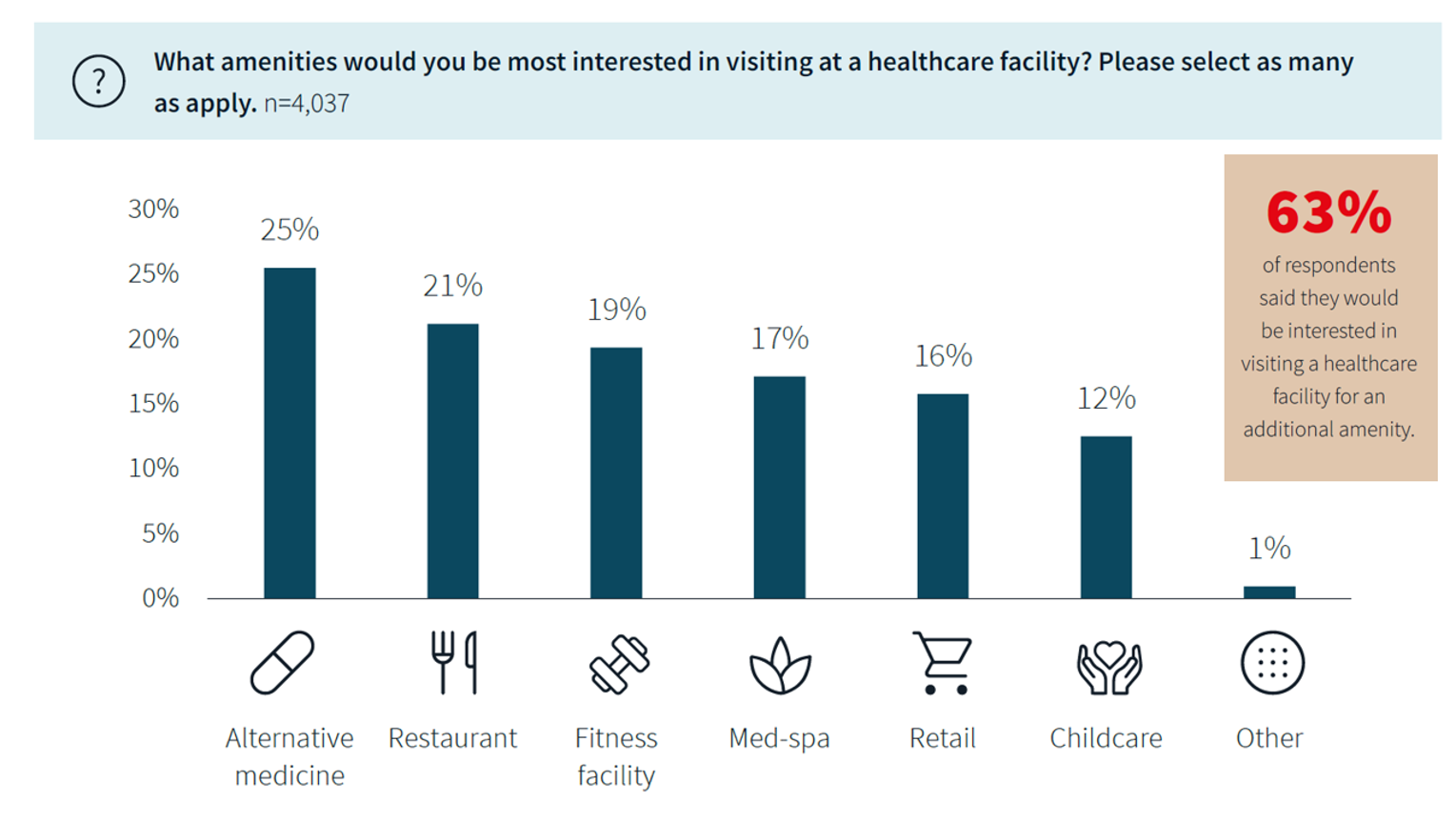
The definition of “convenience” in the eyes of patients, consumers, and caregivers is multi-faceted, with the concept of “location” shifting both physically and digitally. We learn this in new research from JLL, the global real estate services company. “Why is a real estate services company doing research into consumers’ views on health care?” you might ask. See my Hot Points below, discussing my views on the morphing of health care real estate from Pill Hill and inpatient hospitals to the home and closer-to-home sites. In the 2023 Patient Consumer Survey report, the topline lesson
Happy 75th Birthday, NHS – Through A U.S. Health Care Lens
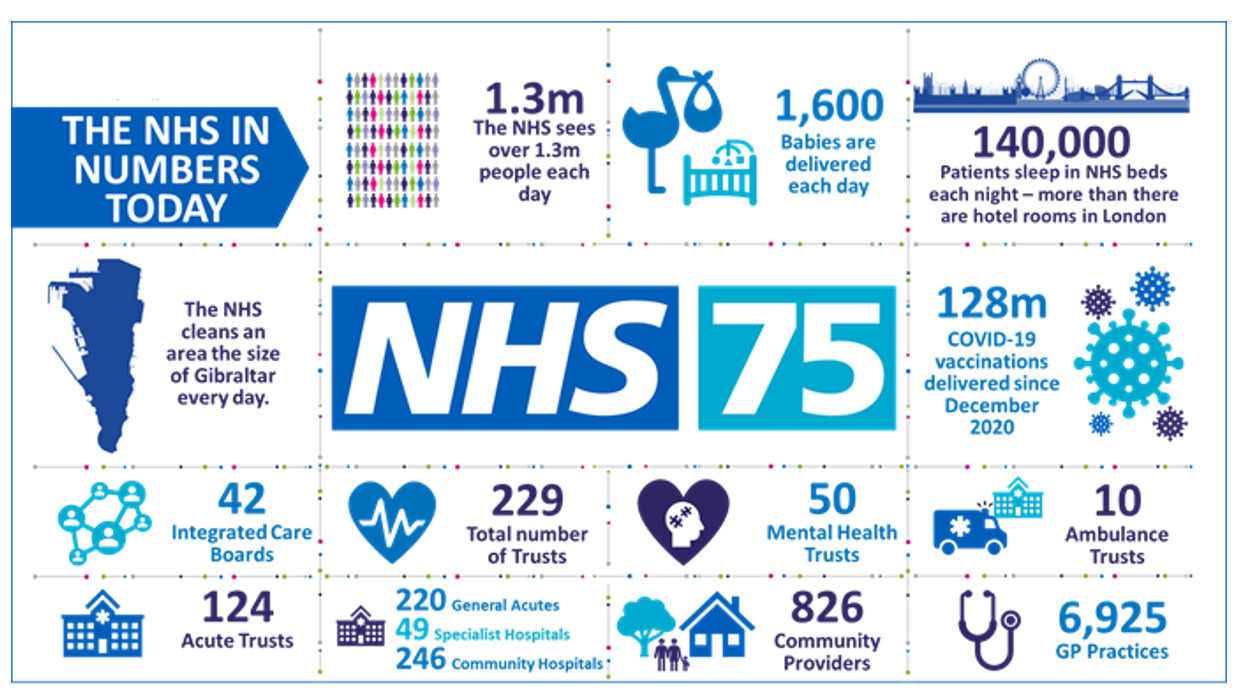
The UK’s National Health Service (NHS) turns 75 today. The NHS was the brainchild of Minister of Health Aneurin Bevan; he wrote in a statement to doctors and nurses in The Lancet on July 3, 1948, “My job is to give you all the facilities, resources, apparatus and help I can, and then to leave you alone as professional men and women to use your skill and judgement without hindrance.” This week in The Lancet, the editors assert, “The founding principles of the NHS put into practice 75 years ago are at risk of
Retail Clinics’ Growing Role in Health Care and Prescription Drug Sales
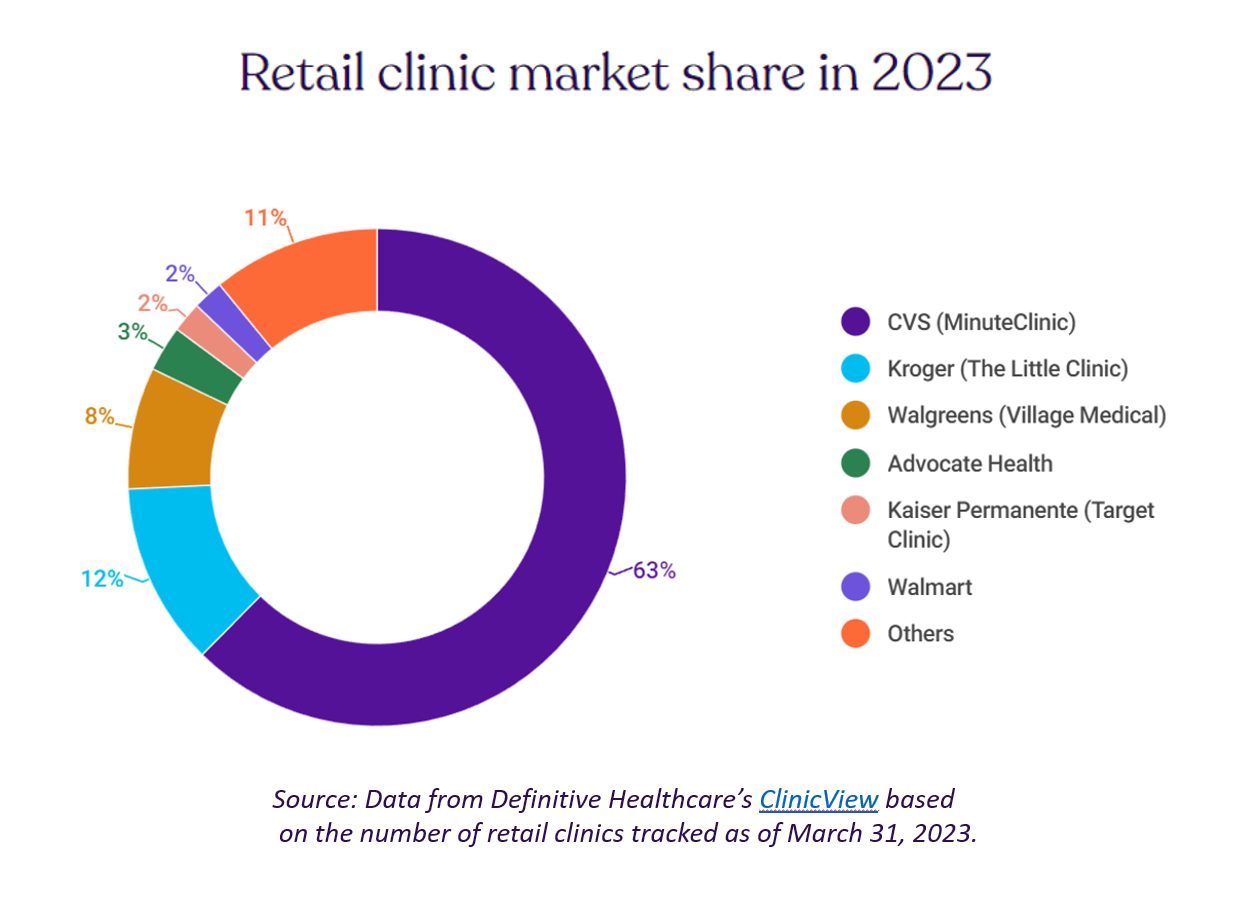
“It seemed like an odd pairing: shampoo and a throat swab,” observes a new report on the growth of retail health from Definitive Healthcare. But retail clinics are no longer, as the paper explains, “an experiment of a few grocery stores….they’re becoming a major force in the U.S. healthcare system,” asserts the thesis of Retailers in healthcare: A catalyst for provider evolution. While the use of emergency departments fell by 1% in the past five years, the use of retail clinics expanded by 70%, Definitive Healthcare calculated. Most retail clinics are owned by
Virtual Health Care Can Reduce Carbon Emissions: the Environmental ROI on Telehealth
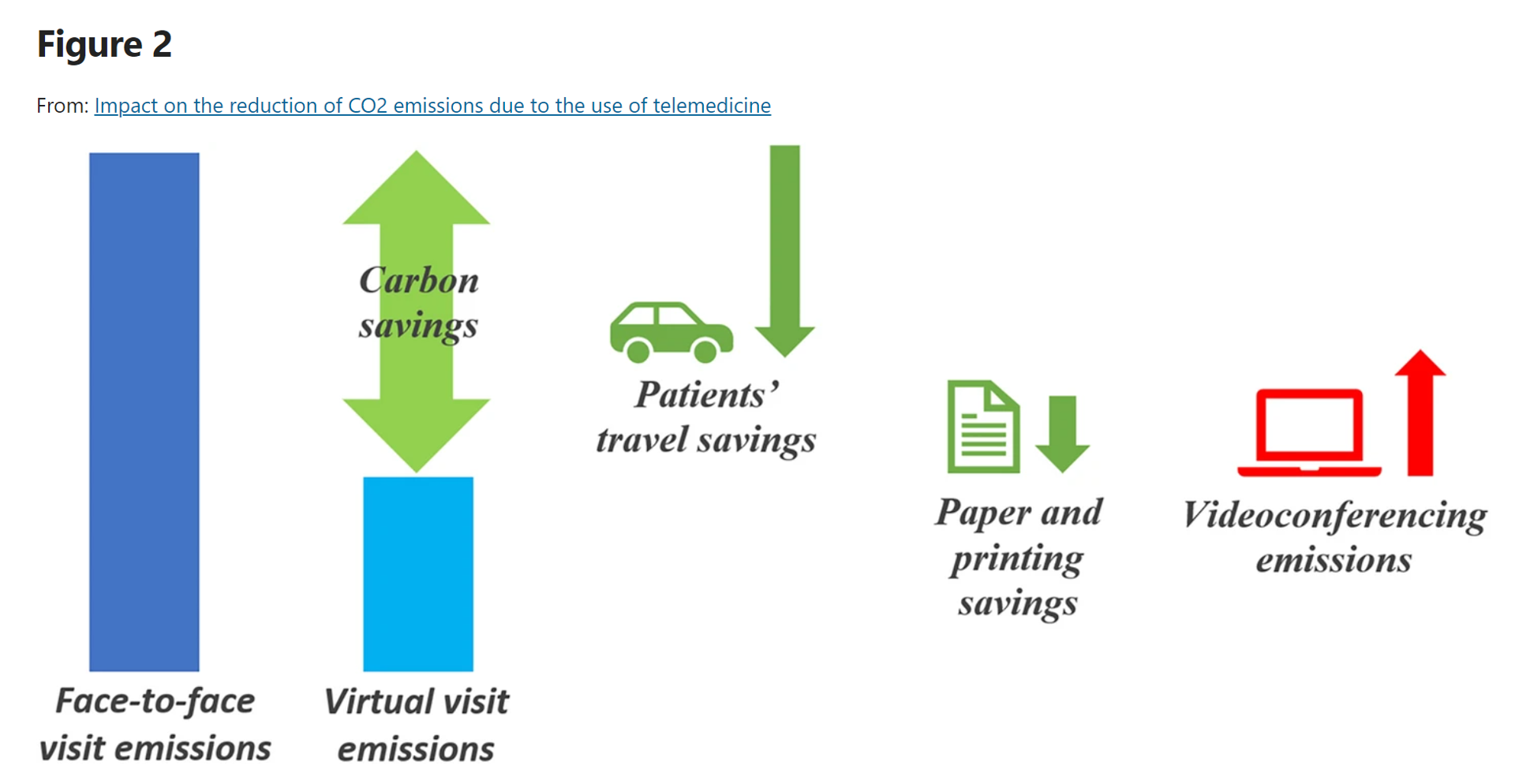
As implemented in the COVID-19 era and its immediate wake, the most obvious environmental benefits offered by telehealth visits replacing in-person patient encounters have been achieved through reduced patient travel, considering The Role of Virtual Consulting in Developing Environmentally Sustainable Health Care, a systematic literature review published in the Journal of Medical Internet Research. This study, led by researchers at the University of Oxford, UK, and the University of Oslo, Norway, identified over 1,600 scientific papers, narrowing the most rigorous and relevant to 23 papers focusing on virtual consulting and carbon emissions. This is an important question for two major
“Your care, your way:” Learning from the Philips Future Health Index 2023
Consider the key drivers of supply and demand in health care, globally, right now: On the medical delivery supply side, the shortage of staff is a limiting factor to continuing to deliver care based on the usual work-flows and payment models. On the demand side, patients are taking on more demanding roles as consumers with high expectations for service, convenience, and safe care delivered closer to home — or at home. This dynamic informs The Future Health Index 2023 report from Philips, launched this week at HIMSS 2023. This is the eighth annual global FHI report, with detailed country-specific analyses to
The Top 10 Patient Safety Concerns for 2023 Are About Social, Mental and Behavioral Health
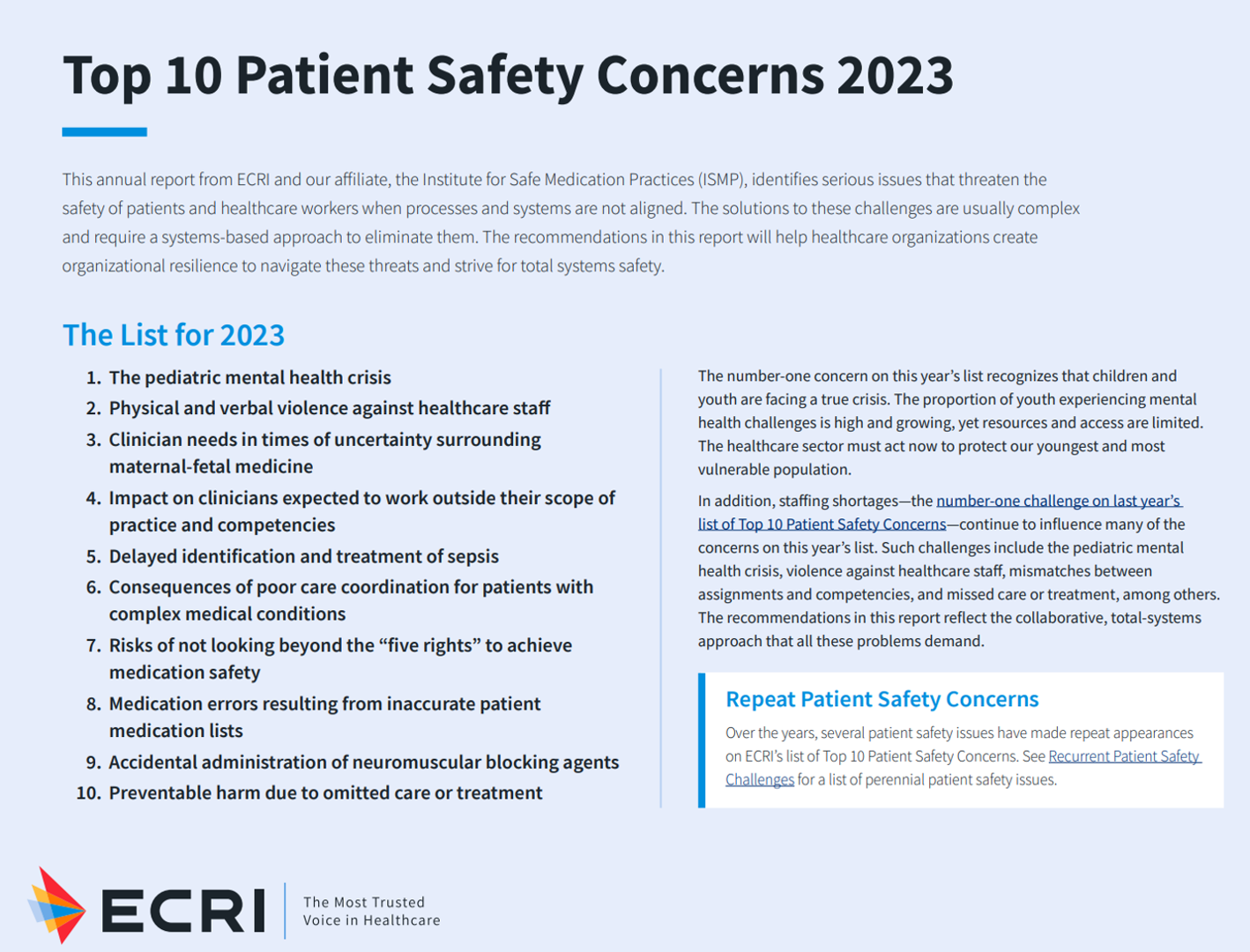
Ten years ago, ECRI named the top 10 health technology hazards for 2013: they were alarm hazards, medication administrative errors using infusion pumps, unnecessary exposure and radiation burns from diagnostic radiology procedures, patient/data mismatches in EHRs and other HIT systems, interoperability failures with medical devices and health IT systems, and five other tech-related hazards. In 2014, ECRI pivoted the title of this annual report to “patient safety concerns,” a nuance away from health technology. Fast forward to 2023 and ECRI’s latest take on the Top 10 Patient Safety Concerns 2023. While technology is embedded in this list, the headlines have more
Quick, Accessible, Inexpensive Health Care – A Retail Health Update from Amazon and Dollar General

Two announcements this week add important initiatives to patients’ growing choices that speak to their consumer-sides’ sense of value and personal healthcare cost-containment: Amazon launched RxPass, a generic medicines subscription service; and, Dollar General promoted its mobile health service powered by DocGo on demand for health visits, “right outside the store.” These two programs come from outside of the legacy health care system of so-called incumbents — hospitals, health systems, health insurance — leveraging two brand-names beloved to many consumers for convenience, price transparency, and sheer cost. First, check out Amazon Pharmacy’s RxPass. Amazon
When Household Economics Blur with Health, Technology and Trust – Health Populi’s 2023 TrendCast

People are sick of being sick, the New York Times tells us. “Which virus is it?” the title of the article updating the winter 2022-23 sick-season asked. Entering 2023, U.S. health citizens face physical, financial, and mental health challenges of a syndemic, inflation, and stress – all of which will shape peoples’ demand side for health care and digital technology, and a supply side of providers challenged by tech-enabled organizations with design and data chops. Start with pandemic ennui The universal state of well-being among us mere humans is pandemic ennui: call it languishing (as opposed to flourishing), burnout, or
Site-Shifting: the Consumer-Driven Pressure on Traditional Healthcare Utilization
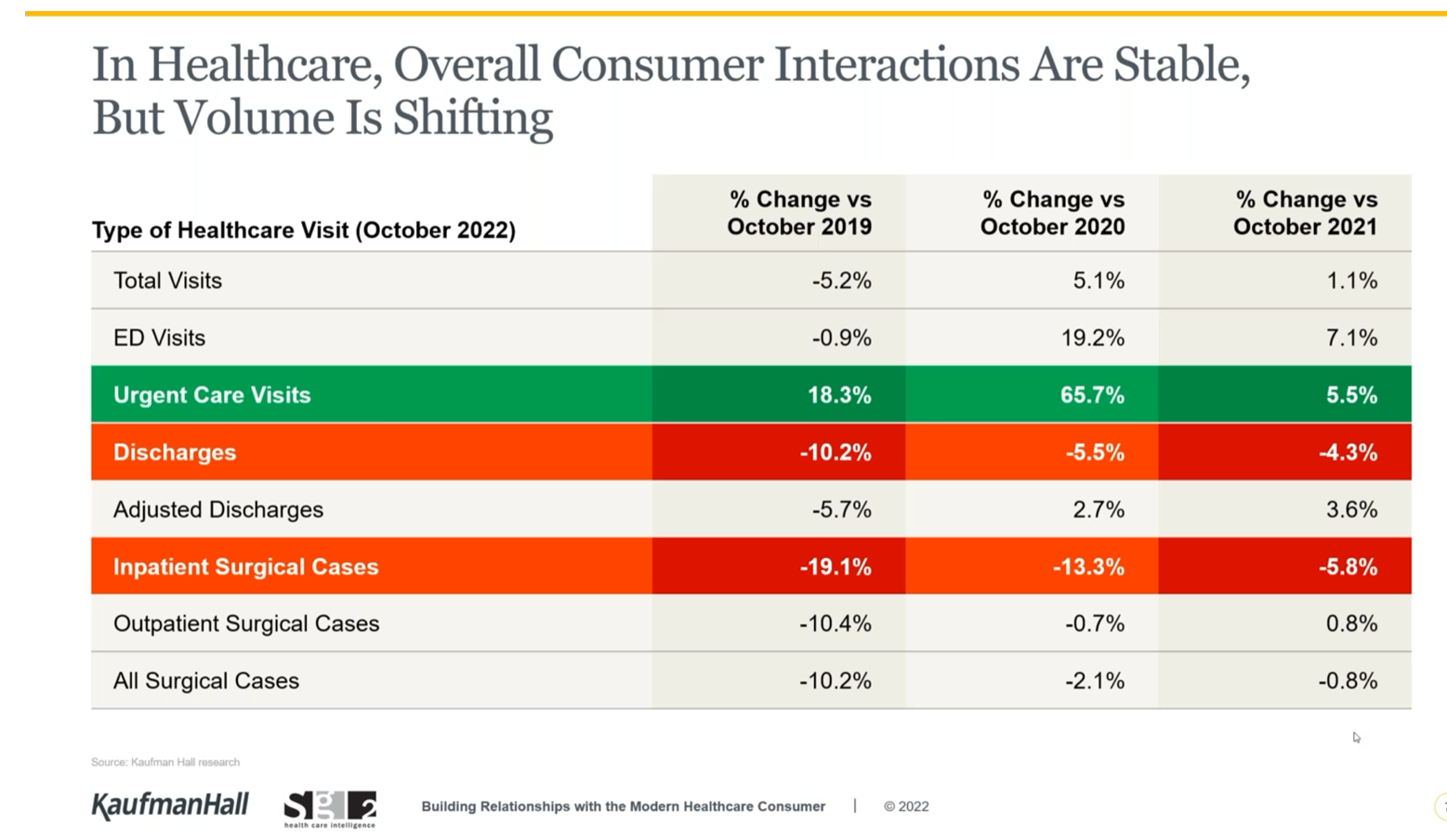
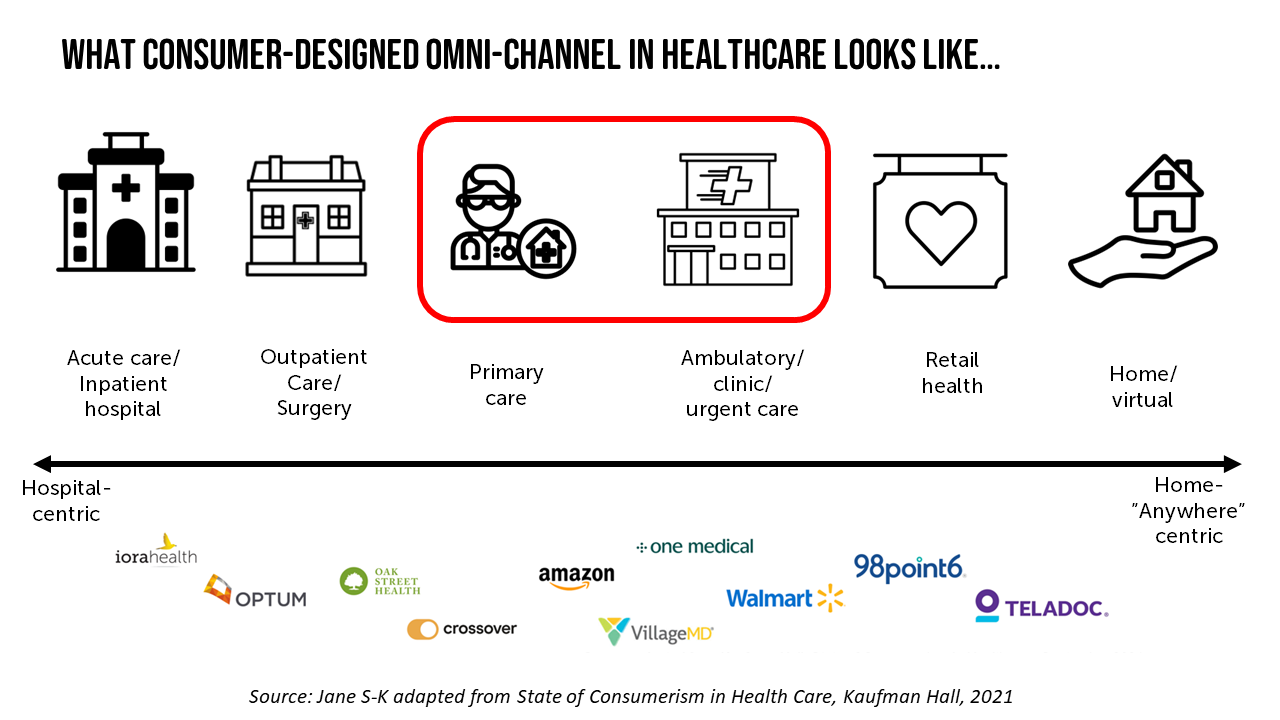
While overall U.S. consumers’ utilization of health care has been pretty stable, the type of visit encounters is shifting away from hospital inpatient cases to ambulatory care, urgent and retail health care sites, data from Kaufman Hall and Sg2 tell us. The companies shared insights in a session on Building Relationships with the Modern Healthcare Consumer last week, warning that hospitals are facing economic challenges with implications on how they should engage and interact with patients in the coming months and years. Wearing a consumer-centric lens, Dan Clarin of Kaufman Hall and Charlotte Brown-Zalewa
Irrational Exuberance for Hospital-To-Home? Care About the Caregivers, the House, the Fridge.
Home, Sweet Hospital-At-Home? It depends, I hedge in my latest essay for Medecision. In our bullish and, on its face, compassionate and cost-rational embrace of the migration of acute care from hospital beds to peoples’ living and bedrooms, there are several guardrails to consider beyond sheer payment and reimbursement calculations. Consider, The caregivers for the folks heading home from hospital The state of the physical home — for safety, comfort, environmental health, and emotional security, and, Food security and nutritional access. On caregiving: I spend extra time detailing research in which Alexandra Drane, founder of
Home Is Where the Health Is: An Update on Connectivity, Food, and Retail
Virtually every closed-door meeting I have had in the U.S. with a client group in the past several months has had a line item on the agenda to brainstorm the impact and opportunity of care-at-home, hospital-to-home, or Care Everywhere. This has happened across many stakeholders in the evolving health/care ecosystem of suppliers, including hospital systems, health plans, grocery chains, retail pharmacy, consumer technology, digital health and tech-enabled providers, pharma and medical supply companies. On October 10, Dr. Robert Pearl, former CEO of The Permanente Medical Group, published a provocative post on Forbes noting that Amazon, CVS, Walmart Are Playing Healthcare’s
The Direct Link Between Value-Based Health Care, Digital Transformation and Social Determinants – Insights from Innovaccer and Morning Consult
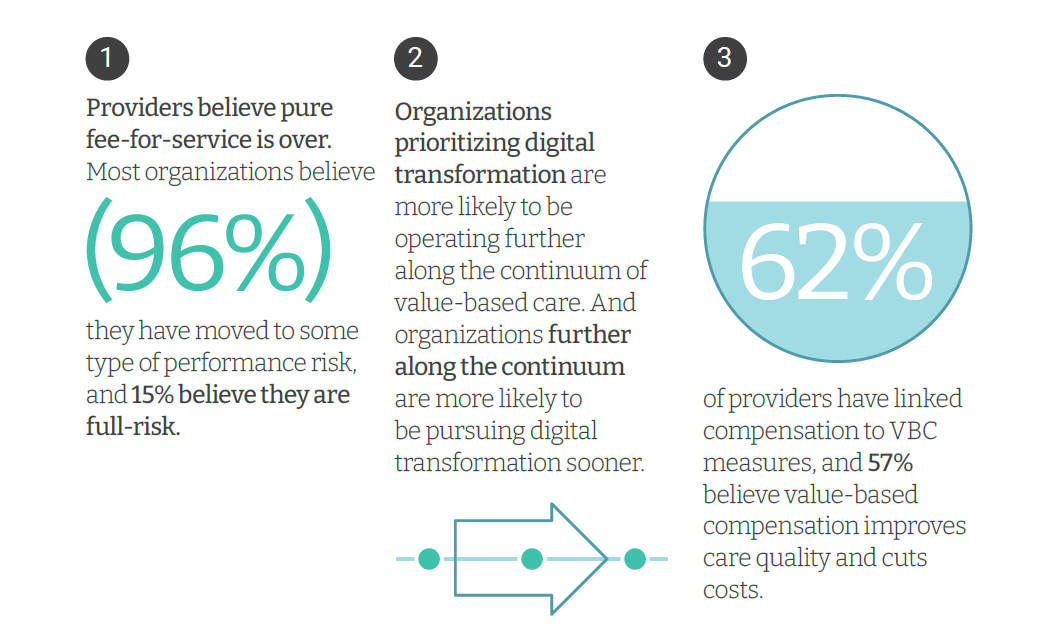
Only 4% of health care payments in the U.S. are pure fee-for-service (FFS) these days. “The end of pure FFS is near,” according to The State and Science of Value-Based Care, a report-out of survey research from Innovaccer and Morning Consult. Innovaccer, a health cloud/data analytics company, worked with Morning Consult to do deep-dive interviews with 75 senior health care executives; research was conducted in November and December 2021, so these perspectives represent those of health system leaders at the start of 2022. The full report is worth your read; my focus in this Health
The Patient As the Payer: Self-Pay, Bad Debt, and the Erosion of Hospital Finances
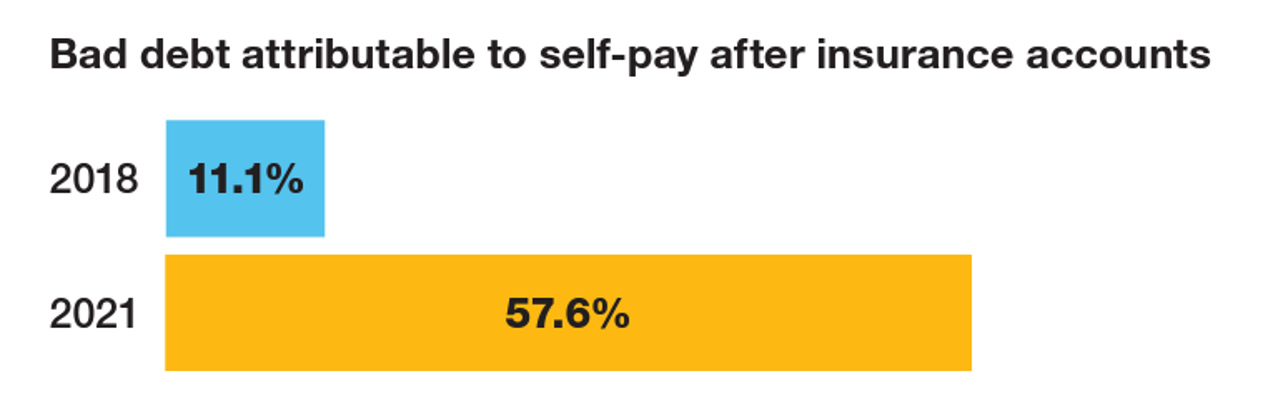
“The odds are against hospitals collecting patient balances greater than $7,500,” the report analyzing Hospital collection rates for self-pay patient accounts from Crowe concludes. Crowe benchmarked data from 1,600 hospitals and over 100,00 physicians in the U.S. to reveal trends on health care providers’ ability to collect patient service revenue. And bad debt — write-offs that come out of uncollected patient bill balances after “significant collection efforts” by hospitals and doctors — is challenging their already-thin or negative financial margins. The first chart quantifies that bad debt attributable to patients’ self-pay payments
Partnering Up in the Health Care Ecosystem to Drive Transformation – for Organizations and Health Consumers Alike
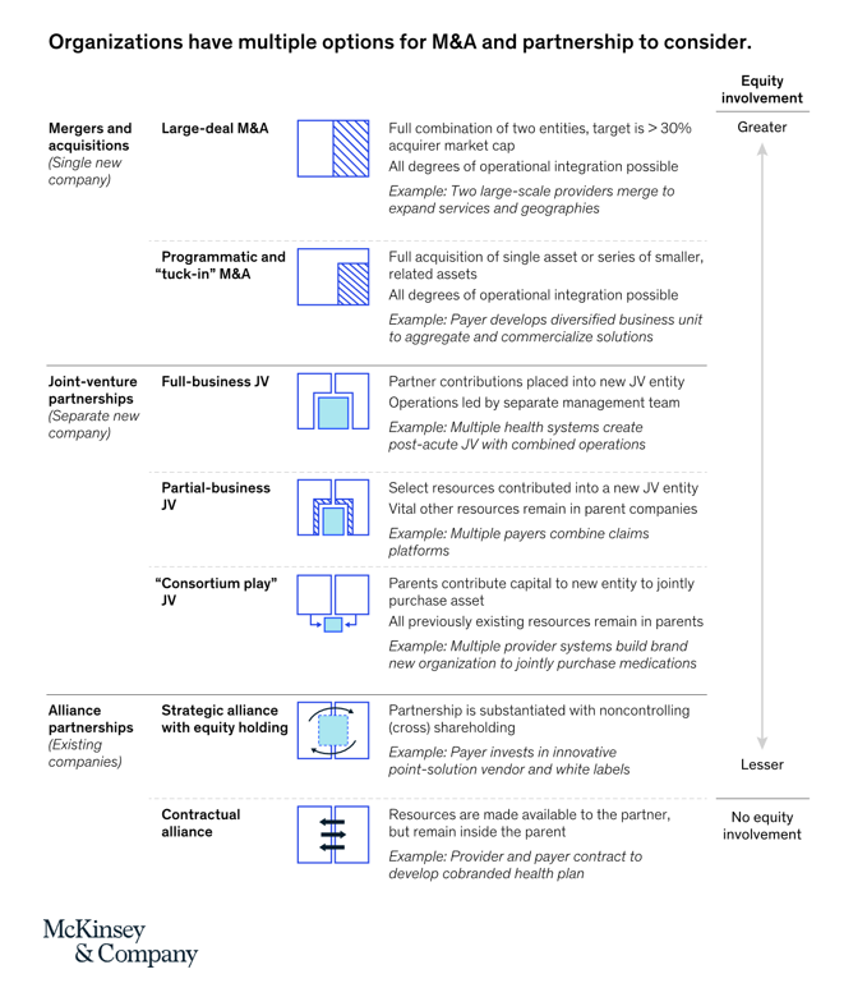
“Partnerships, including JVs and alliances with other healthcare organizations and with new entrants, are just one way to access new capabilities, unlock speed to market, and achieve capital, scale, and operational efficiencies” in health care transformations. “In an environment with continued competition for attractive assets and significant capital in play from institutional investors, these partnerships may also be the most accessible way for organizations to capture value in expanding healthcare services and technology value pools,” we learn in Overcoming the cost of healthcare transformation through partnerships from a team of health care folks with McKinsey & Company.
Healthcare access, racial disparities, guns and climate – U.S. doctors are worried about some big social issues
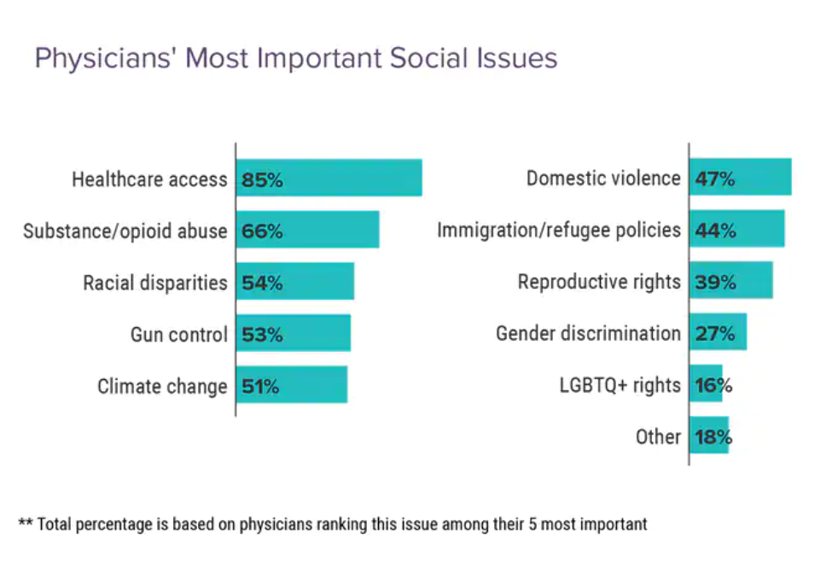
Doctors heads and hearts are jammed with concerns beyond curing patients’ medical conditions: U.S. physicians are worried about big social issues, according to a Medscape survey report, Physicians’ Views on Today’s Divisive Social Issues 2022. Topping physicians’ list of their top-five most important social issues, far above all others ranked healthcare access. Underneath that top-line statistic, it’s important to note that: 52% of doctors are “very concerned” about healthcare access, 28% are “concerned,” and 13% are “somewhat concerned.” Medscape underscores that in 2020, 31 million U.S. residents had no health insurance coverage, and
A New Chevy Equinox SUV, a Year in Grad School, or Health Care for Four – The 2022 Milliman Medical Index
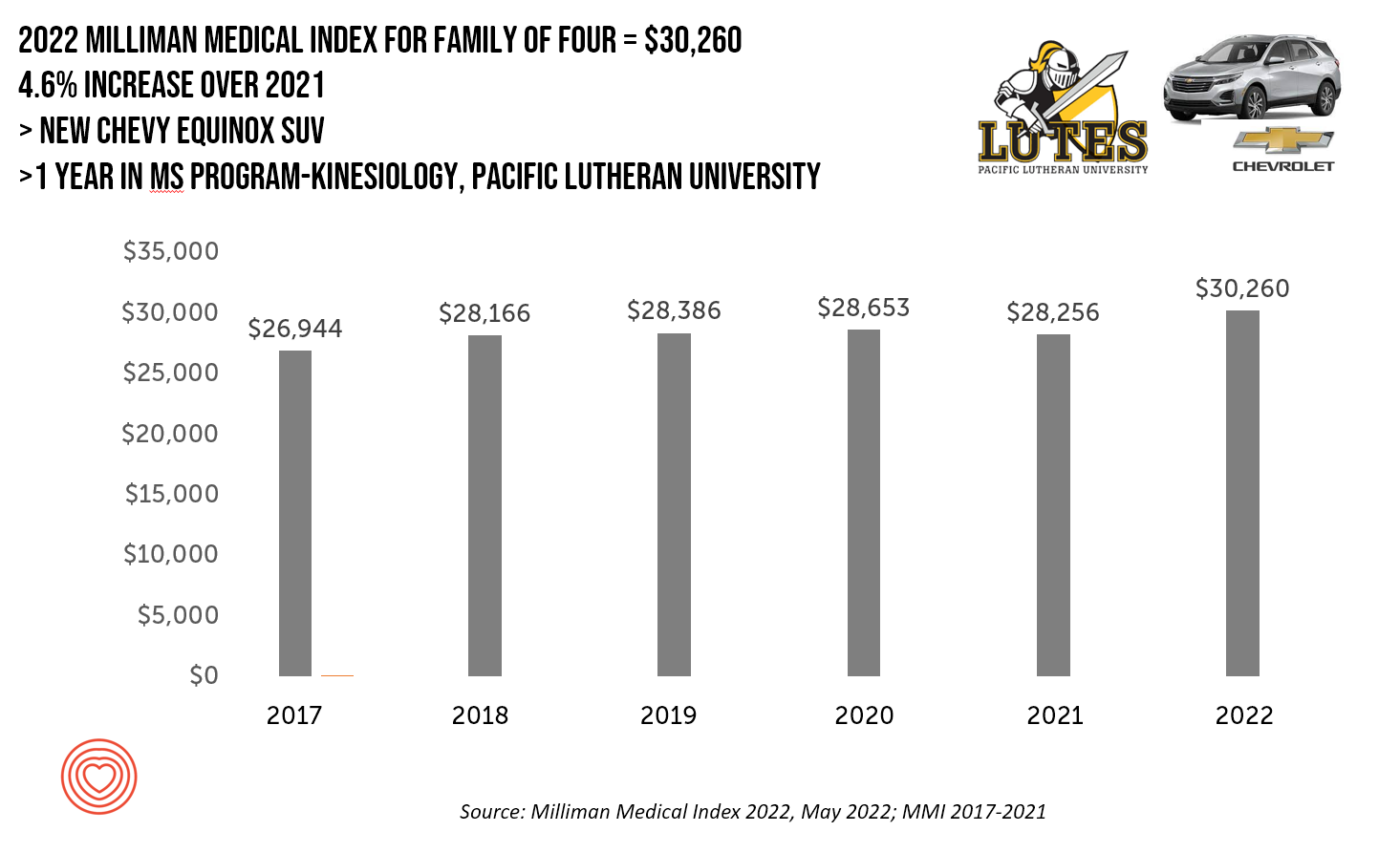
A new Chevy Equinox SUV, a year in an MS program in kinesiology at Pacific Lutheran U., or health care for a family of four. At $30,260, you could pick one of these three options. Welcome to this year’s 2022 Milliman Medical Index, which annually calculates the health care costs for a median family of 4 in the U.S. I perennially select two alternative purchases for you to consider aligning with the MMI medical index. I have often picked a new car at list price and a year’s tuition at a U.S. institution of
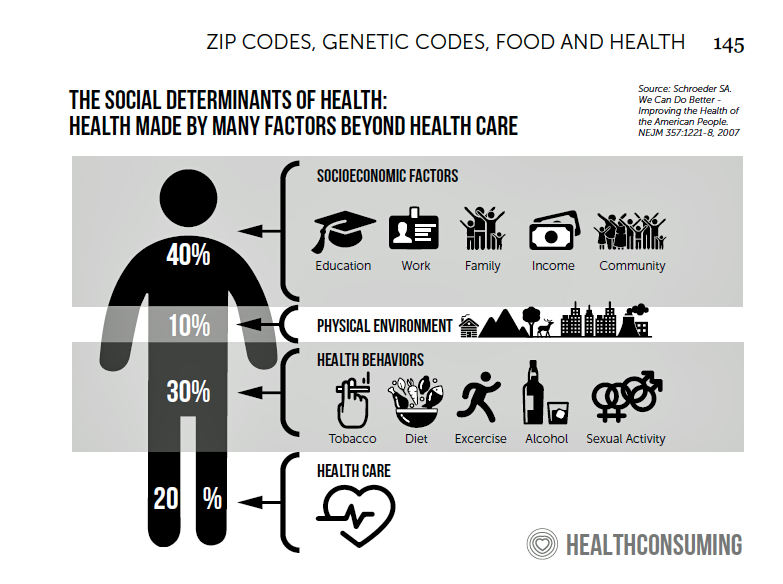
Social Determinants of Health Risks Challenge the Promise of Hospital-to-Home
In the wake of the pandemic and growing consumer preferences, the hospital-to-home movement is gaining traction among health systems. Amidst bullish forecasts for the promise of hospital-to-home discharges, the ability for many patients to make this migration would be a difficult bridge to cross. On the promising front, recent studies reviewed through a meta-analysis published in JAMA found that hospital-to-home programs can be clinically and cost-effective for inpatients discharged from hospital. Earlier this year, McKinsey addressed how “Care at Home” ecosystems can reshape the way health systems — and people — envision patient care. This
Reimagining Health Care Without Walls – Deloitte’s Vision
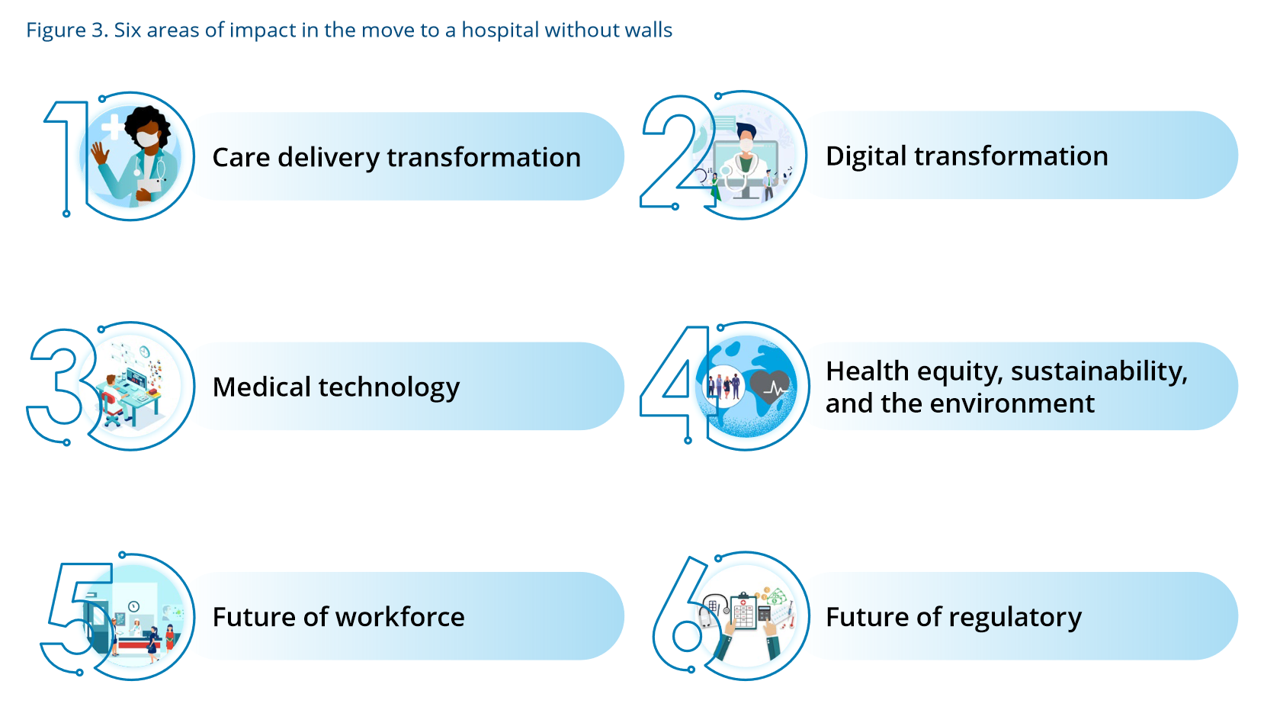
Delivering health care during the heights of the COVID-19 pandemic proved to both patients and their clinicians that virtual care was not only a viable channel for care, but very often a preferable “place” to collaborate for treatment. Even before the coronavirus pandemic emerged in early 2020, telehealth and the hospital-to-home movement were beginning to become part of a portfolio of delivery modes across the continuum of care. Deloitte spells out the current and future prospects for the Hospital in the future “without” walls in a new report that spells out driving forces, future scenarios, and impacts on a business long
Thinking About Telehealth Through the Lens of Real Estate – Listening to JLL
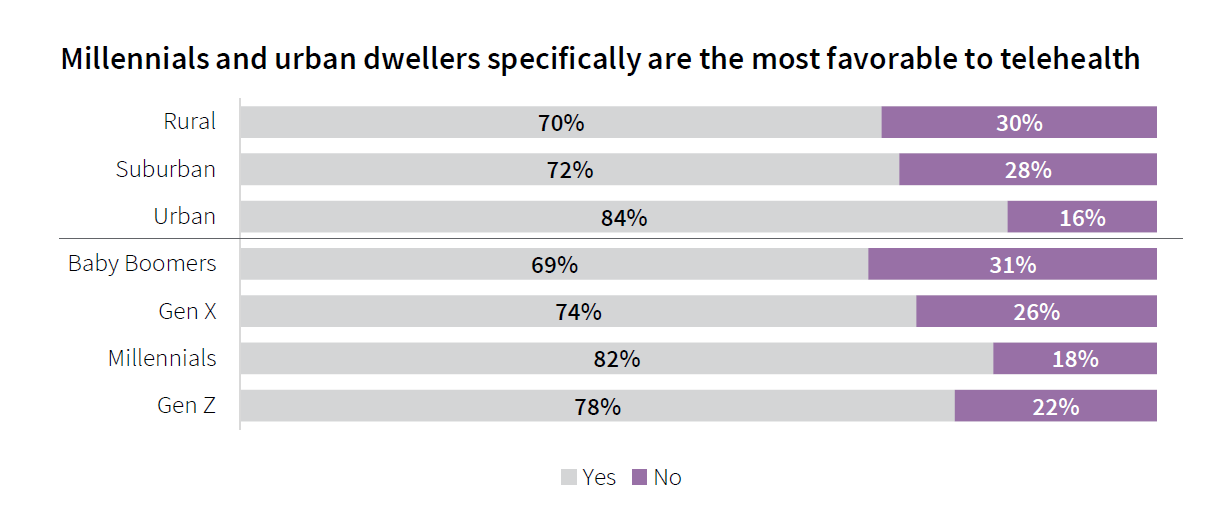
If you made your living in commercial real estate — and especially, working with hospitals’ and health systems’ office space — would the concept of telehealth be freaking you out right now? If you heed the words of JLL’s 2022 Patient Consumer Survey, you’d chill (at least a bit). The tagline on this paper is, “Convenience and choice drive patient decisions as new digital options take hold.” I was particularly keen to dig into this study based on its sponsoring organization: JLL is a real estate services company serving over a dozen vertical markets — including health care, life sciences,
Medical Distancing Is Bad For Your Health

“Social distancing is great. Medical distancing? Not so much,” I observe in Medical Distancing in America: A Lingering Pandemic Side Effect., my essay published this week in Medecision’s Liberate Health blog. Since we learned to spell “coronavirus,” we also learned the meaning and risk-managing importance of physical distance early in the COVID-19 pandemic. But medical distancing became a corollary life-flow of the physical version, and for our collective health and well-being, it hasn’t been good for our health in ways beyond keeping our exposure to the virus at bay. For health care providers — physicians, hospitals, ambulatory clinics, diagnostic centers —
Nurses Continue to Rule in Honesty and Ethics in U.S. Professions – Healthcare Professions Still Top Gallup’s Annual Poll
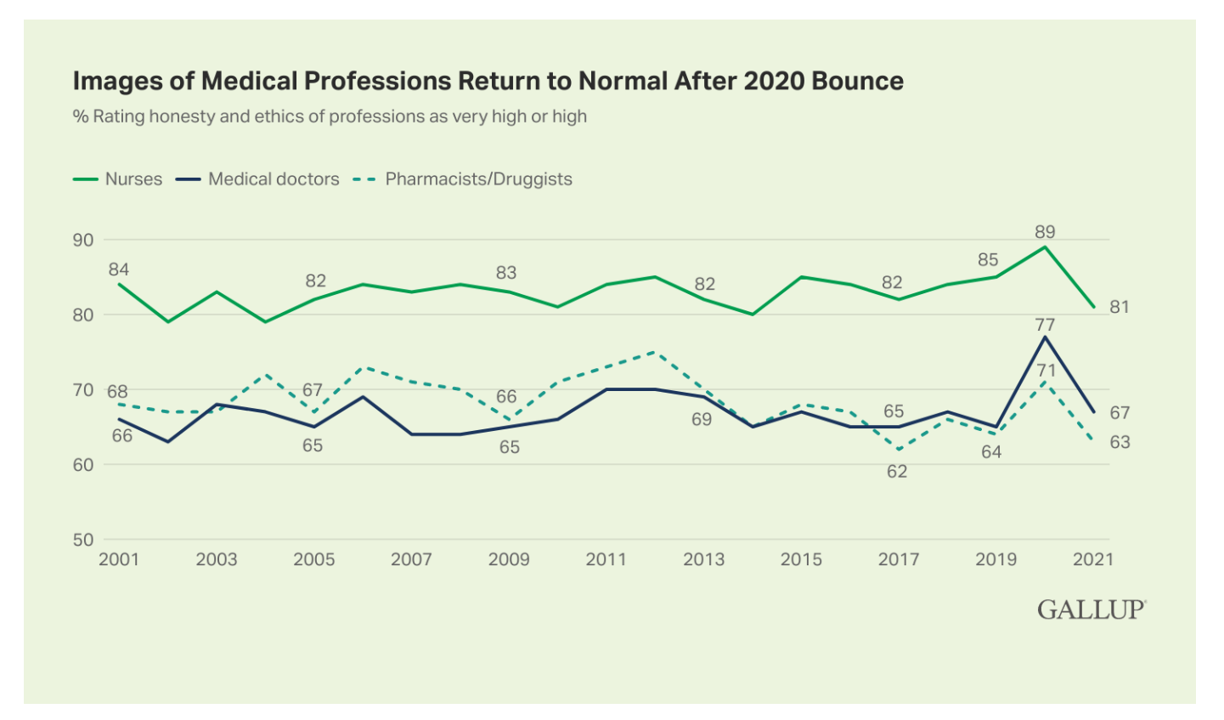
Three health care professions rank in the top four of the most honest and ethical rankings in Gallup’s annual poll on honesty and ethics in professions. And nurses are at the top of the list for the 20th year in a row. Grade-school teachers ranked third place between physicians and pharmacists, shown in the big chart of job types from most ethical to least. Perennially, the bottom-ranked posts are a mix of politicians (Members of Congress and lobbyists, state office holders), car salespeople, and the Mad Men and Women of advertising. Media professionals in TV and newspapers also polled relatively
Health Care Planning for 2022 – Start with a Pandemic, Then Pivot to Health and Happiness

One of my favorite Dr. Seuss characters is the narrator featured in the book, I Had Trouble In Getting to Solla-Sollew. I frequently use this book when conducting futures and scenario planning sessions with clients in health/care. “The story opens with our happy-go-lucky narrator taking a stroll through the Valley of Vung where nothing went wrong,” the Seussblog explains. Then one day, our hero (shown here on the right side of the picture from the book) is not paying attention to where he is walking….thus admitting, “And I learned there are troubles of more than one kind, some come from
“The Front Line Is Shrinking:” Nurses Re-Imagine Nursing at the #NurseHack4Health Hackathon

While nurses were in short supply before 2020, the coronavirus pandemic and stress on front-line health care workers exacerbated the shortage of nursing staff globally. This urgent call-to-action became the rallying cry and objective for this weekend’s #NurseHack4Health, “The Front Line Is Shrinking,” with the goal of building a sustainable workforce of the future. I’m grateful to the nurse leadership teams at Johnson & Johnson, Microsoft, and Sonsiel for inviting me to participate in another round of the #NurseHack4Health hackathon pitches over the past weekend. This year inspired nearly 800 registrants from at least 48 countries to convene via Microsoft
How Healthcare Experience Ranks Versus Other Industries (Not So Great)
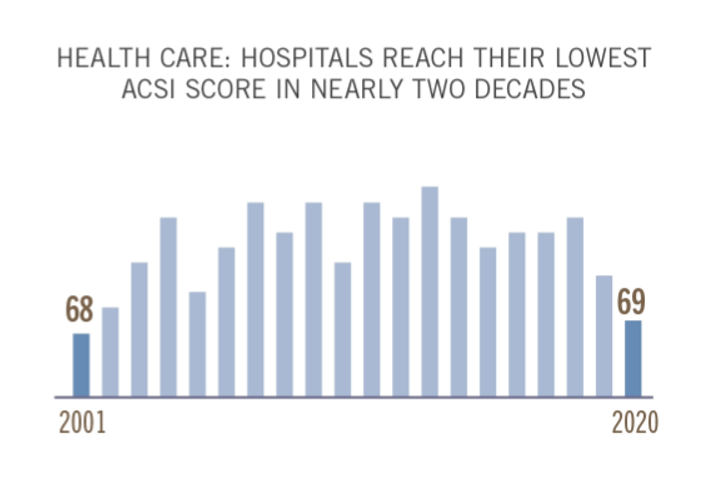
The coronavirus pandemic put health care at the top of peoples’ minds all over the world. As important as health became to humans at the base of our Hierachies of Needs, in the U.S., health care industries fell to their lowest consumer satisfaction scores in two decades, we learn in the latest evaluation by the American Consumer Satisfaction Index report. I explore consumer-patient experience for hospitals, health plans and ambulatory care compared with other industries in the November 2021 Medecision Liberation blog, calling out the importance of two key factors that drove peoples’ positive perceptions of brands and products in
Designing Digital Health for Public Health Preparedness and Equity: the Consumer Tech Association Doubles Down
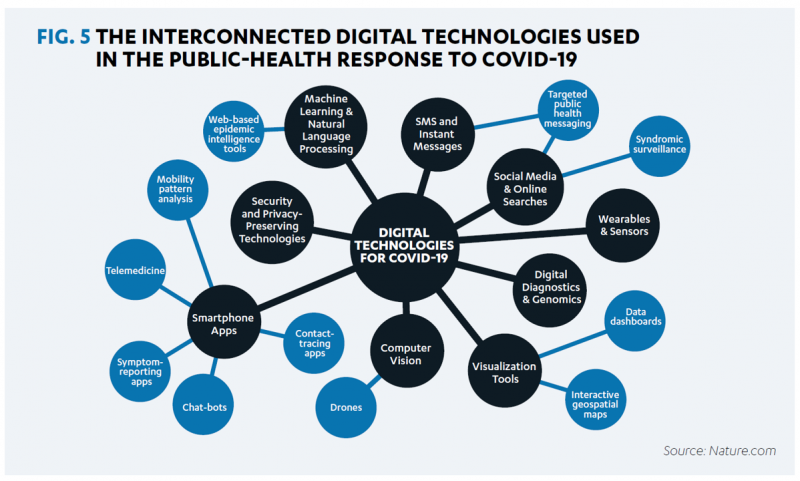
A coalition of health care providers, health plans, technology innovators, NGOs, and medical societies has come together as the Public Health Tech Initiative (PHTI), endorsed by the Consumer Technology Association (CTA) with the goal of advancing the use of trustworthy digital health to proactively meet the challenge of future public health emergencies….like pandemics. At the same time, CTA has published a paper on Advancing Health Equity Through Technology which complements and reinforces the PHTI announcement and objective. The paper that details the PHTI program, Using Heath Technology to Response to Public Health Emergencies, identifies the two focus areas: Digital health
Be Mindful About What Makes Health at HLTH
“More than a year and a half into the COVID-19 outbreak, the recent spread of the highly transmissible delta variant in the United States has extended severe financial and health problems in the lives of many households across the country — disproportionately impacting people of color and people with low income,” reports Household Experiences in America During the Delta Variant Outbreak, a new analysis from the Robert Wood Johnson Foundation, NPR, and the Harvard Chan School of Public Health. As the HLTH conference convenes over 6,000 digital health innovators live, in person, in Boston in the wake of the delta
A Negative Outlook for US Hospital Margins Through 2021
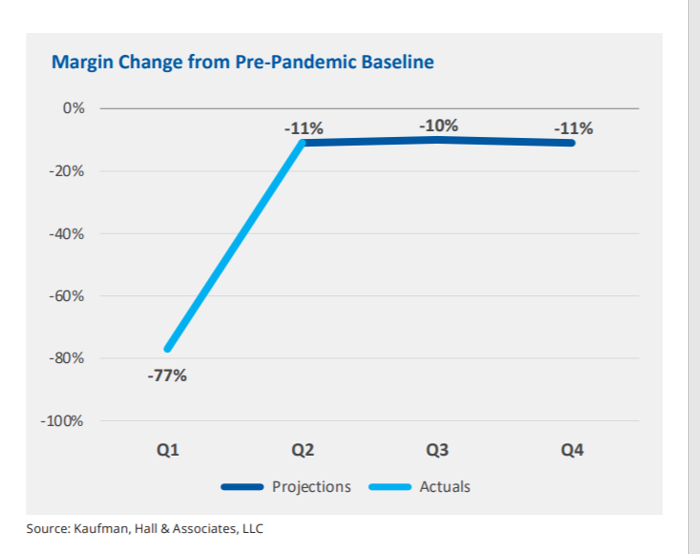
In the fourth quarter of 2021, U.S. hospital margins will still be lower than before the COVID-19 pandemic, Kaufman, Hall & Associates project in their latest read on hospital finances. Kaufman Hall has been monitoring hospitals’ financial health in the coronavirus era since March 2020, month-by-month. This new report looks into the Financial Effects of COVID-19: Hospital Outlook for the Remainder of 2021. This report was conducted on behalf of the American Hospital Association (AHA), who succinctly summarized the forecast saying, “COVID-19 [is] expected to drive continued hospital losses throughout 2021.” That projection is further couched in the concern that
#HelloHumankindness and Happy New Year….

When Dignity Health, the Catholic health care system, launched the “Hello humankindness” PR campaign in June 2013, well, they had me at “Hello.” When the project went live, Dignity Health’s President/CEO Lloyd Dean provided the rationale for the program, saying: “What’s missing in the public discourse about health care is the fact that while medicine has the power to cure, it’s humanity that holds the power to heal.” Dean pointed to two drivers shaping U.S. culture and the nation’s health care industry: The institutionalization of health care, and, The decline of civility in society. That was 2013. #HelloHumankindness sought to
New Primary Care, Retail and Tech Entrants Motivating Hospitals to Grow Consumer Chops
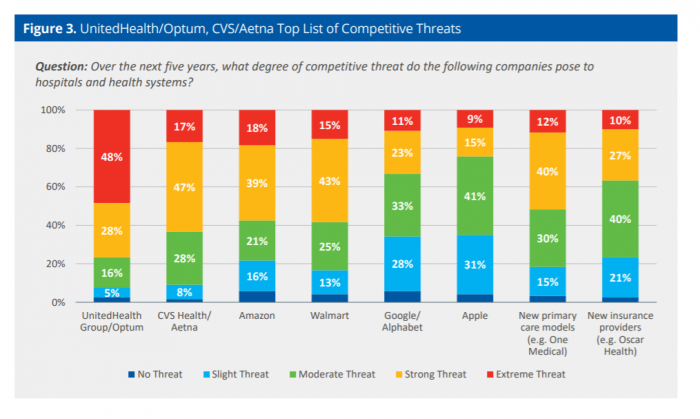
Rising costs, generational shifts, digital transformation, and fast-growing investments in new health care models and technologies are forcing change in the legacy health care, noted in the State of Consumerism in Healthcare 2021: Regaining Momentum, from Kaufman, Hall & Associates. As the title of Kaufman Hall’s sixth annual report suggests, health care consumers are evolving — even if the traditional healthcare system hasn’t uniformly responded in lock step with more demanding patients. Kaufman Hall analyzed 100 health care organizations in this year’s consumerism survey to assess their readiness to embrace consumer-centric strategies, understand how the industry prioritizes these approaches, evaluate
Nurses and Aides Are Beloved and Deserve Higher Pay; and a Spotlight on the Filipinx Frontline
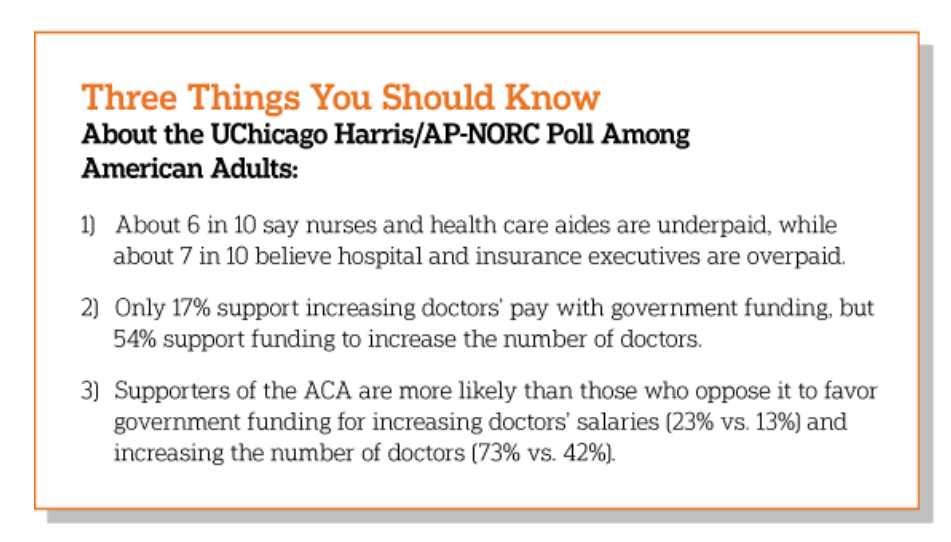
A majority of Democrats, Independents, and Republicans agree that nurses are underpaid. Most Americans across political parties also believe that hospital executives are overpaid, according to a poll from The Associated Press-NORC Center for Public Affairs Research. The survey analysis is aptly titled, Most Americans Agree That Nurses and Aides Are Underpaid, While Few Support Using Federal Dollars to Increase Pay for Doctors, . Insurance executives are also overpaid, according to 73% of Americans — an even higher percent of people than the 68% saying hospital execs make too much money. In addition to nurses being underpaid, 6 in 10
Our Pandemic Lessons: Listening to Michael Dowling – a #HIMSS21 Wrap-Up

“We don’t un-learn,” Dr. Amy Abernethy asserted as she shared her pandemic perspectives on a panel with 2 other former U.S. health policy and regulatory leaders. The three spoke about navigating compliance (think: regulations and reimbursement) in an uncertain world. An uncertain world is our workplace in the health/care ecosystem, globally, in this moment. So to give us some comfort in our collective foxhole, my last post for this week of immersion in #HIMSS21 is based on the keynote speech of Michael Dowling, CEO of Northwell Health. Dowling keynoted on the theme of “Leading for the Future,” sharing his lessons
IoT and The Rise of the Machines in Healthcare
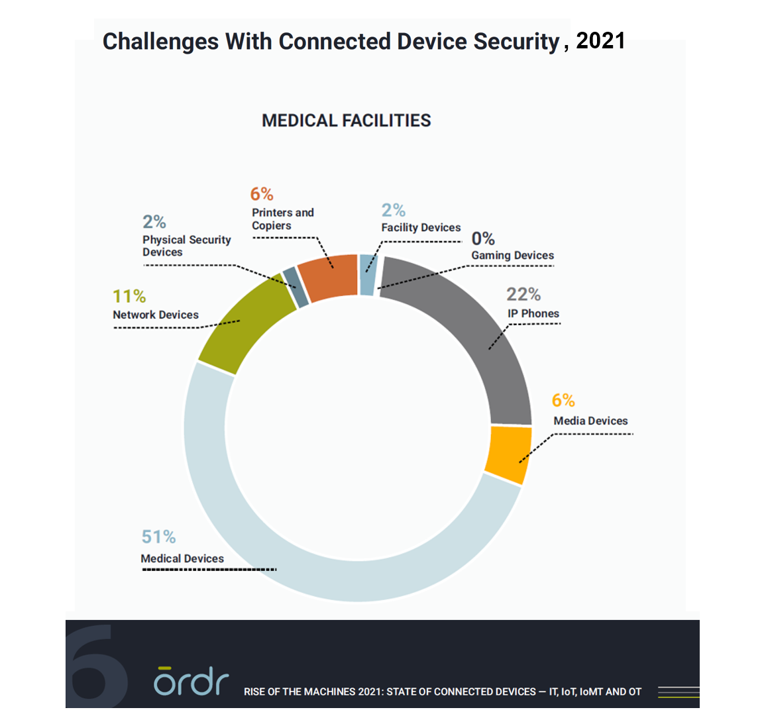
As connected devices proliferate within health care enterprises and across the health care ecosystem, cybersecurity risks abound. During the first year of the COVID-19 pandemic, the health care sector was profoundly affected by cyber-attacks on connected devices, we learn in the report, Rise of the Machines 2021: State of Connected Devices – IT, IoT, IoMT and OT from Ordr. For this annual report, Ordr analyzed security risks across over 500 deployments in healthcare, life sciences, retail, and manufacturing sectors for the 12 months June 2020 through June 2021. In health care, outdated operating systems present some of the greatest risks:
Healthcare Via the Cloud, Across the Enterprise and in the Patient’s Home – a Sustainable View from Philips at HIMSS 2021
The COVID-19 pandemic sparked a reappraisal of value-based care, a shift to remote and virtual care, and acceleration of healthcare stakeholders’ investments in Artificial Intelligence-based solutions, Philips discovered in the 2021 Future Health Index, the company’s latest survey conducted among 2,800 health care leaders working in 14 countries. This week at the 2021 annual HIMSS conference, Philips is “making the case for moving to the cloud,” discussing the Philips HealthSuite, a cloud-based platform for connecting providers and patients, devices (and the data they generate), and care across the health care continuum. That’s a big promise and vision, so to kick
Can the U.S. Improve Health System Performance with Digital Health Tools? Pondering A Big Question for #HIMSS21
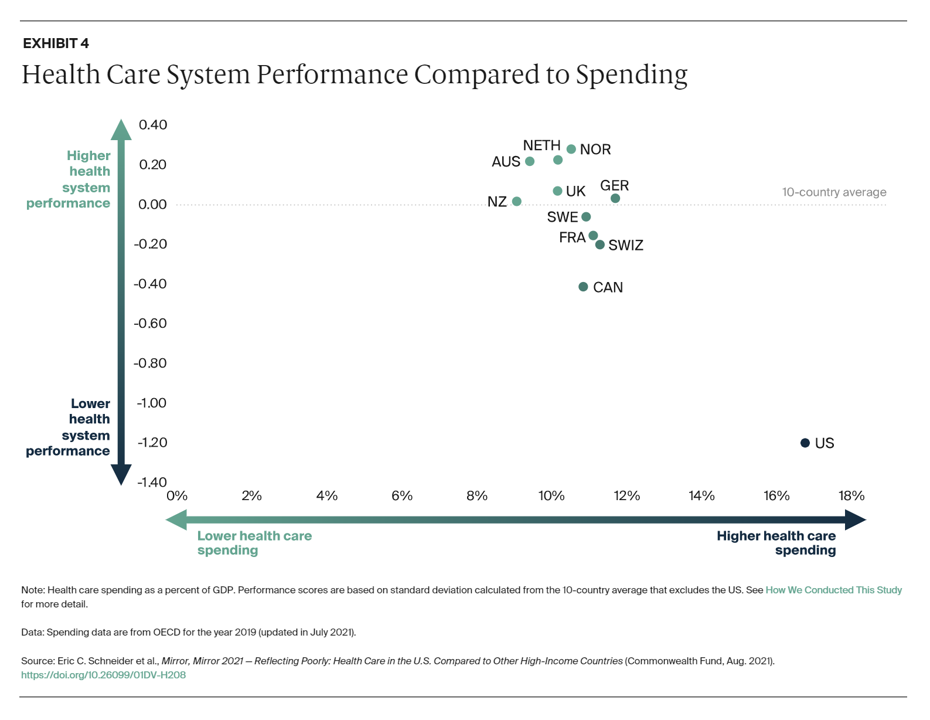
Simply put, is the equation, “Spend more, get less” a sustainable business model? Of course not. But that’s the simple math on U.S. health care spending and what comes from it, according to Mirror, Mirror 2021: Reflecting Poorly, a perennial report from The Commonwealth Fund that compares health system performance across eleven developed countries. The first table details the metrics that the Fund compares across the eleven peer nations, which included Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States. The metrics compared were access to care, care process, administrative efficiency, equity,
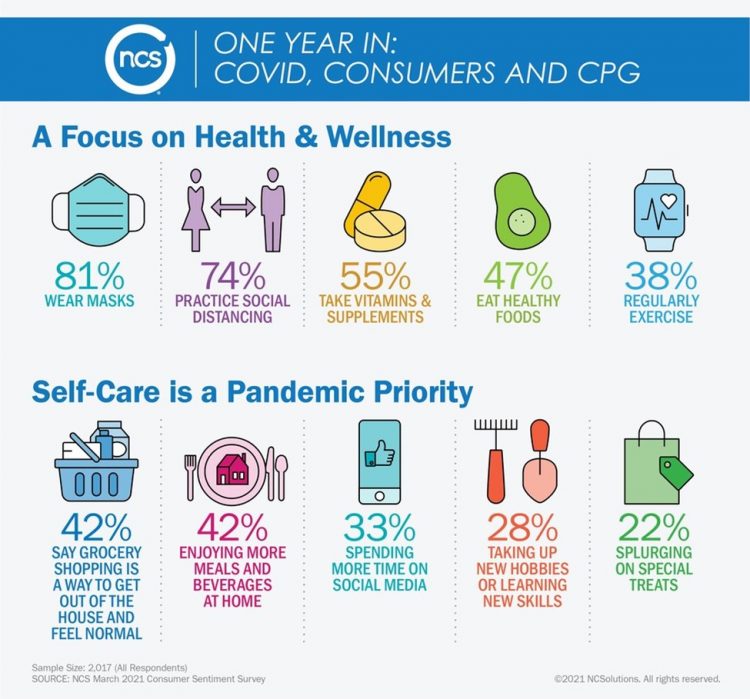
Healthy Living Trends Inspired by COVID-19: Retailers, Food, and Consumers’ Growing Self-Care Muscles
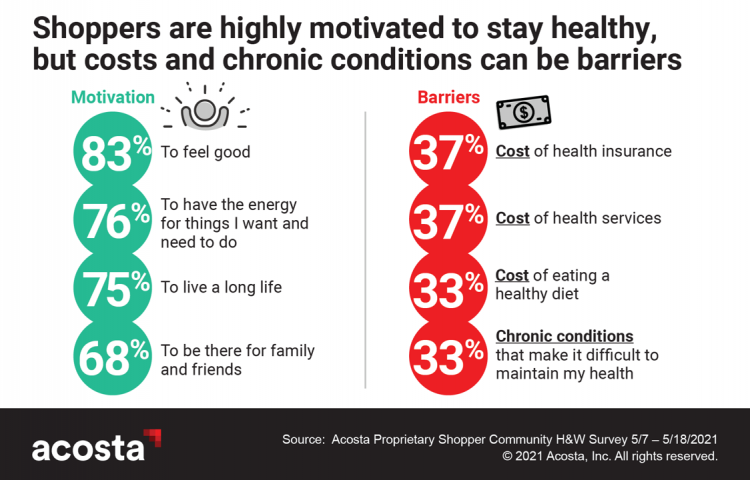
“Self-care” took on new meaning and personal work-flows for people living in and through the coronavirus pandemic in the U.S. Acosta, the retail market research pro’s, updated our understanding consumers evolving as COVID-19 Has Elevated the Health and Wellness Trends of the Recent Years, results of a survey conducted among in May 2021. In the U.S., consumers’ take on self-care has most to do with healthy eating and nutrition (for 1 in 2 people), getting regular medical checkups (for 42%), taking exercise, relaxing, using vitamins and supplements, and getting good sleep. Healthy relationships are an integral part of self-care for
The Digital Home: A Platform for Health, via Deloitte and the COVID-19 “Stress Test”
Wherever you live in the world touched by the coronavirus pandemic, you felt (and were) stress-tested. Both you were, and your home was as well. In this year’s 2021 annual report by Deloitte into Connectivity & Mobile Trends, their report details How the pandemic has stress-tested the crowded digital home. This analysis was done, as it is every year, by the Deloitte Center for Technology, Media & Telecommunications. Deloitte’s Center commissioned an online survey among 2,009 U.S. consumers to gauge five generations of peoples’ perspectives on connected life in the context of COVID. The report covers the various life-flows of
Healthcare, Heal Thyself! How the Industry Can and Should Play the Trust Card
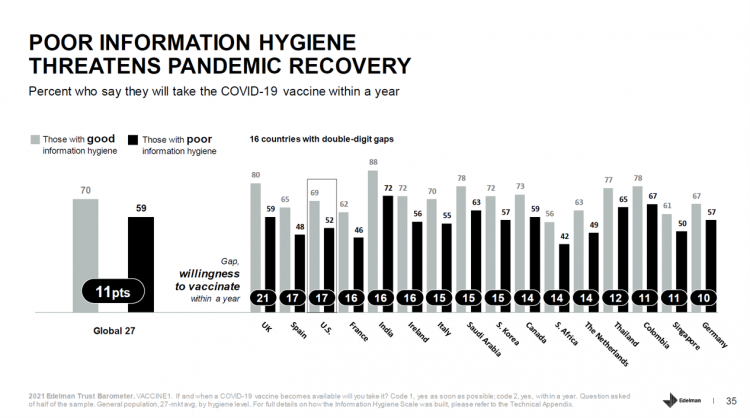
The emergence of the COVID-19 vaccine “infodemic” has slowed the ability for nations around the world to emerge out of the public health crisis. Growing cynicism among some health citizens facing the politicization of public health tactics like vaccines and facial masks is what we’re talking about. At the root is peoples’ lack of trust across a range of information providers, including government, media, business, and even peers. The 2021 Edelman Trust Barometer spotlighted the infodemic and eroding trust in the U.S. in the voices of public health, the public sector, and media. This is a global challenge as well,
The ROI on Virtual Care – Thinking About Value and Future Prospects With the AMA
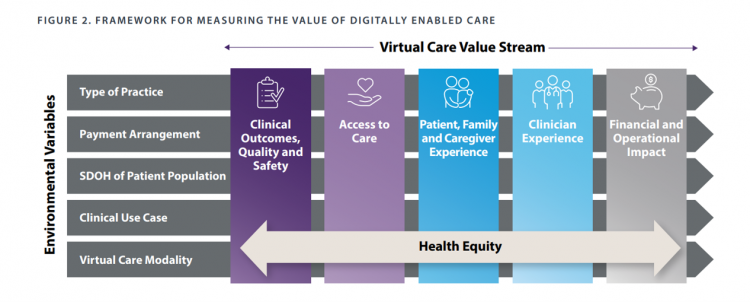
When a new technology or product starts to get used in a market, it follows a diffusion curve whose slope depends on the pace of adoption in that market. For telehealth, that S-curve has had a very long and fairly flat front-end of the “S” followed by a hockey stick trajectory in March and April 2020 as the COVID-19 pandemic was an exogenous shock to in-person health care delivery. The first chart from the CDC illustrates that dramatic growth in the use of telehealth ratcheting up since the first case of COVID-19 was diagnosed in the U.S. Virtual care has
Trust in Healthcare is Under Stress in the US and Globally, Edelman Finds
You’re stressed, I’m stressed; most of us have felt stress in the COVID-19 era which began in the U.S. in the first quarter of 2020. Nearly eighteen months later, a 2021 Edelman Trust Barometer update finds that consumers’ trust in the health care industry is under stress, too — in the U.S. and around the world. The first chart from the Edelman health care update demonstrates that in most countries polled, health citizens’ trust in health care was buoyed in the first five months of 2020 (January through May): up 18 points in the U.S., 14 points in Canada and
Nurses Hacking for Health and Compassionomics

The hearts and minds of nurses are fertile and inspirational sources and engines for health care innovation. This past weekend, and for the second time, I had the privilege and opportunity to be a panelist for the perennial hackathon meet-up of Nurse Hack 4 Health, sponsored by Microsoft, Johnson & Johnson, Sonsiel, and DevUp. This round, the hackathon attracted hundreds of nurses from at least 20 countries and 30 U.S. states. Even a few students attended, a growing trend as academia recognizes the shortage of workers trained to solve thorny problems of the world. In health care, right here, right
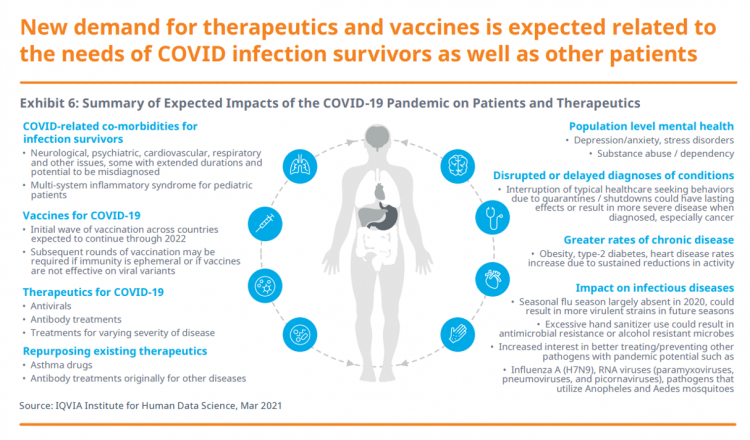
Spending on Medicines In and Post-COVID Say a Lot About Patients and Larger Healthcare Trends – an IQVIA Update
Spending on medicines, globally, will rebound this year and rise above pre-pandemic levels through 2025. Between 2021 and 2025, the annual growth global growth rate for prescription drugs spending is expected to range from 3% to 6%, a $1.6 trillion bill for the worlds’s total Rx medicines market. That relatively low single-digit growth rate is tempered by savings from biosimilars and the loss of brand exclusivity (that is, more generics coming to market). On the faster-growth side, we can expect two big therapeutic areas to drive spending upward: oncology and immunology, projected to expand by 9% to 12% each year
Virtual Health Tech Enables the Continuum of Health from Hospital to Home

In the COVID-19 pandemic, as peoples’ daily lives shifted closer and closer to home, and for some weeks and months home-all-the-time, health care, too, moved beyond brick-and-mortar hospitals and doctors’ offices. The public health crisis accelerated “what’s next” for health care delivery, detailed in A New Era of Virtual Health, a report published by TripleTree. TripleTree is an investment bank that has advised health care transactions since 1997. As such, the team has been involved in digital health financing and innovation for 24 years, well before the kind of platforms, APIs, and cloud computing now enabling telehealth and care, everywhere. The
The Pandemic’s Death Rate in the U.S.: High Per Capita Income, High Mortality
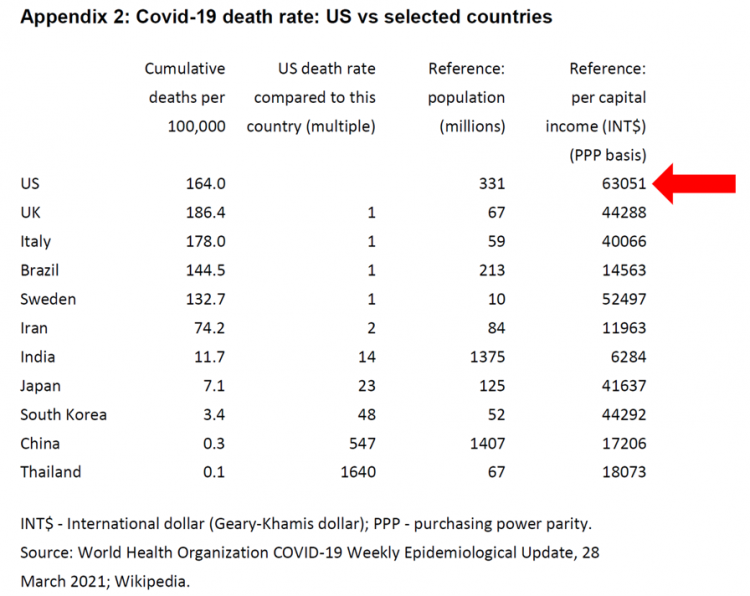
The United States has among the highest per capita incomes in the world. The U.S. also has sustained among the highest death rates per 100,000 people due to COVID-19, based on epidemiological data from the World Health Organization’s March 28, 2021, update. Higher incomes won’t prevent a person from death-by-coronavirus, but risks for the social determinants of health — exacerbated by income inequality — will and do. I have the good fortune of access to a study group paper shared by Paul Sheard, Research Fellow at the Mossaver-Rahmani Center for Business and Government at the Harvard Kennedy School. In reviewing
Emerging with A Stronger Healthcare System Post-COVID: NAM’s Lessons Learned
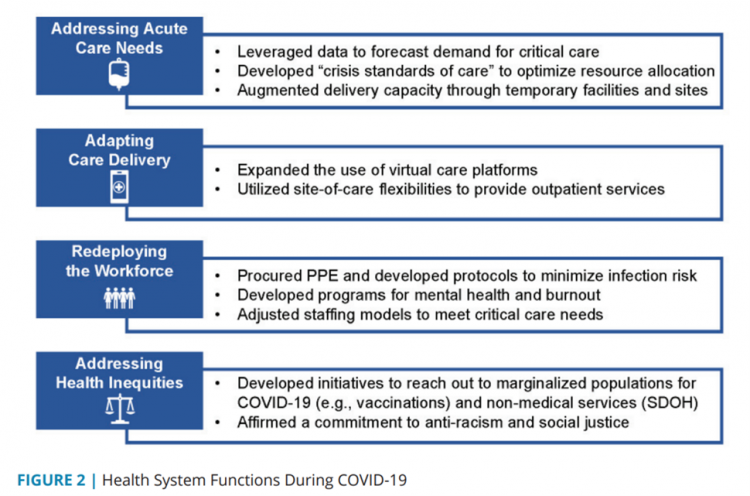
The coronavirus pandemic exposed weaknesses in the U.S. health care system that existed before the public health crisis. What lessons can be learned from the COVID-19 stress-test to build American health care back better? The National Academy of Medicine is publishing nine reports addressing health stakeholder segments impacted and re-shaped by COVID-19 — for public health, quality and safety, health care payers, clinicians, research, patients-families-communities, health product manufacturers, digital health, and care systems. The report on health care systems and providers was released this week: COVID-19 Impact Assessment: Lessons Learned and Compelling Needs was authored by experts on the front-line
Housing as Prescription for Health/Care – in Medecision Liberation

COVID-19 ushered in the era of our homes as safe havens for work, shopping, education, fitness-awaking, bread-baking, and health-making. In my latest essay written for Medecision, I weave together new and important data and evidence supporting the basic social determinant of health — shelter, housing, home — and some innovations supporting housing-as-medicine from CVS Health, UnitedHealth Group, AHIP, Brookings Institution, the Urban Land Institute, and other stakeholders learning how housing underpins our health — physical, mental, financial. Read about a wonderful development from Communidad Partners, working with the Veritas Impact Partners group, channeling telehealth to housing programs serving residents with
How Grocery and Retail Companies Are Delivering Health and Healthcare
The Wall Street Journal featured the grocery chain Kroger in an article yesterday titled, COVID-19 Vaccinations, Tests Give Boost to Kroger’s Health Ambitions. “With 2,250 pharmacies and 220 clinics largely in the Midwest and the southern U.S., Kroger is the fourth-largest pharmacy operator by script count,” the Journal noted, adding details about Walmart, CVS Health, and Walgreens all fast-expanding their respective health care footprints. As more consumers view their homes as personal and safe health havens, there is no shortage of suppliers in the food, retail, and mobility sectors working fast to meet that demand for convenient and accessible services.
2020 Was Our Year of COVID; 2021 Will Be Our Year of Vaccines and Excess Deaths in America
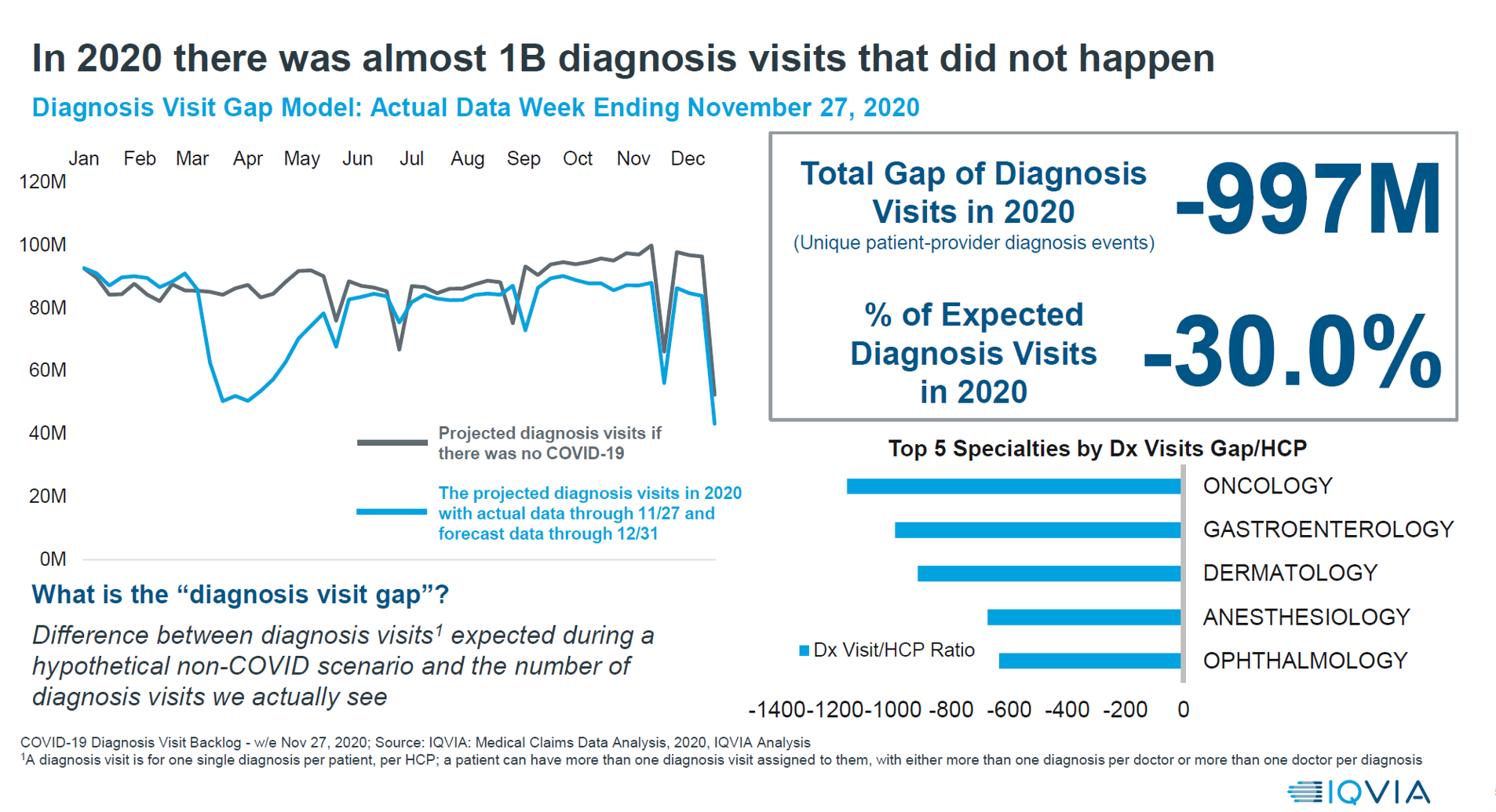
With a third vaccine approved by the FDA for licking COVID-19, brought to market by Johnson & Johnson, the U.S. can expect an uptick in vaccinations among fellow health citizens. That’s such welcome news and a positive outlook for a healthier 2021. But there’s another angle on 2021 for which health care providers and health citizens alike should prepare: that is the excess deaths that will happen due to patients postponing needed health care, diagnostic tests, and preventive services that stem from people avoiding care in doctor’s offices and hospitals. The chart here comes from IQVIA’s latest study into COVID-19’s
Hospitals Continue to Lose Money in Year 2 of the Pandemic
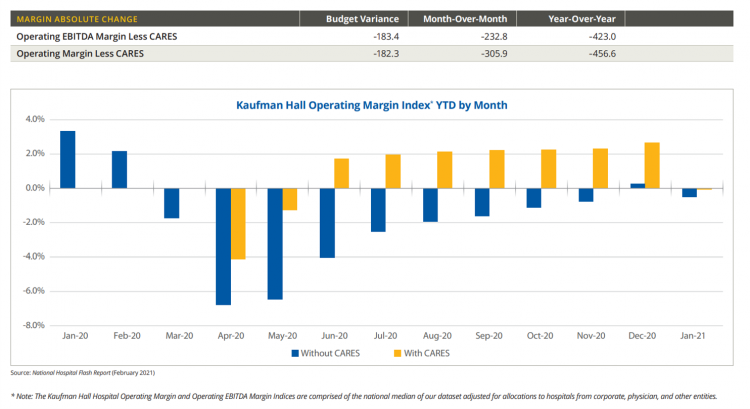
U.S. hospitals’ operating margins went negative in January 2021 after turning north for the first time in December 2020 since the start of the coronavirus pandemic, according to the February 2021 Hospital Flash Report from Kaufman Hall, commissioned by AHA, the American Hospitals Association. The first chart illustrates the importance of CARES Act funding to keep hospitals financially afloat during the public health crisis through most of last year. The start of 2021 was difficult for hospitals and health systems, Kaufman Hall explains, with falling outpatient revenues and increasing expenses resulting in that below-the-line blue bar for January 2021’s operating
The Health Care Cost Curve is Bending Down – A New View from Deloitte
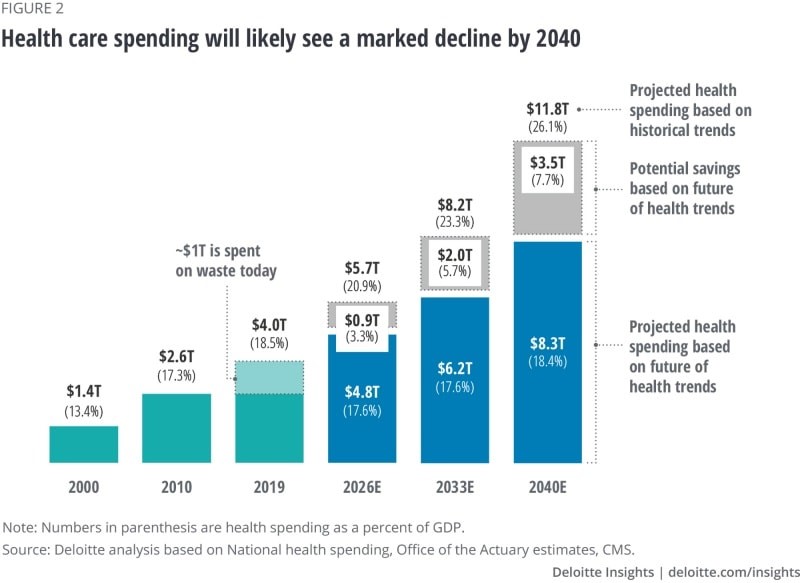
Over the next 20 years, health care spending in the U.S. will migrate toward well-being and the early detection of disease, away from the funding of America’s sick-care system, according to Breaking the cost curve, a forecast of U.S. health economics in the year 2040 from Deloitte. Current spending on health care in America is roughly $4 trillion (with a “t”) dollars, approaching 20% of the nation’s economy. By 2040, spending is projected to be $8.3 trillion based on future health trends — not historic workflows and delivery mechanisms which would consume an additional $3.5 trillion — close to what we
The Digital Transformation of Home for Health – Brainstorming with Karsten Russell-Wood of Philips

At the start of CES 2021, I had the opportunity to catch up with Karsten Russell-Wood, Portfolio Marketing Leader, Post Acute & Home, Connected Care at Philips. We brainstormed just as CES 2021 was going to “open,” virtually, for the consumer electronics conference’s first all-virtual meeting. Philips, a longtime major exhibitor at CES, created an entirely new online experience for the CES attendees – a sort of virtual gallery of different exhibits that are accessed from a single point in a “room” with various entry points. One of the company’s key messages for CES 2021 was health care delivered outside
Call It Deferring Services or Self-Rationing, U.S. Consumers Are Still Avoiding Medical Care
Patients in the U.S. have been self-rationing medical care for many years, well before any of us knew what “PPE” meant or how to spell “coronavirus.” Nearly a decade ago, I cited the Kaiser Family Foundation Health Security Watch of May 2012 here in Health Populi. The first chart here shows that one in four U.S. adults had problems paying medical bills, largely delaying care due to cost for a visit or for prescription drugs. Fast-forward to 2020, a few months into the pandemic in the U.S.: PwC found consumers were delaying treatment for chronic conditions. In October 2020, The American Cancer
Dr. Burnout – The 2021 Medscape Physician Burnout & Suicide Report
Physicians in the U.S. are experiencing “death by 1,000 cuts,” according to the 2021 Medscape Physician Burnout & Suicide Report. Medscape polled 12,339 physicians representing over 29 specialties between late August and early November 2020 to gauge their feelings about work and life in the midst of the coronavirus pandemic. Medscape researched its first Physician Lifestyle Report in 2012. That research focused on physician “happiness” and work-life satisfaction. In 2013, the issue of burnout was called out on the cover of the report, shown here with the question, “does burnout affect lifestyle?” In 2015, the Physician Lifestyle Report was titled,
Our Homes Are Health Delivery Platforms – The New Home Health/Care at CES 2021

The coronavirus pandemic disrupted and re-shaped the annual CES across so many respects — the meeting of thousands making up the global consumer tech community “met” virtually, both keynote and education sessions were pre-recorded, and the lovely serendipity of learning and meeting new concepts and contacts wasn’t so straightforward. But for those of us working with and innovating solutions for health and health care, #CES2021 was baked with health goodness, in and beyond “digital health” categories. In my consumer-facing health care work, I’ve adopted the mantra that our homes are our health hubs. Reflecting on my many conversations during CES
The Digital Consumer, Increasingly Connected to Health Devices; Parks Associates Kicking Off #CES2021

In 2020, the COVID-19 pandemic drove U.S. consumers to increase spending on electronics, notably laptops, smartphones, and desktop computers. But the coronavirus era also saw broadband households spending more on connecting health devices, with 42% of U.S. consumers owning digital health tech compared with 33% in 2015, according to research discussed in Supporting Today’s Connected Consumer from Parks Associates. developed for Sutherland, the digital transformation company. Consumer electronics purchase growth was, “likely driven by new social distancing guidelines brought on by COVID-19, which requires many individuals to work and attend school from home. Among the 26% of US broadband households
Preparing for a Long-COVID Lifestyle in 2021 – A Health-At-Home Focus for CES 2021

In the U.S., the latest read on supply-and-demand for COVID-19 vaccines illustrates a gap between what had been promised for the first phase of vaccine rollout versus the reality of supply chain challenges, cold storage, and 50-state and local fragmentation at the last mile for U.S. health citizens. An op-ed published in yesterday’s Washington Post by Dr. Robert Wachter of UCSF and Dr. Ashish Jha of Brown University found these two wise physicians feeling “punched in the face” with the state of coronavirus vaccination in America. As a result, they soberly, pragmatically recommended administering just the first jab of vaccine
Nurses, doctors, pharmacists join with teachers in Gallup’s 2021 honest and ethics poll
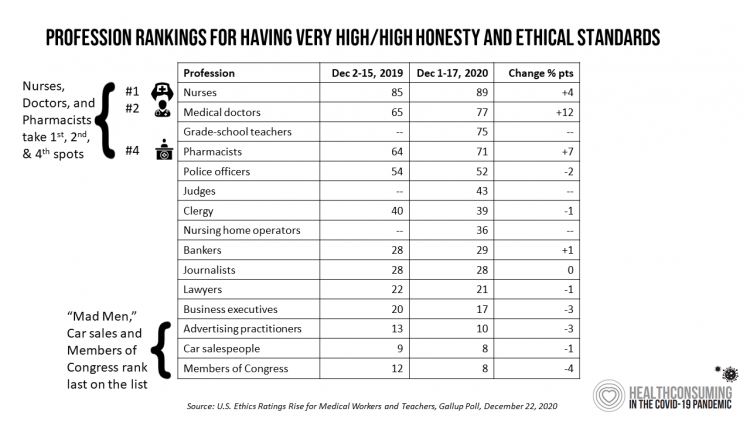
Each year, Americans rank nurses as the most honest and ethical professionals along, generally followed by doctors and pharmacists. In the middle of the coronavirus pandemic in the U.S., grade school teachers join the three medical professions in the annual Gallup Poll on the top-ranked professions for honest and ethical behavior in America as we enter 2021 with many U.S. hospitals’ intensive care units at full capacity….and schools largely emptied of students. The three health care professions scored their highest marks ever achieved in this Gallup Poll, which has been assessing honesty and ethics in America since 1999. Nurses are
The 2021 Health Populi TrendCast – Health Care, Self-Care, and the Rebirth of Love in Public Health

In numerology, the symbolic meaning behind the number “21” is death and re-birth. In tarot cards, 21 is a promise of fulfillment, triumph, and victory. How apropos that feels right now as we say goodbye and good riddance to 2020 and turn the page for a kinder, gentler, healthier New Year. It would be sinful to enter a New Year as challenging as 2021 promises to be without taking the many lessons of our 2020 pandemic life and pain into account. For health care in America, it is a time to re-build and re-imagine a better, more equitable landscape for
Will 2021 Be the Year of Sicker Americans? Pondering Late 2020 Data from IQVIA
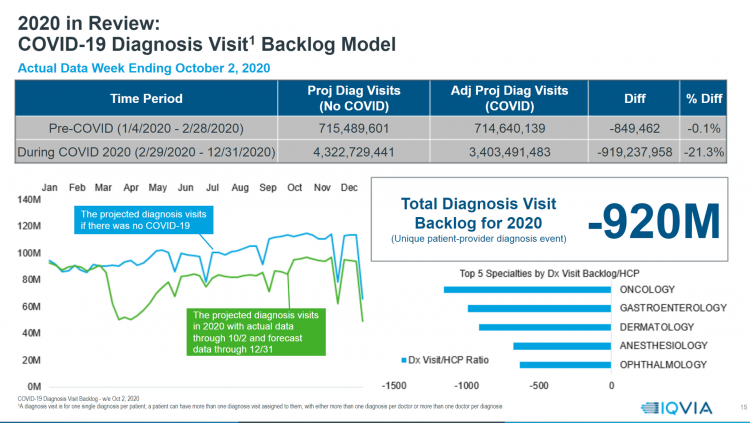
Yesterday, IQVIA presented their end-of-year data based on medical claims in the U.S. health care system tracking the ups, downs, and ups of the coronavirus in America. IQVIA has been tracking COVID-19 medical trends globally from early 2020. The plotline of patient encounters for vaccines, prescribed medicines, foregone procedures and diagnostic visits to doctors begs the question: in 2021, will Americans be “sicker,” discovering later-stage cancer diagnoses, higher levels of pain due to delayed hip procedures, and eroded quality of life due to leaky guts? Here are a few snapshots that paint a picture for greater morbidity and potentially more “excess
Home Is the Health Hub for Older People – Learning from Laurie Orlov
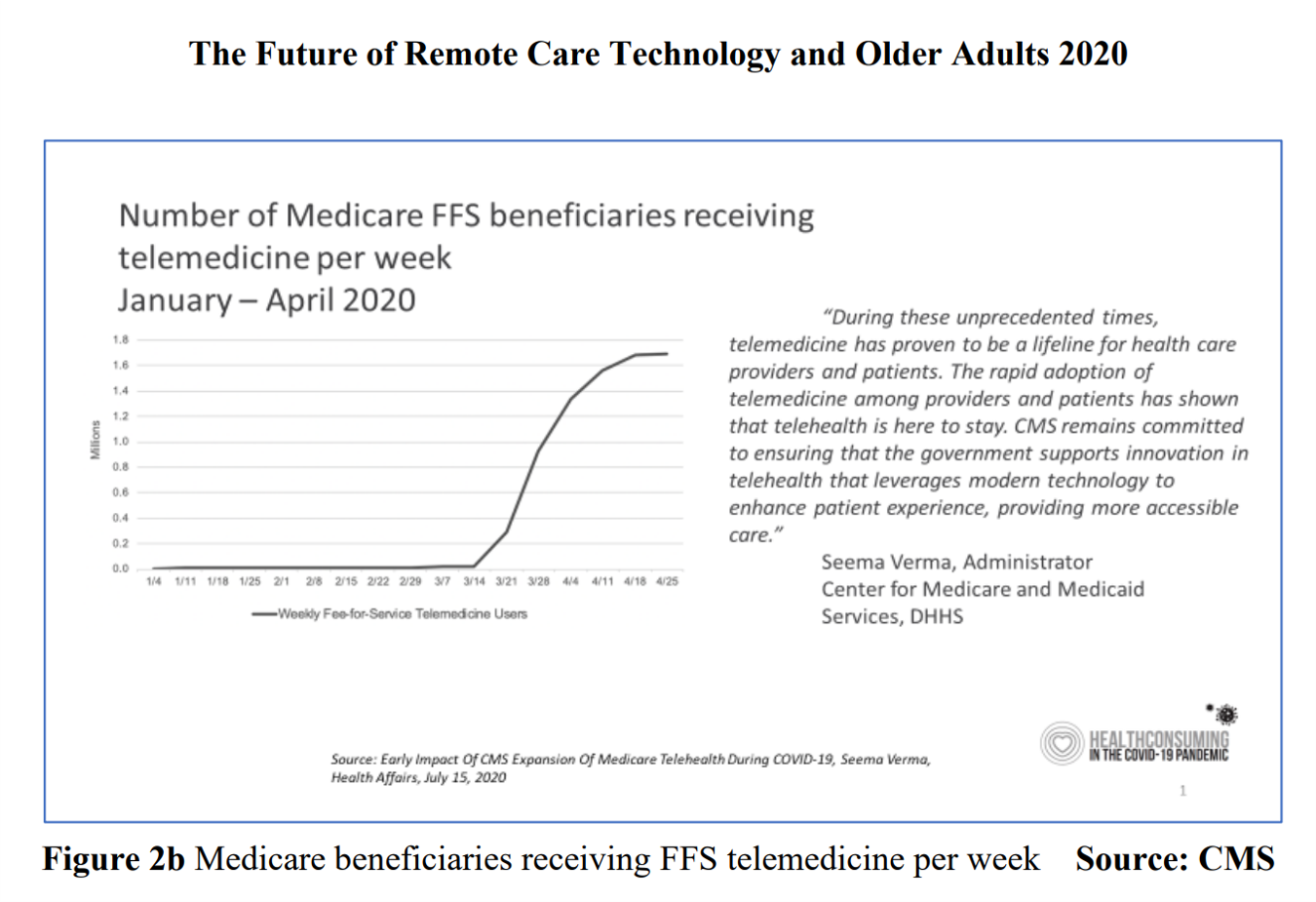
By April 2020, over one million Medicare members were receiving health care via telemedicine. The graph here shows you the hockey-stick growth for virtual care use by older Americans into the second month of the coronavirus pandemic. The COVID-19 public health crisis up-ended all aspects of daily living in America for people of all ages. For older Americans, avoiding the risk of contracting the tricky virus in public, and especially, in health care settings, became Job 1. The pandemic thus nudged older people toward adopting digital lifestyles for daily life, for shopping, for praying, and indeed, for health care. Laurie
The Comforts of Home Drive Demand for Healthcare There
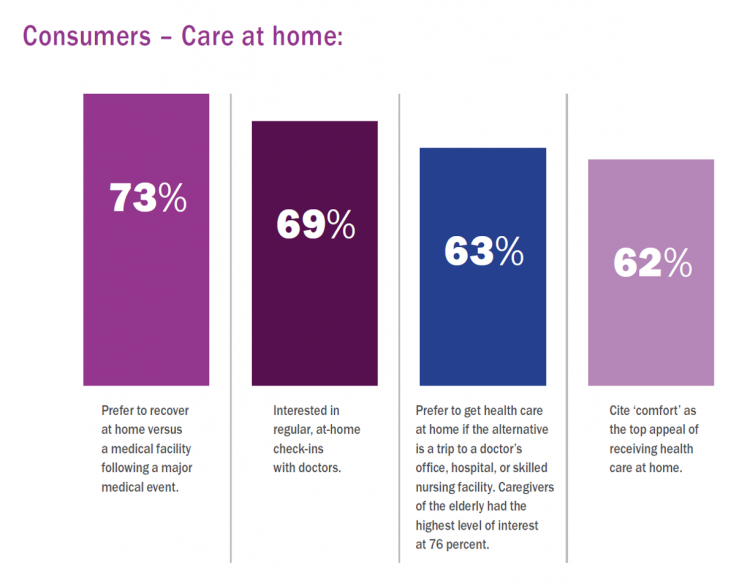
Two in three U.S. consumers skipped or delayed getting in-person medical care in 2020. One in 2 people had a telehealth visit int he last year. Most would use virtual care again. The coronavirus pandemic has mind-shifted how patients envision a health care visit. Today, most consumers prefer the idea of getting health care at home compared with going to a doctor’s office. Most Americans also like the idea of recovering at home instead of at a medical facility after a major medical event, according to the report, Health-at-Home 2020: The New Standard of Care Delivery from CareCentrix. COVID-19 has
Rebuilding Resilience, Trust, and Health – Deloitte’s Latest on Health Care and Sustainability
The COVID-19 pandemic has accelerated health care providers’ and plans’ investment in digital technologies while reducing capital spending on new physical assets, we learn in Building resilience during the COVID-19 pandemic and beyond from the Deloitte Center for Health Solutions. What must be built (or truly re-built), health care leaders believe, is first and foremost trust, followed by financial viability to ensure long-term resilience and sustainability — for the workforce, the organization, the community, and leaders themselves. For this report, Deloitte interviewed 60 health care chief financial officers to gauge their perspectives during the pandemic looking at the future of
Healthcare Costs, Access to Data, and Partnering With Providers: Patients’ Top User Experience Factors
As patients returned to in-person, brick-and-mortar health care settings after the first wave of COVID-19 pandemic, they re-enter the health care system with heightened consumer expectations, according to the Beryl Institute – Ipsos Px Pulse report, Consumer Perspectives on Patient Experience in the U.S. Ipsos conducted the survey research among 1,028 U.S. adults between 23 September and 5 October 2020 — giving consumers many months of living in the context of the coronavirus. This report is a must-read for people involved with patient and consumer health engagement in the U.S. and covers a range of issues. My focus in this
The Coronavirus Pandemic Turbocharged Digital Health Investment in 2020
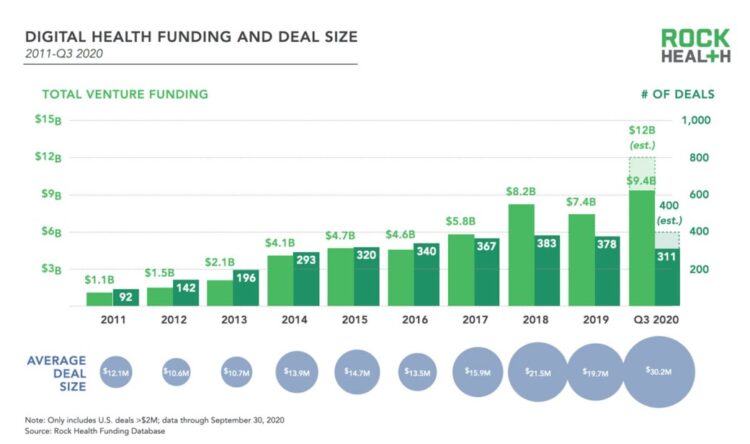
2020 will be remembered for disruption and dislocation on many fronts; among the major blips in the year will be it remembered as the largest funding year for digital health recorded, according to Rock Health’s report on the 3Q2020 digital health funding. This funding record (“already” before year-end, tallied by the third quarter as Rock Health notes) was driven by “mega”-deals accelerated during the public health crisis of COVID-19. In the third quarter of 2020, some $4 billion was invested in U.S. based digital health start-ups adding up $9.4 billion in 2020….so far. This is $1.2 billion more than two
Pharma’s Future Relevance Depends on Empathy, Messaging, Partnering, and Supporting Patients and Providers
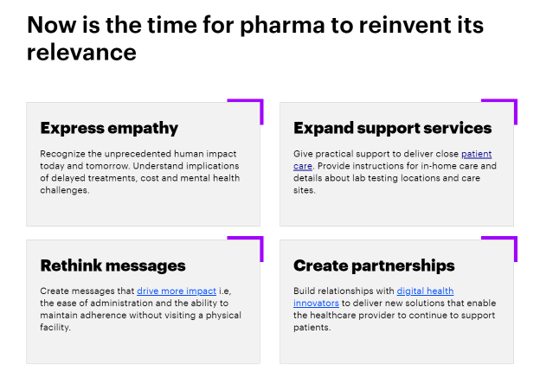
COVID-19 is re-shaping all industries, especially health care. And the pharma industry is challenged along with other health care sectors. In fact, the coronavirus crisis impacts on pharma are especially accelerated based on how the pandemic has affected health care providers, as seen through research from Accenture published in Reinventing Relevance: New Models for Pharma Engagement with Healthcare Providers in a COVID-19 World. For the study, Accenture surveyed 720 health care providers in general practice, oncology, immunology, and cardiology working in China, France, Japan, the United Kingdom, and the U.S., in May and June 2020. Top-line, Accenture points to four
My ABCovid-19 Journal – Day 3 of 5, Letters “K” through “O”
Welcome back to my ABCovid-19 Journal, which I created/curated in the early weeks of the coronavirus pandemic. This week, I’m sharing all the letters of the alphabet with you which reminded me keywords and themes emerging as we were learning about this dastardly public health threat beginning early in 2020. In today’s Health Populi blog I bring you letters “K” through “O,” continuing through the rest of the alphabet tomorrow and Friday while I’m on a lake-side holiday that’s good for mind, body, and spirit. K is for Kirkland, Washington state In the U.S., one of the earliest hotspots for





 Hackathons are intense, fast-paced events where interdisciplinary teams come together to solve complex problems. In this SEE YOU NOW Insight from
Hackathons are intense, fast-paced events where interdisciplinary teams come together to solve complex problems. In this SEE YOU NOW Insight from  I'm once again pretty gobsmackingly happy to have been named a judge for
I'm once again pretty gobsmackingly happy to have been named a judge for  Stay tuned to Health Populi in early January as I'll be attending Media Days and meeting with innovators in digital health, longevity, and the home-for-health during
Stay tuned to Health Populi in early January as I'll be attending Media Days and meeting with innovators in digital health, longevity, and the home-for-health during