The Healthcare Affordability Elections, 2026 and 2028 – Listening to the KFF Tracking Poll, January 2026
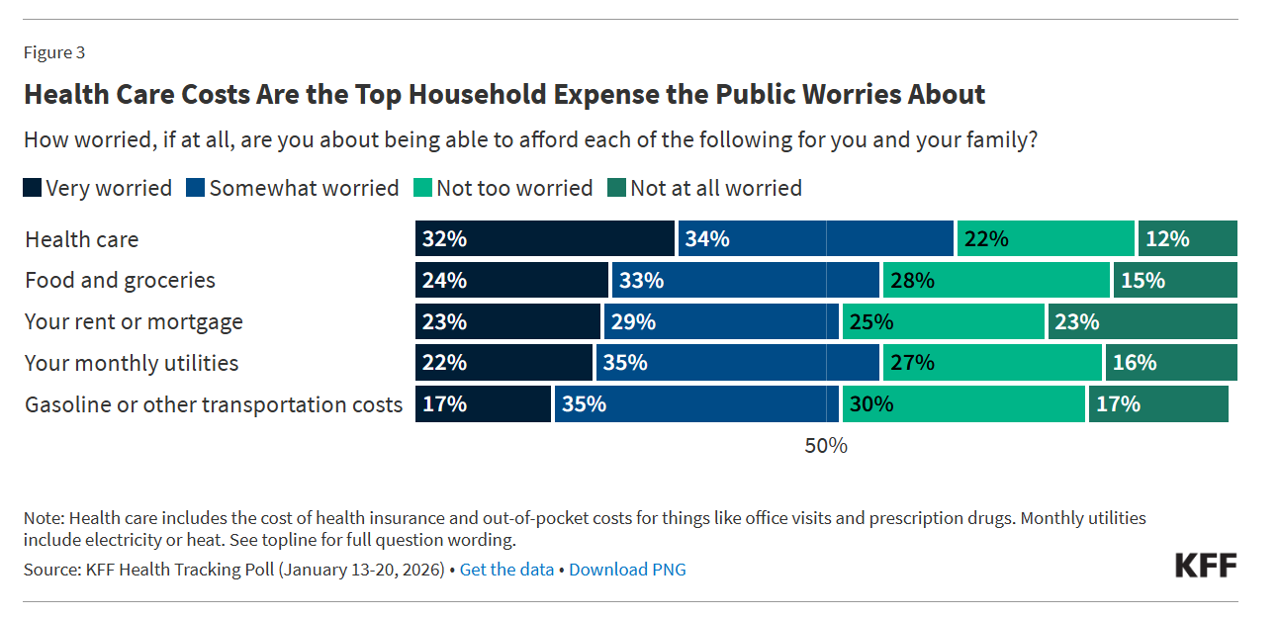
The title of KFF’s press release launching the Foundation’s January 2026 Health Tracking Poll clearly observes, “Health Care Costs Tops the Public’s Economic Worries as the Runup to the Midterms Begins.” I’ve pulled out the key details to share my lens on the 2026 midterm and 2028 Presidential election forecast, which I believe will turn out to be (in part) The Patients’ Elections. Here’s the top-line title finding — where most people in the U.S. — 2 in 3 people (66%) — are worried more about health care costs compared with other major household expenses.
Exercise is Health Care, and Consumers Are Willing to Pay – Context for #CES2026
“Americans are not just setting fitness goals; they are budgeting for them,” Liz Clark, President and CEO of the Health & Fitness Association observed. “People increasingly see exercise as an essential investment in their long-term health. Even in a challenging economic environment, Americans are prioritizing physical activity as a proactive form of preventive healthcare.” Americans see exercise as healthcare — and health — according to a survey from the Health & Fitness Association (HFA). HFA commissioned Kantar to conduct the online survey among 2,000 U.S. adults 18 and over in December 2025 — well-timed for the
Navigating a Constellation of Uncertainties: Health/Care in 2026 (My Un-Forecast)
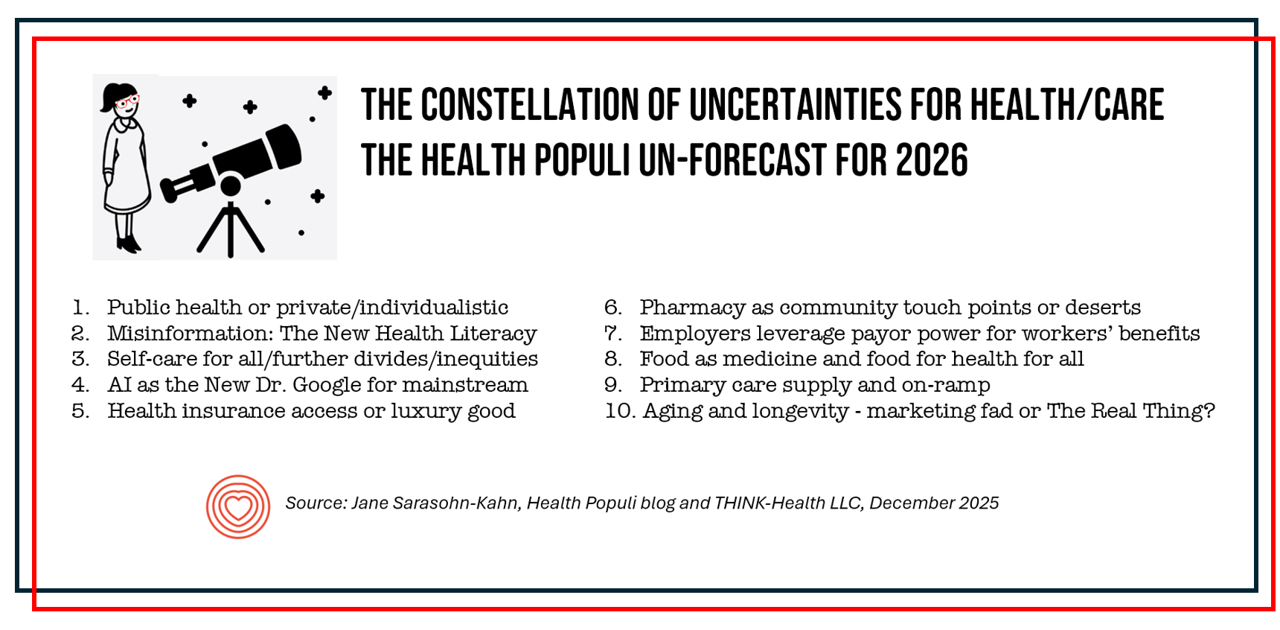
Almost from the first year of launching Health Populi in 2007, I’ve written a “TrendCast” for the coming year of health care. Over many years, there weren’t so many blogs devoted to health care which featured such prognostications, and so readers could divine signal from noise and move forward into new years with manageable lists of What To Expect Next Year in Healthcare. Here’s one from ten years ago that brings a sense of déjà vu: most of the findings are consistent with what we know for sure about 2026 and it’s useful to look back with today’s eyes to
The New Health Consumer Mindset and Wallet: From GLP-1s to Trading Up for Health & Longevity

From GLP-1s to longevity and new views on self-care for healthcare, the people are taking their health in-hand, at-home, and via-tech to complement and sometimes replace the legacy health system touchpoints which are the traditional categories for care: hospitals, doctors, rehab centers, diagnostics and labs, and health care financing and plans — some opting out of plans and going full-risk (cash, out-of-pocket) truly self-insuring against future medical risks. As I prepare to publish my Year-End/New Year TrendCast for 2026, I felt like front-ending next week’s annual long post with details on the demand side of the forecast — a focus
Men’s Fertility Feelings – The Influence of Trust and Social Media (My Progyny Post #3)

Trust is a key enabler for people’s health engagement. As the American Medical Colleges’ Center for Health Justice defines it, trustworthiness is “rooted in honesty and honors lived experience….. key to a successful patient-provider partnership.” In his book, Notes On Being A Man, Scott Galloway calls out that men’s fertility issues are formed as part of a larger societal context and crisis point, exacerbated by economic pressures and lack of opportunities for male bonding and in-person social touchpoints. In the second post in this series of three, we discussed those economic pressures Galloway notes, and the financial stressors that shape
The Home Economics of Family and Fertility: Men’s Financial Views on Their Fertility Journeys (My Progyny Post #2)
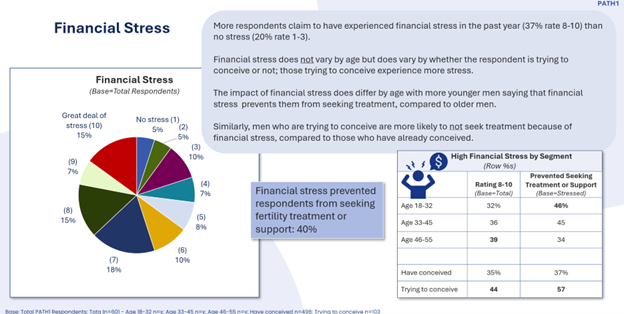
Cost is a leading reason why people say they could not obtain the fertility care they need. But the costs of IVF and other forms of fertility care lie within a larger home economics framework of family-building and -raising. The context and costs of raising a child in America. Consider the layers of a household budget starting with the home’s “macro”-economics of income. Then within that circle, especially in the U.S., the factor of whether that household is covered by employer-sponsored health insurance. The next layer of more health micro-economics in the family is the
Feeling Under-Served and Overlooked: Men’s Views on Their Fertility Journeys (My Progyny Post #1)
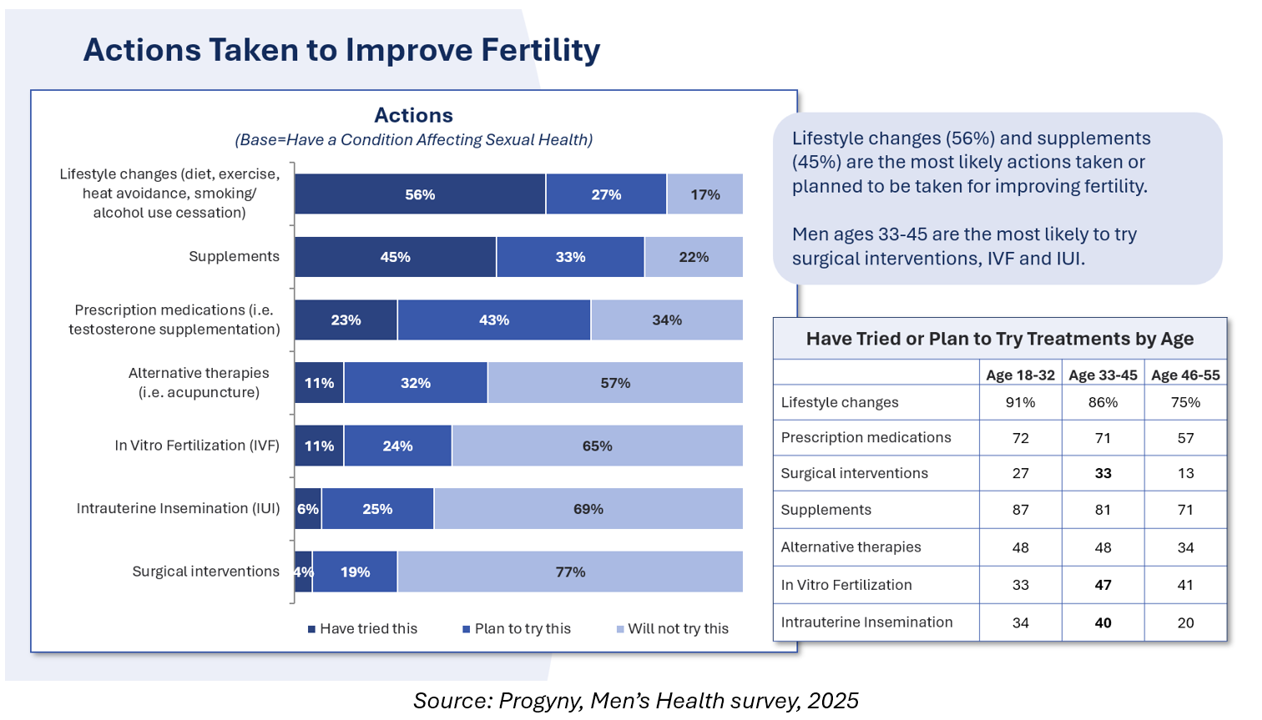
In his latest book, Notes on Being a Man, Scott Galloway discusses his personal fertility journey in the larger social context of what it means to be a man in modern America. Galloway’s infertility challenges shared with his wife inform his views on men’s health across all dimensions — physical, mental health, social health, financial well-being — and how, of course, men’s overall health is also a women’s and children’s issue. Men can feel “left out” of infertility discussions, based on results from the first and largest multi-national study into men’s feelings about their infertility revealed. “How men feel about
Most MAGA Supporters Support Extending the Expiring ACA Tax Credits – Will That Move Negotiations to Re-Open the Government?
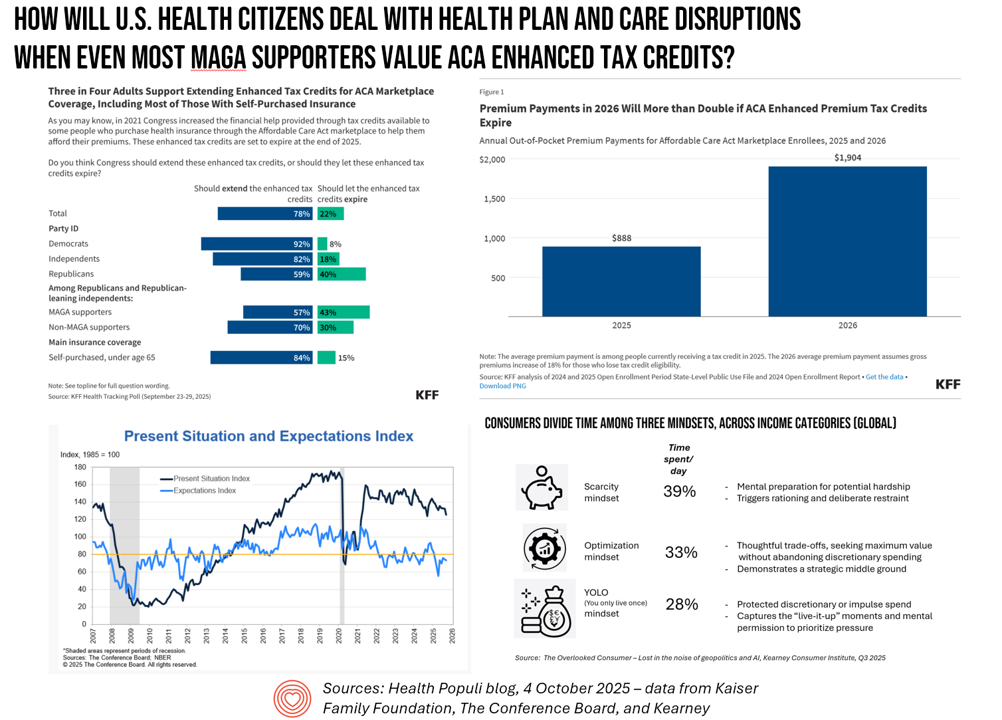
A couple of days into the U.S. Federal government shutdown, there’s one message the Congressional Democrats are tending to voice: that is that health care is on the line, and that’s the issue on which they’re betting will bring negotiators back to Capitol Hill — expecting a few Republicans to join in that dialogue. Most U.S. adults across political parties would want to see Congress extend the enhanced Affordable Care Act tax credits that are set to expire next year we see in a poll from the Kaiser Family Foundation published October 3. And that includes most Republicans and MAGA
The Emotional Drivers of Healthcare Discontent – Press Ganey Points to Access and Affordability Worries Driving Anxiety and Anger
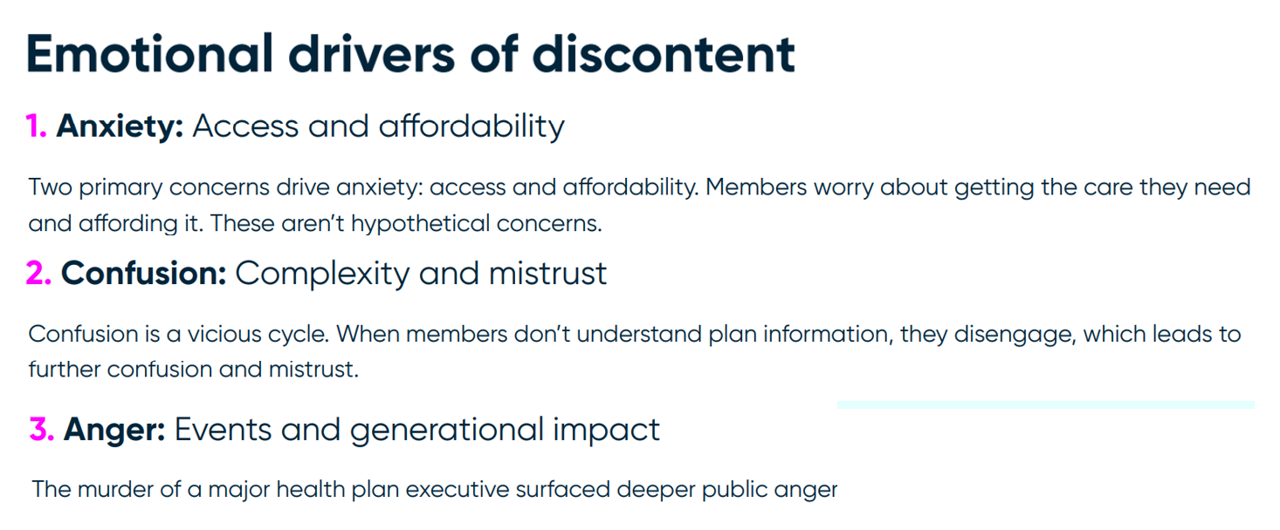
In the current era of U.S. health citizen grievance with the health care system, people feel anxious, confused, and angry — especially when it comes to access and affordability of health care. We learn more about these emotional drivers of health/care grievance in Understanding Health Plan Member Discontent, an assessment of health consumers’ views of satisfaction across health insurance plan types (commercial, Medicaid, Medicare, and marketplace plans) and age of member, from the health consumer experience team at Press Ganey. Those three underlying factors driving discontent translate to different generations differently. Overall, anxiety relates to
In 10 Years, Health Care Will Happen Where Life Happens – PwC’s Tea Leaves into 2035
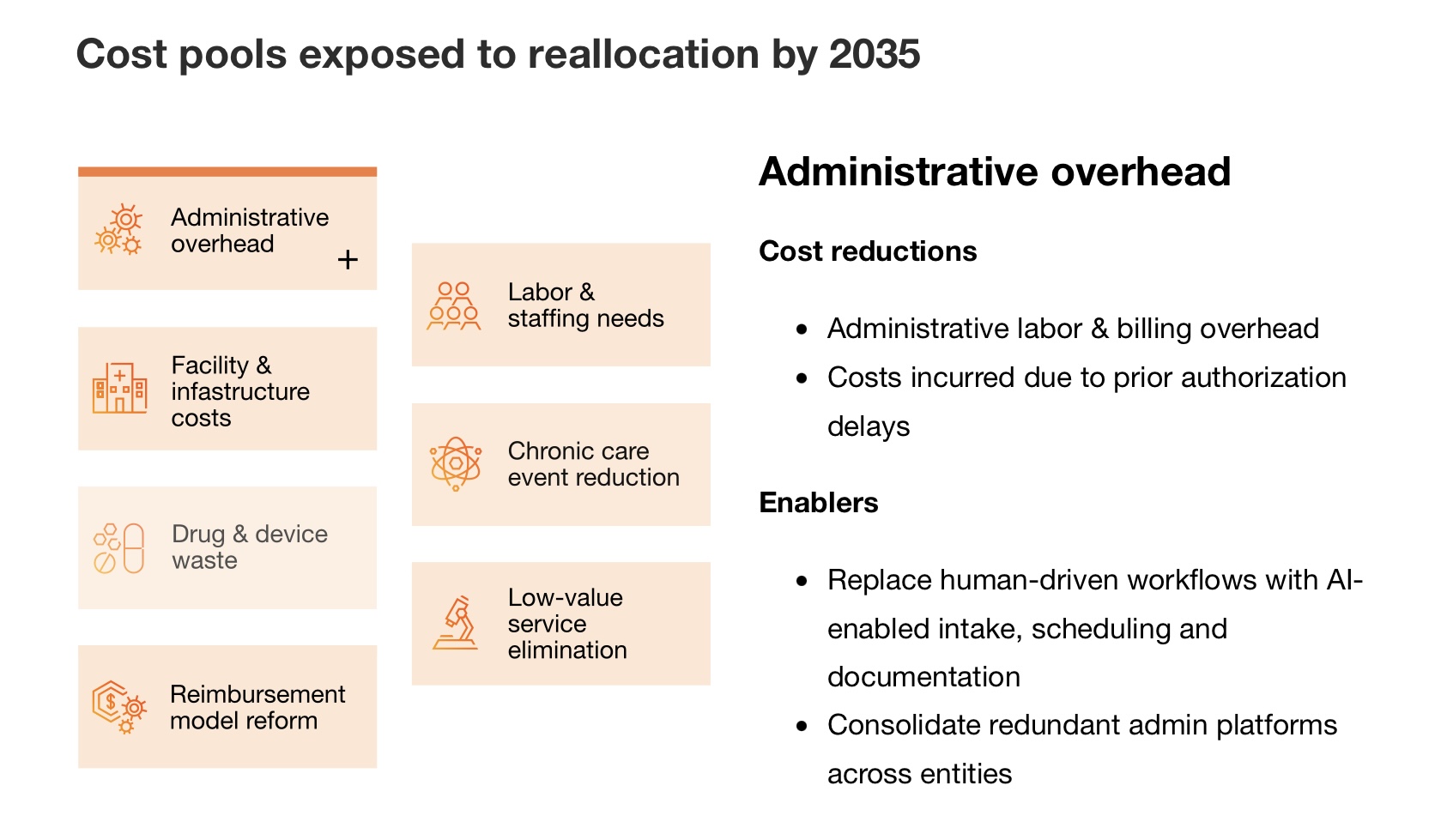
The costs of medical care are breaking the system, PwC asserts at the start of its new report on the $1 trillion opportunity to reinvent healthcare. The past 3 years of 8+% U.S. national health expenditure increases are “untenable,” PwC says, with 90% of that spending going toward patients with chronic and mental health conditions. What will transform the system and move us from “breaking point to breakthrough?” Biology and technology, PwC explains, with technology moving exponentially and simplifying care at scale, and biology decoding the “human operating system” enabling precision at scale. This
Dr. Osterholm Explains “The Big One” – A Deja Vu Moment with a True North Public Health Expert
“The truism that no one is completely safe until everyone is safe is a truism because it happens to be true.” So caution Michael Osterholm, epidemiologist, professor at the University of Minnesota School of Public Health, and director of CIDRAP (the Center for Infectious Disease Research and Policy at the U-MN) and collaborating writer Mark Olshaker in their new book, The Big One. (In this post, for the sake of brevity, I’ll refer to the two authors as “O&O”). Simply put, the tagline tells us what we are about to read: a
Expect Double-Digit Prescription Drug Trend Increases in 2026 – The Update from HUB International
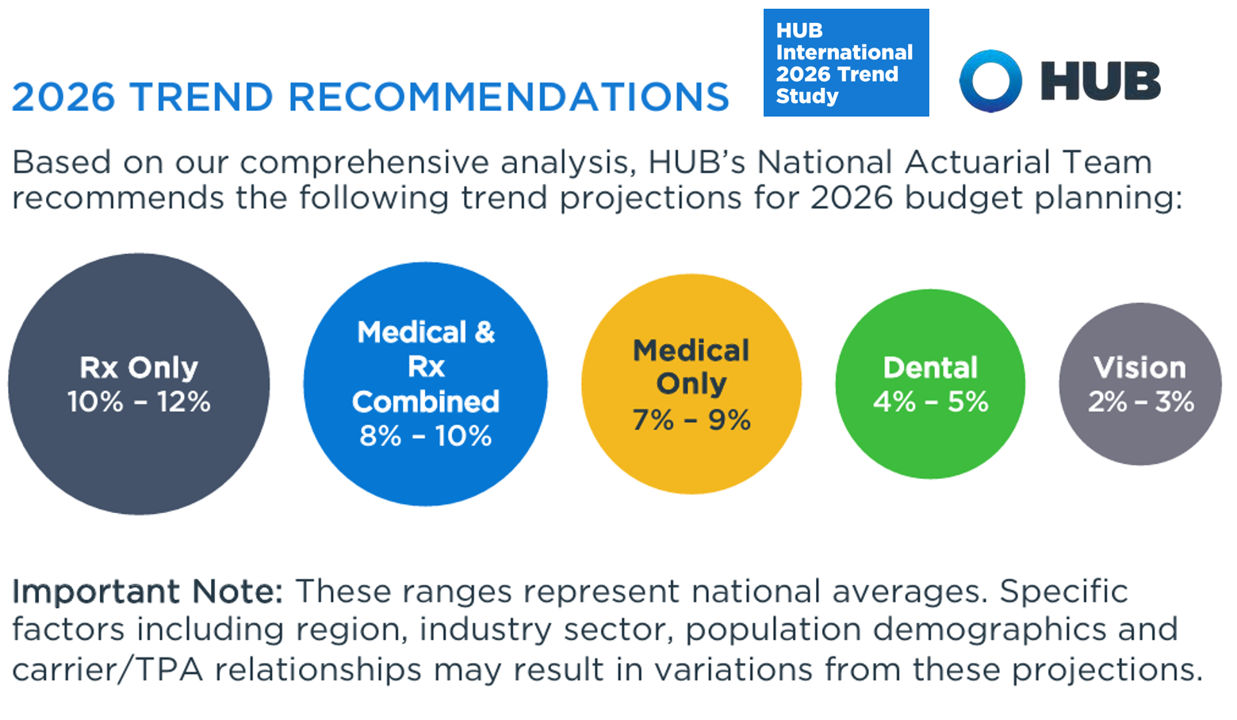
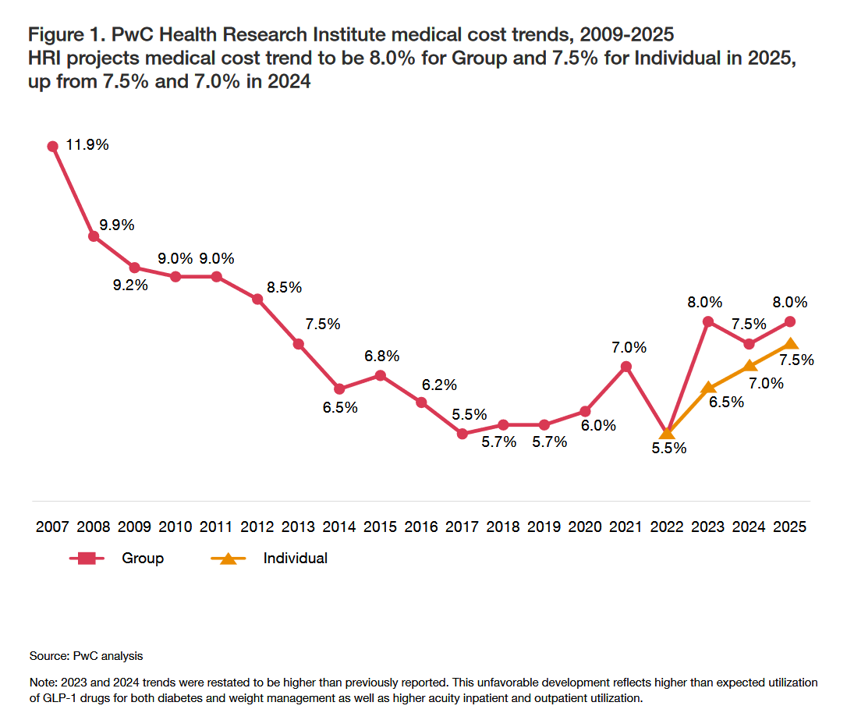
Prescription drug price trend for 2026 will be between 10% and 12% according to the 2026 Trend Study from HUB International, a global insurance and financial services firm. Here’s HUB’s line chart of the combined medical and Rx trend, illustrating nearly double trend growth since 2022 following the peak of 10.1% (combined) in 201 as patients returned to health care services and encounters when feeling safe in the fading out of the COVID-19 pandemic. That precipitous low-point in 2022 of 3.4% was the peak of the coronavirus stay-at-home period, representing the “medical distancing” felt across
On Labor Day 2025: From Health Care “Revenue Bounty Hunters,” Medical Bills Back into FICO Scores, the Rise of “Cute Debt,” and Tariffs — U.S. Consumers’ Face Eroding Financial Health
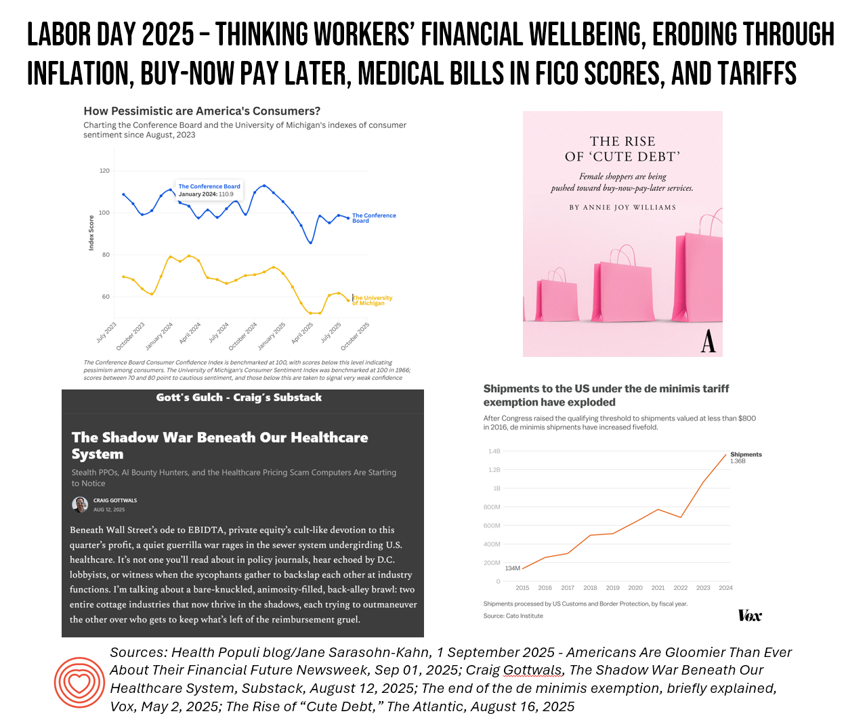
On this U.S. Labor Day 2025, the physical and the fiscal, with the mental, converge as I ponder what working Americans are facing….packing kids up for school, sorting out college payments and loans, dealing with rising costs of daily living, and feeling a growing pinch of what President Trump’s tariffs have had in store now that they’re hitting SKUs around the household. This post will cover most days this week as my own workflows will be heavy as clients return to face returns-to-work and updating scenario plans. We start this post with a headline: “Why Hospitals Are Hiring ‘Revenue Bounty
U.S. Physicians Have to Deal with the Growing Info-Demic of Disinformation Meant to Mislead Patients
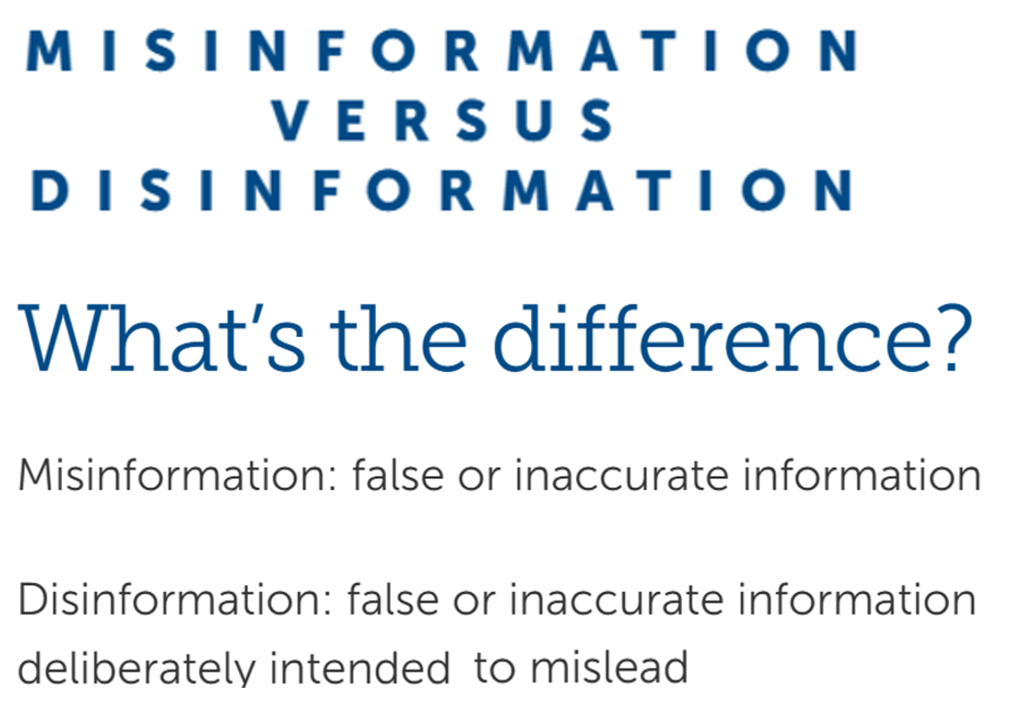
Close to 100% of U.S. doctors agree that misinformation and/or disinformation undermines patient care, according to a new survey from the Physicians Foundation. The Foundation polled over 1,000 U.S. physicians in late May 2025 to gauge doctors’ perspectives on information and patients’ health literacy. Furthermore, over one-half of physicians believe that misinformation – and/or disinformation — significantly impacts the ability to deliver quality patient care. The first graphic differentiates between “misinformation” and “disinformation,” where the latter is false or inaccurate information deliberately intended to mislead people. Misinformation is somewhat more benign in
Prescription Drug Pricing in America – a 3-Part Update, From the Over- the-Counter OPill and “Half-Price” Ozempic to Most-Favored-Nation Rx (Part 3)
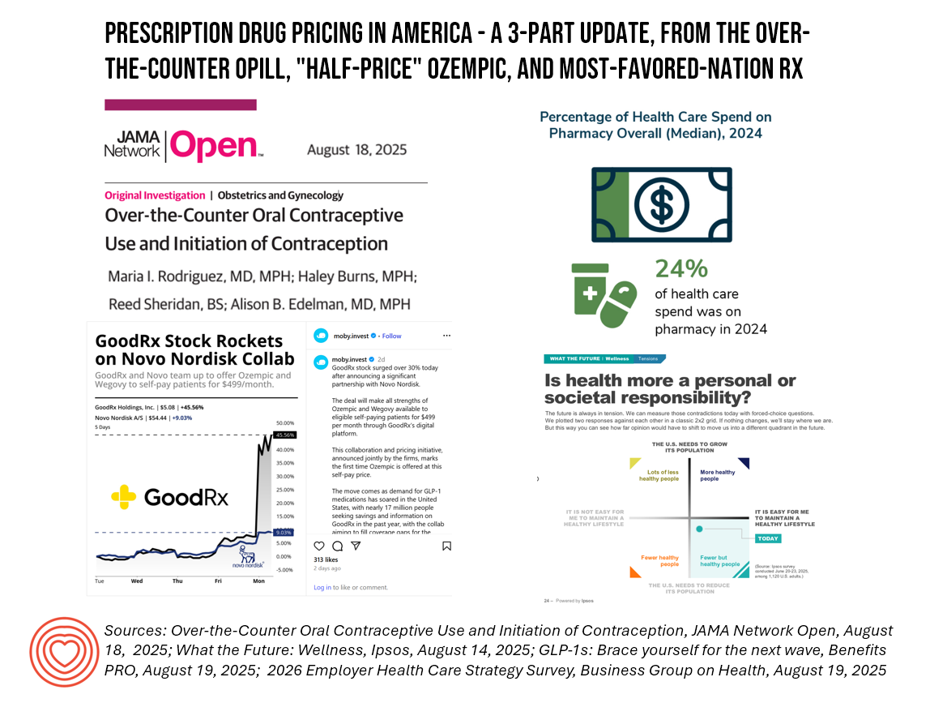
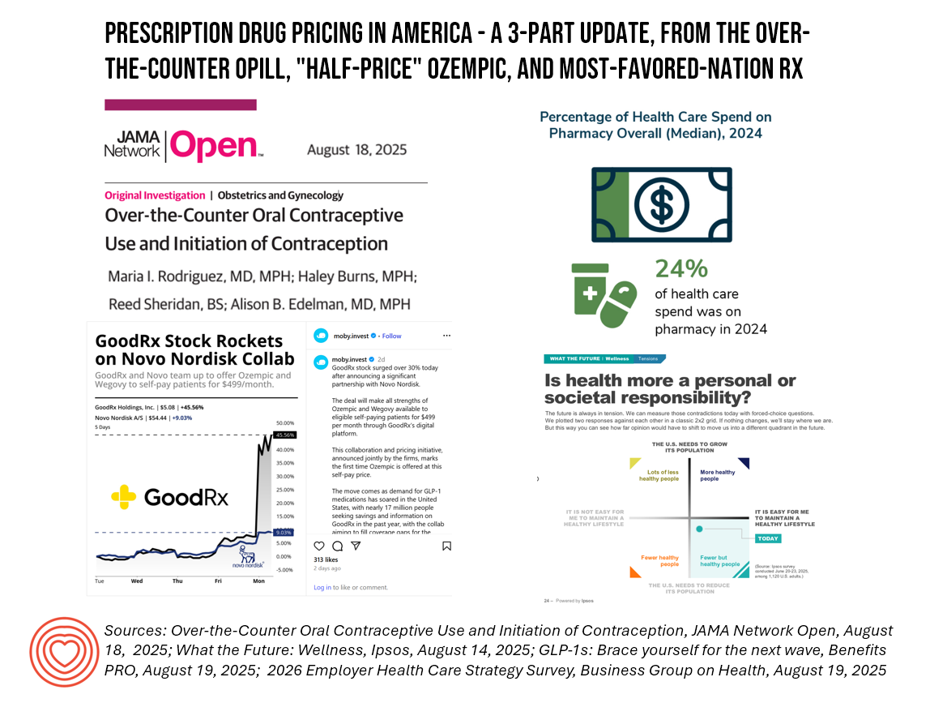
Welcome to Part 2 of 3 in my consideration of Prescription Drug Pricing in America. You can catch up with yesterday’s Part 1 post here, and Part 2 here. The macro-context for these 3 posts are the forecasts for health care spending for the coming year. Health care cost increases forecasted for 2026 will, in significant part, be driven by prescription drug trend. This graphic from this week’s release of the Business Group on Health’s employer survey on healthcare cost growth to 2026 illustrates a key finding that’s echoed in other similar studies recently released and covered here in Health Populi.
Prescription Drug Pricing in America – a 3-Part Update, From the Over- the-Counter OPill and “Half-Price” Ozempic to Most-Favored-Nation Rx (Part 2)
“Big Pharma has a new vision for selling drugs. It’s going to the mattresses,” writes Josh Nathan-Kazis in MSN earlier this week. That is, going direct-to-consumer (DTC) the way the mattress industry has done in the past decade, cutting out brick-and-mortar sleep shops at retail. In the case of “Make(ing” like a mattress company,” Josh explains, the pharma manufacturers “sell shots and pills straight to the consumer.” In this case, that’s cutting out the pharmacy benefits managers and other intermediaries that have taken dollars in the transactions of drug benefit claims which have added costs to payers (health plan sponsors
Prescription Drug Pricing in America – a 3-Part Update, From the Over- the-Counter OPill and “Half-Price” Ozempic to Most-Favored-Nation Rx (Part 1)
Health care costs will increase, overall, as much as 10% in 2026, the consensus of several health benefit analysts inform us. And, “workers to bear brunt of health cost increases in 2026,” reads today’s Axios headline on the topic, weaving together several studies from the Business Group on Health, Mercer, and the International Foundation of Employee Benefit Plans. A kay cost-contributor cited in all of these health cost forecasts is the prescription drug line item: specialty drug prices, and specifically the costs of GLP-1 medicines and cancer therapies. One strategy gaining fast-traction on both the
Women Walk a Financial Tightrope: What That Means for Women’s Health, Mind, Body, & Wallet
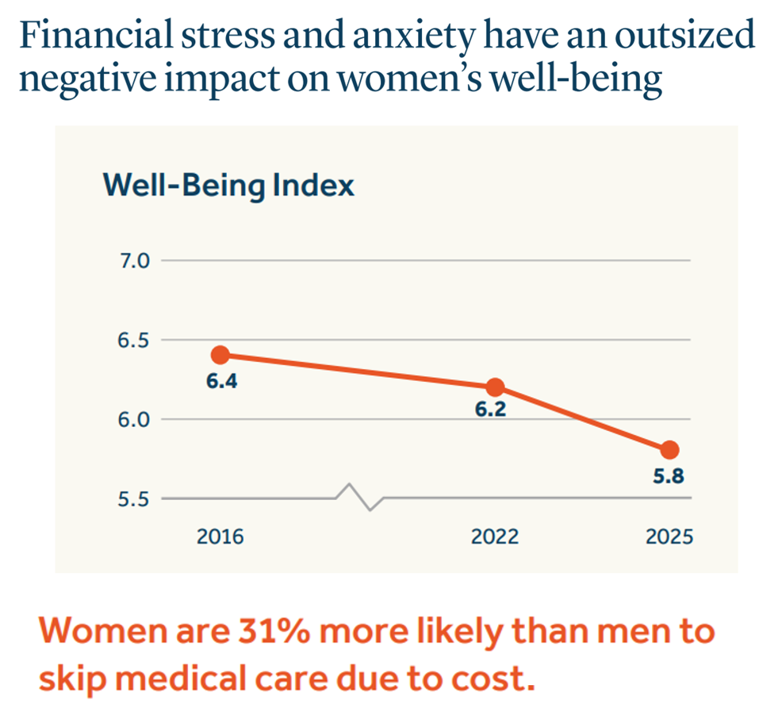
Financial stress and anxiety have an ‘outsized’ negative impact on the well-being of women in America, compared to male counterparts, we learn in Health. Wealth, and Happiness – Helping to overcome roadblocks to women’s well-being, a report from the Guardian Life Insurance Company. This report is part of Guardian’s annual research program called Mind, Body, Wallet, which the company launched 14 years ago. The goal of Mind, Body. Wallet is to assess how health citizens define “well-being” in daily living, making the crucial connections between mental health (“Mind”), physical health (“Body”), and money
Why a Grocery Store Signed On to “Make Health Tech Great Again”

Joining the ranks of technology heavyweights Amazon, Anthropic, Apple, Google, and OpenAI, as well as digital health innovators Noom, Oura, Virta Health and Welldoc, who have pledged to “Make Health Tech Great Again,” Albertsons, one of the largest grocery chains in the U.S., put its name on the list with these and other early adopter collaborators. The Albertsons’ company blog published on 31 July discussed the background and rationale for this decision. “Specifically, we pledge to explore how our Sincerely Health platform can connect to The Centers for Medicare and Medicaid Services (CMS) Aligned
The Patient as Consumer – Updates from Fidelity on Retiree Health Care Costs ($172,500), Delaying Care, Tariff Impacts on Spending, and Roche Going DTPatient for Rx’s?

As of August 2025, U.S. patients of all demographics and geographies face many uncertainties with respect to their care. Issues such as health plan coverage, prescription drug costs, and access to services, among other challenges, continue to re-shape patients-as-health-consumers seeking transparency, clinical choices, and trust-worthy relationships with touchpoints in their personal health ecosystems. Four just-breaking stories across the health/care ecosystem illustrate several of these uncertainties and forces in U.S. health care — some adding friction and angst in a patient’s life, others perhaps providing some relief for certain health consumers. These news items address health care costs in retirement, the
Medicare at 60: Prior Authorizations Are a Problem for People in the U.S., Regardless of One’s Political Party, Income, or Insurance Type
Happy 60th Anniversary Medicare, today marking six decades since the passage of this law which was a landmark milestone for The Great Society, U.S. style. Since its inception and implementation, Medicare quite often leads in adoption of new medicines, new processes, new technologies in health care. But as I track the phenomenon of health citizenship in the U.S., I observe growing consensus among American patients — cross health plan type — increasingly impatient for health care access. We can now add Americans’ growing dissatisfaction with the prior authorization process, an opinion that now spans majorities of consumers regardless of their
How Taking Care of Our Pets Could Inspire Us to Care Better for Ourselves (and Each Other)

In a recent study which was part of the American Heart Association’s Healthy Bond for Life initiative, two-thirds of Americans told the AHA that they took better care of their pets than themselves. So with a lens on how to help inspire peoples’ self-care, I was keen to dive into research from Pet Partners Insurance (PPI), a pet health insurance provider, collaborating with the Human Animal Bond Research Institute (HABRI), to learn more about The Power of Pet Perks: How Pet-Inclusive Benefits Drive Employee Engagement, Retention, and Positive Workplace Culture. My interest
U.S. Workers Who Get Health Insurance From Work Can Expect Greater Cost-Sharing and New Networks in 2026

At least one-half of employers will likely raise employee cost-sharing amounts in 2026, according to the Survey on health & benefit strategies for 2026 from Mercer. Mercer surveyed 711 organizations for this study, fielded in April 2025, to assess employers’ views on and strategies for health benefits in 2026. There are three challenging pillars underlying employers’ 2026 approaches to workers’ benefits: How to disrupt cost growth with what Mercer coins as “bolder” strategies How to consider and address all dimensions of affordability, and, How to design and implement inclusive benefits that build workforce
National Health Spending in the U.S. in 2033: What 20.3% of the GDP Will Be Spent On
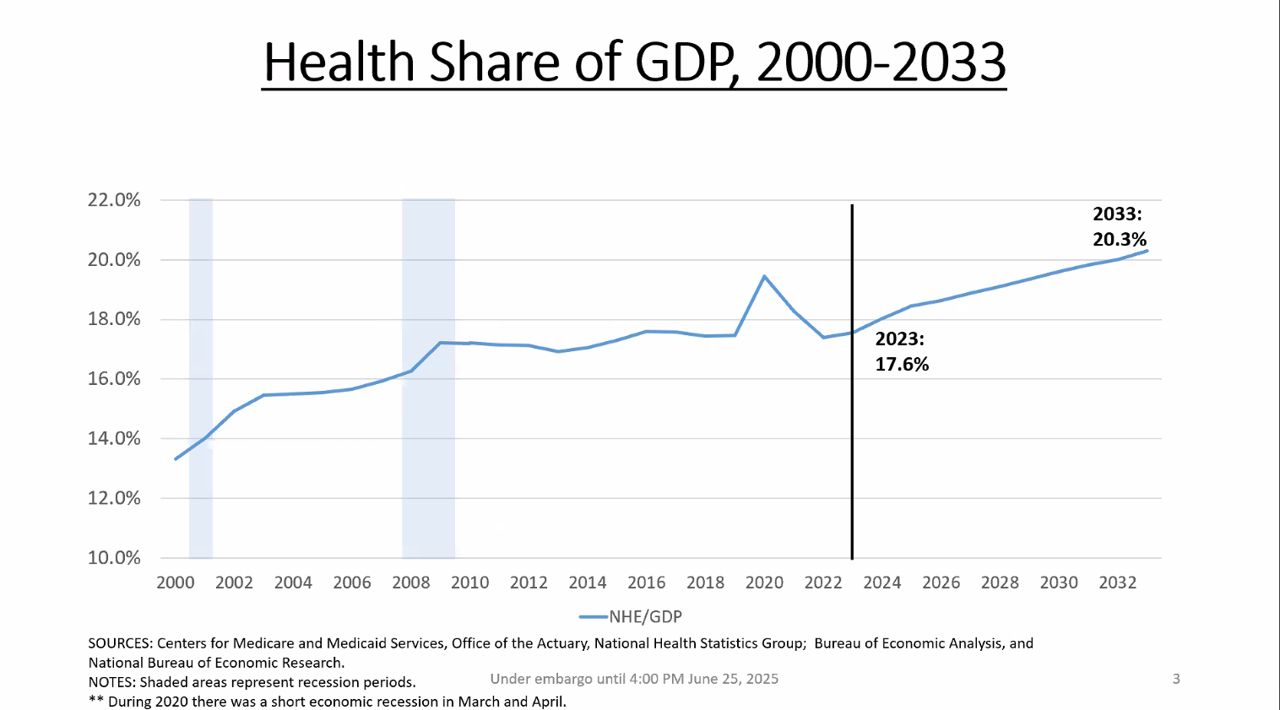
By 2033, national health spending will comprise 20.3% of the U.S. GDP, based on the latest national health expenditure projections developed by researchers from the Centers for Medicare and Medicaid Services (CMS). This growth will be happening as CMS projects coverage of insured people to decline over the period. Earlier today, I attended a media briefing hosted by Health Affairs to receive the CMS team’s top-line forecast of NHE from 2024 to 2033 discussing these findings. Fuller details on the projections will be released in the July issue of Health Affairs on 7
That Big Beautiful Bill’s Healthcare Proposals Aren’t So Pretty in the Views of Most People in the U.S. – Including Josh Hawley (R-Mo.) – Listening to the Kaiser Family Foundation June Health Tracking Poll

Across all U.S. voters, the so-called “Big Beautiful Bill” Act (BBB) is seen unfavorably by nearly a 2:1 margin. Underneath that top-line, Democrats, Independents, and non-MAGA Republicans oppose it, while MAGA supporters favor it. But favorability erodes when people hear about possible health impacts, we learn in the June 2025 Health Tracking Poll from the Kaiser Family Foundation. The details on views of the BBB Act are shown in the first bar chart, with overwhelming disfavor among Democrats and Independents, and majority unfavorability among non-MAGA GOP supporters. Next check into partisans’ lenses
What GoFundMe and Crowdfunding Campaigns Tell Us About Healthcare in America

“Can people afford to pay for health care?” a report from the World Health Organization asked and answered, with a focus on European health citizens. The same question underpins a new research paper published in Health Affairs Scholar, Insights from crowdfunding campaigns for medical hardship, Here, crowdfunding is a proxy for “can’t afford to pay for health care” in America. Here in blazing colors we have a snapshot of the study’s data in the form of a “heatmap.” FYI, a heatmap is a data visualization format that represents the magnitude of values of a dataset as a color — generally
The Spirit for Eating Healthier Is Willing, But the Cost of Doing So “Outweighs” the Will – Listening to Escoffier

It’s been a full week’s coverage on food-as-medicine and food as a driver of health in America this week on the Health Populi blog. Today we turn to the chefs at Escoffier who know food, teach food, and now offer programs in holistic nutrition and wellness through the lens of culinary arts. With that lens, Escoffier recently published a report on the future of healthy eating, which will round out this week’s Health Populi landscape on food and health. In the paper, the Escoffier team curated data points from many studies — via Gallup, Mintel, Innova,
Consumers Are Keen to Invest in Health and Well-Being – But Show Them the Evidence

Consumers around the world feel more invested than ever in what makes people feel both well and prosperous, we learn in the NielsenIQ Global State of Health & Wellness 2025 survey report. But there’s a trust deficit that must be healed in order for a health consumer to invest in services and products that feed health and well-being. NIQ fielded the survey research online in January and February 2025 among nearly 19,000 adults living in 19 countries: Brazil, Canada, China, the Czech Republic, France, Germany, Hungary, India, Indonesia Italy, Mexico, Netherlands, Poland, South Africa, Spain, Turkiye, UAE, United Kingdom, and
A Toyota RAV4 Hybrid, a Playground Set, or Healthcare for a Family of 4: What $35,119 Can Buy in 2025 According to Milliman
If you went shopping for something that cost $35,119 in 2025, which would you most value? A new 2025 Toyota RAV4 Hybrid with some extras on board? A Canyon BYO playground set for your yard, school, or social-athletic club? Or, Healthcare coverage for a family of 4 in the form of a PPO? Welcome to this year’s 20th anniversary edition of the Milliman Medical Index (MMI), which I’ve looked forward to reviewing for most of its two-decade history. [You can read my annual takes on the MMI here in Health Populi by searching “MMI” and the year of publication in
The Next Version of Medical Tourism: Medical Immigration?

One in three Americans could imagine leaving America for good as expatriates — with access to affordable and reliable health insurance the top consideration, according to research conducted by the Harris Poll on behalf of GeoBlue and International Citizens Insurance (ICI). “Thirty-one percent of potential expats cite concerns about healthcare coverage abroad being the reason they haven’t yet taken the leap to move abroad. This trumped concerns about their work and social life abroad,” the survey found. Earlier this year, The Harris Poll’s American Expats Survey, published in February 2025, found that health care accessibility
Health, Wealth, and How Business Can Support Consumers in an Era of “Uncertainty on Steroids”

Facing uncertainties across everyday life flows, U.S. consumers look to economic and health security — and welcome businesses to support these, we learn in an analysis from The Conference Board. The Conference Board (TCB) polled 3,000 U.S. consumers gauging their perspectives on uncertainties emerging out of the new Trump administration’s policy changes introduced in the first quarter of 2025. The chart details people’s financial/fiscal responses in blue, and the health (mental, social, and physical aspects) in yellow: Consumers’ fiscal strategies for coping with uncertainty are to seek out more affordable brands and retailers, adjusting
Health Insurance Coverage Among Smaller U.S. Businesses Is Eroding: A Signal From JPMorganChase
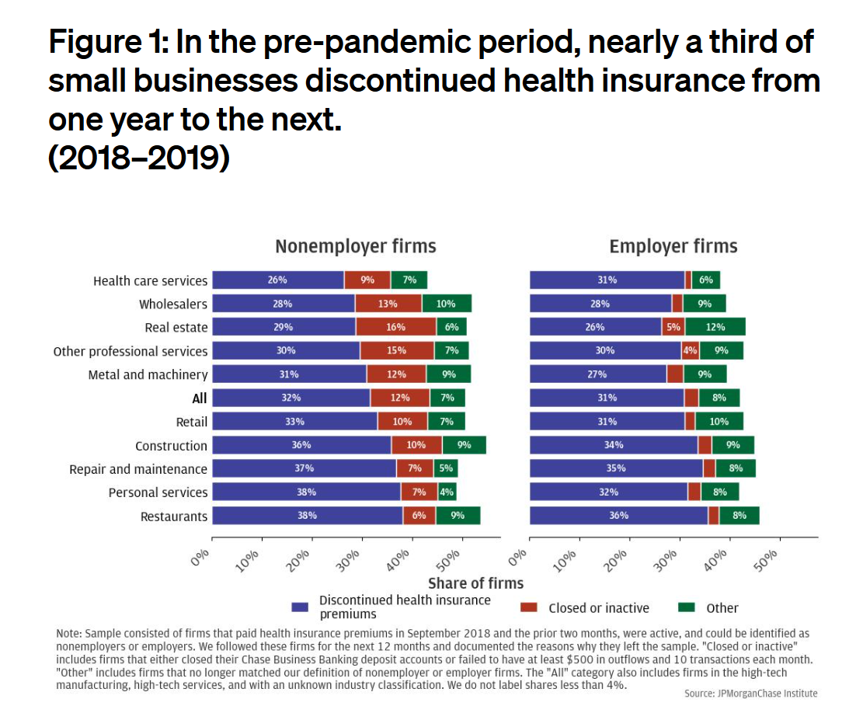
Working-age people in the U.S. depend on their employers to provide health insurance; just over one-half of people in America receive employer-sponsored health insurance. But a concerning signal has emerged that calls into question how sustainable the uniquely American employer-sponsored health plan model is: that is that one in 3 small businesses in the U.S. stopped covering health insurance after the worst of the pandemic health effects in 2023 as the companies payroll expenses continued to increase, a statistic raised in The consistency of health insurance coverage in small business: industry challenges and insights, a report from the JPMorganChase Institute
U.S. Health Care in 2025 Requires Scenario Planning: The Uncertainties (AI!?) That Inspire DIY Healthcare

As Weight Watchers prepares to initiate bankruptcy proceedings, I file the news event under “thinking the unthinkable.” “Thinking about the unthinkable” is what Herman Kahn, a father of scenario planning, asked us to do when he pioneered the process. In this book, for Kahn, “the unthinkable” was thermonuclear war, and the year was 1962. The book was tag-lined as “must reading for an informed public” and in it, Kahn I’ve been drawn back to this book lately because of a more intense workflow using
Most Americans Don’t Want to Cut Medicaid (Including Republicans)
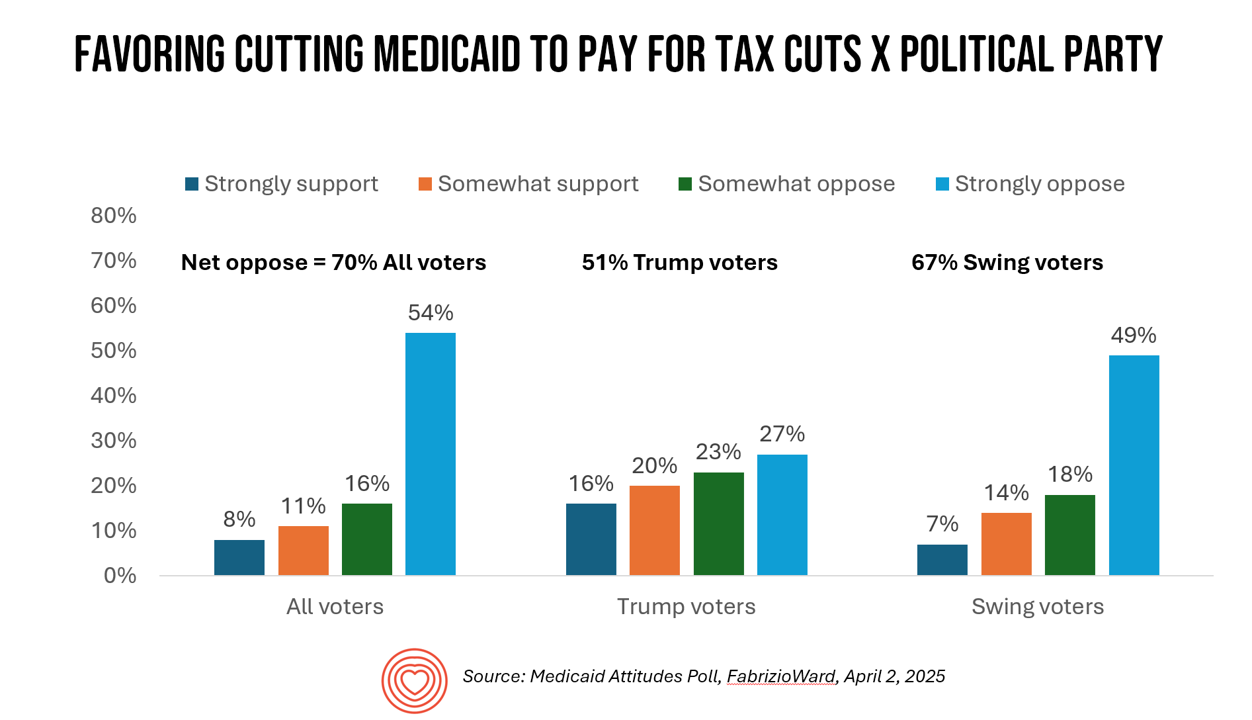
With potential down-sizing of Medicaid on the short-term U.S. political horizon, a fascinating poll found that most people identifying as Republican would not favor cuts to Medicaid. What fascinates me about this survey, published earlier this week, is that it was conducted by FabrizioWard, a polling firm that has often been used by President Trump. The firm’s Bob Ward told POLITICO that, “There’s really not a political appetite out there to go after Medicaid to pay for tax cuts. Medicaid has touched so many families that people have made up their minds about what
Are We Liberated Yet? Tariffs Can Impact Financial Health (Riffing on MoneyLion’s Health Is Wealth Report)
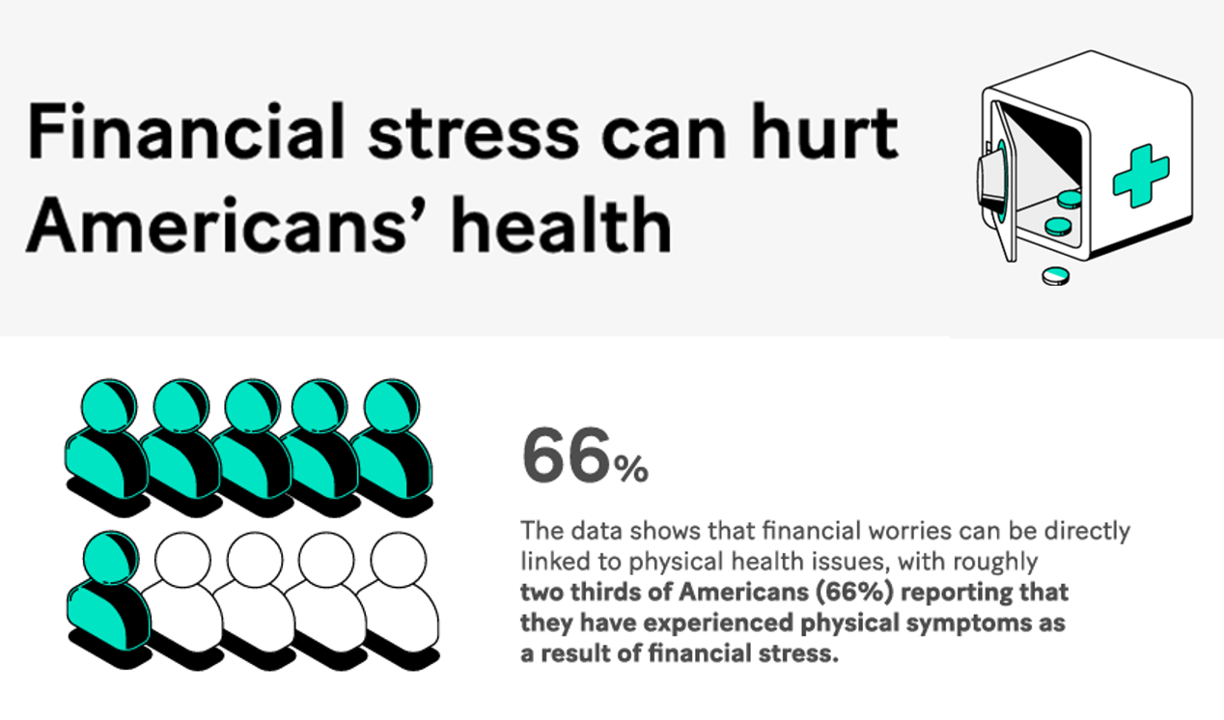
Americans’ financial health was already stressing consumers out leading up to Liberation Day, April 2nd, when President Trump announced tariffs on dozens of countries with whom the U.S. buys and sells goods. A new report from MoneyLion and Mastercard called Health is Wealth is well-timed for today’s Health Populi blog. The study was fielded by The Harris Poll online among 2,092 U.S. adults 18 and older between February 28 and March 4, 2025, so it was completed a month before the tariffs came to hit peoples’ 401(k) savings and employers’ company stock market caps.
How BioPharma Can Improve Consumers’ Experience and Health
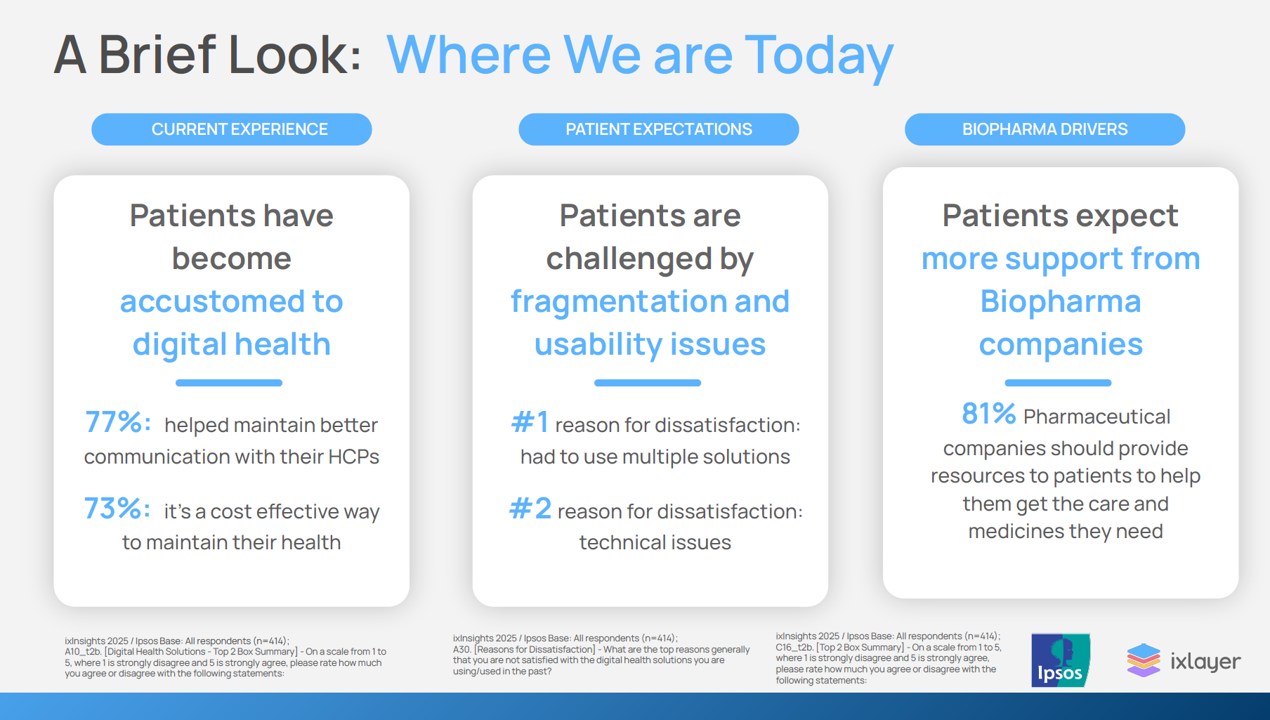
Patients as health consumers now know what “good” looks like in their digital experiences. People have tasted the convenience and respect they feel from well-designed, streamlined omnichannel retail experiences, and they now expect this from health care — specifically supported by the pharmaceutical companies who manufacture the medicines they use in managing chronic conditions, we learn in ixlayer ixInsights 2025: Pharma’s Role in Improving the Health Experience from ixlayer and Ipaos. The patient-focused report gets specific about people dealing with asthma, COPD, Type 2 diabetes, heart disease, psoriasis, and atopic dermatitis with a lens on
What is a Consumer Health Company? Riffing Off of Deloitte’s Report on CHCs/A 2Q2025 Look at Self-Care Futures
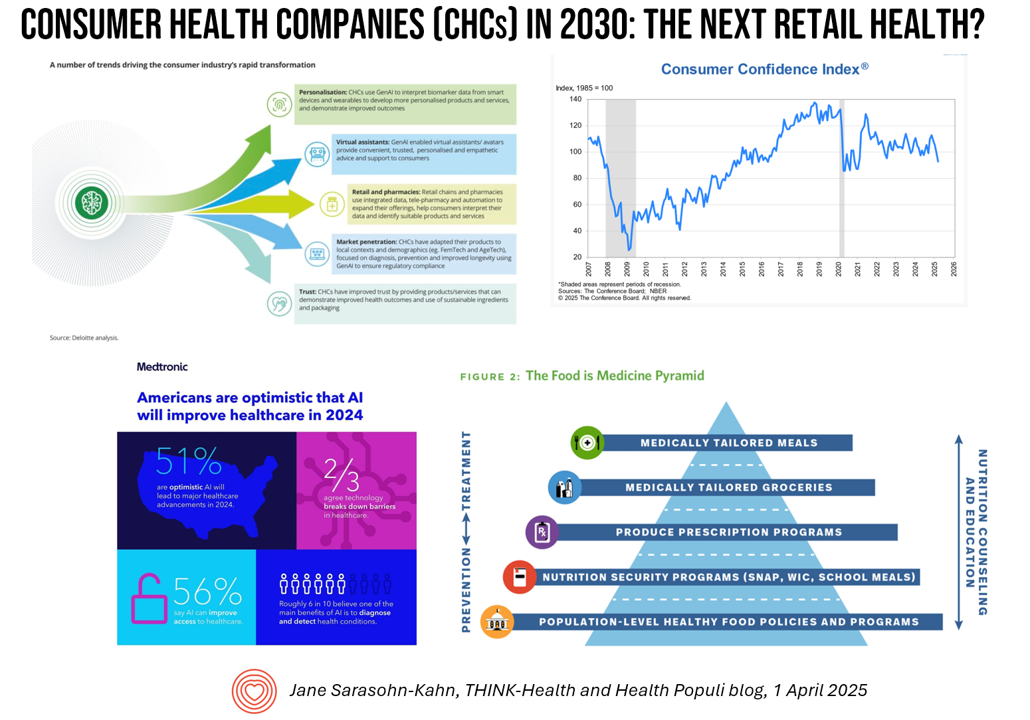
The health care landscape in 2030 will feature an expanded consumer health industry that will become, “an established branch of the health ecosystem focused on promoting health, preventing, disease, treating symptoms and extending healthy longevity,” according to a report published by Deloitte in September 2024, Accelerating the future: The rise of a dynamic consumer health market. While this report hit the virtual bookshelf about six months ago, I am revisiting it on this first day of the second quarter of 2025 because of its salience in this moment of uncertainties across our professional and personal lives — particularly related to
Health Care Nation – How to Inspire a Rosa Parks Moment for Healthcare in America?
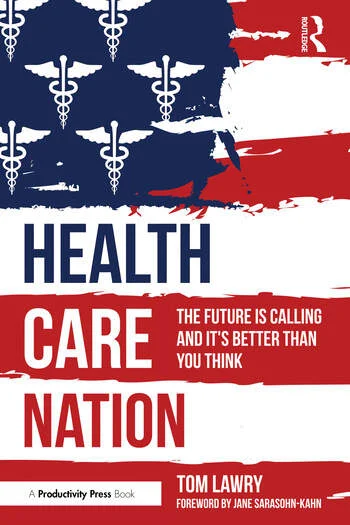
Tom Lawry may be best-known as a leading voice on AI in health care; after all, he’s written two very well-selling books on the topic, speaks all over the world on the subject, and in his most recent company-based gig helped lead Microsoft’s efforts in AI in health care and life sciences. When his publisher asked him to write a third book on AI in health care – still a hot topic in publishing – Tom said he’d rather turn to a subject long on his mind: the state of health care in America and how to change the conversation
From Bowling Alone to Eating Alone – What the Shift to Take-Out Food Means for Our Social Well-Being and Mental Health
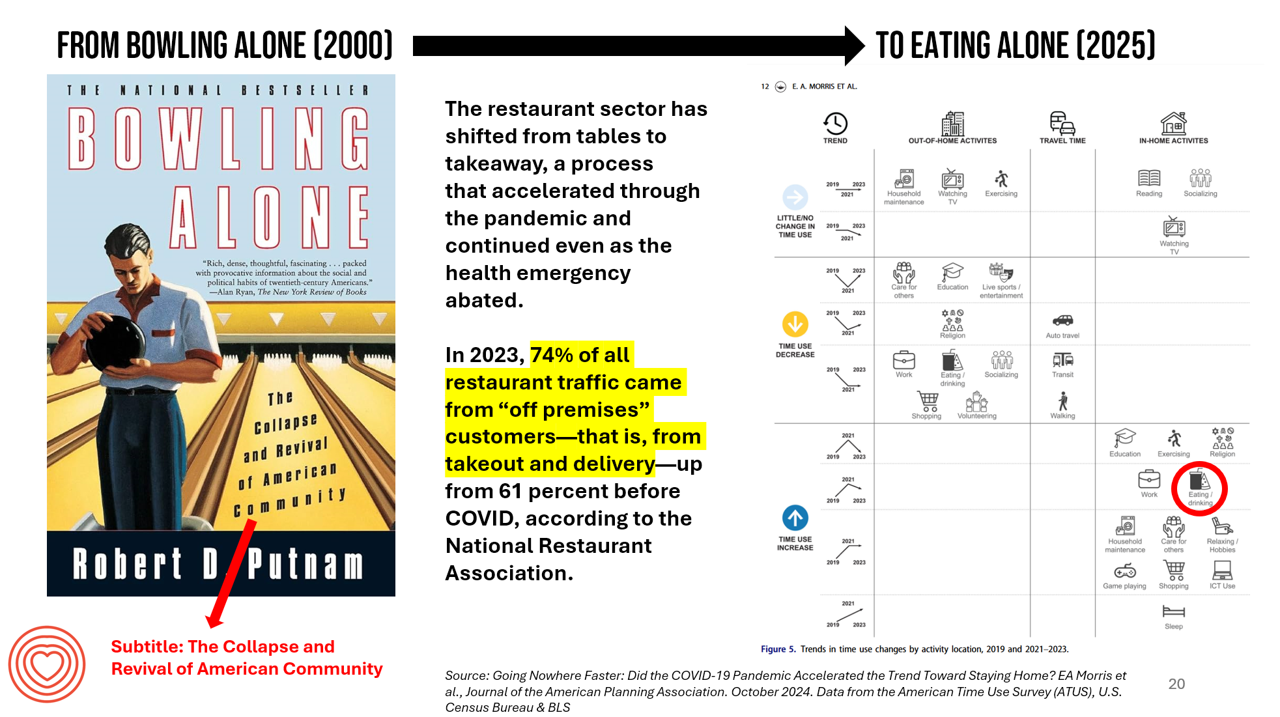
New data from the American Time Use Survey, research conducted by the U.S. Census Bureau and the Bureau of Labor Statistics, shows that Americans now favor eating in-home compared with eating out at restaurants. Corroborating this shift is other data from the National Restaurant Association sharing that 74% of all restaurant traffic in 2023 came from “off premises” customers — that is, from takeout and delivery — up from 61% in the pre-COVID era. What does this mean for our health, well-being, and sense of community and connectivity? I’m preparing a new talk to
The Growth of DIY Digital Health – What’s Behind the Zeitgeist of Self-Reliance?
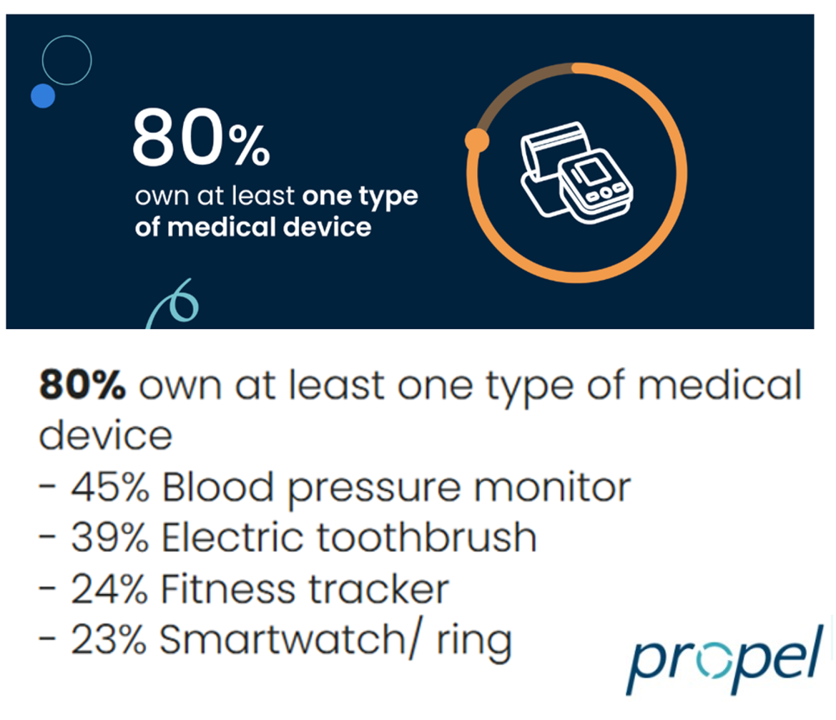
Most people in the U.S. use at least one medical device at home — likely a blood pressure monitor. used by nearly one-half of people based on a survey of 2,000 consumers conducted for Propel Software. The Propel study’s insights build on what we know is a growing ethos among health consumers seeking to take more control over their health care and the rising costs of medical bills and out-of-pocket expenses. That includes oral health and dental bills: 2 in 5 U.S. consumers use electric toothbrushes (a growing smart-device category at the
Consumers Are Financially Stressed – What This Means for Health/Care in 2025
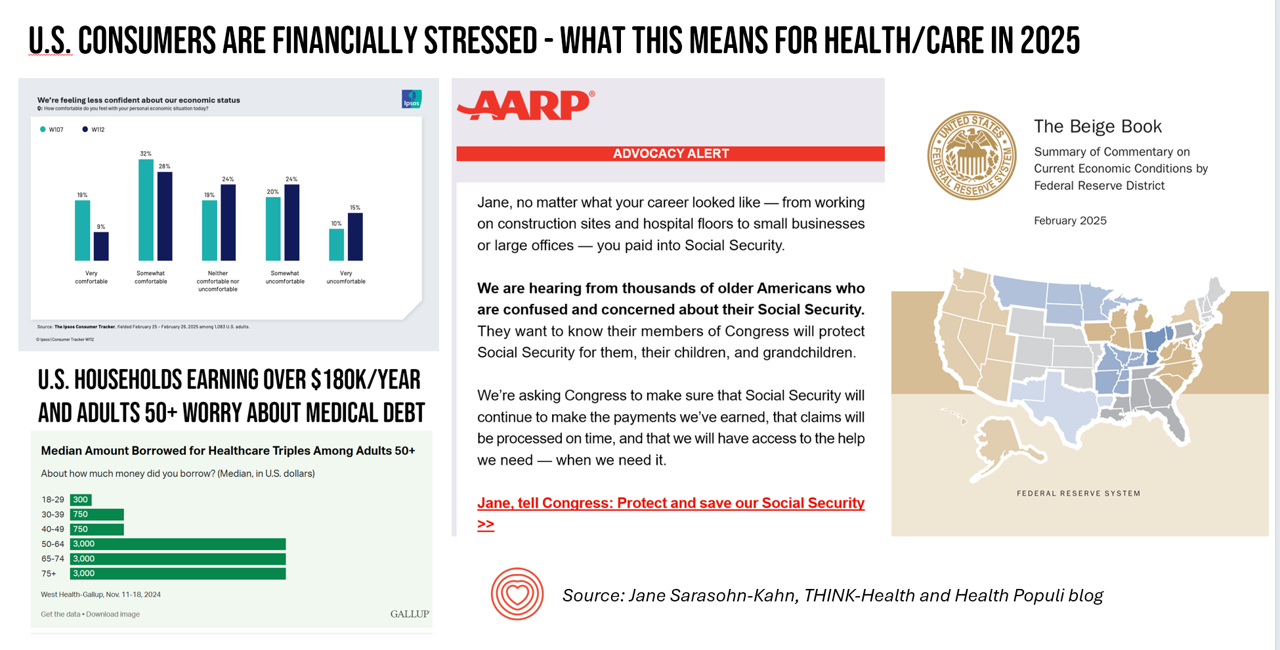
People define health across many life-flows: physical health, mental health, social health, appearance (“how I look impacts how I feel”) and, to be sure, financial well-being. In tracking this last health factor for U.S. consumers, several pollsters are painting a picture of financially-stressed Americans as President Trump tallies his first six weeks into the job. The top-line of the studies is that the percent of people in America feeling financially wobbly has increased since the fourth quarter of 2024. I’ll review these studies in this post, and discuss several potential impacts we should keep in mind for peoples’ health and
Improve Sleep, Improve the World and Health: ResMed’s Look at Global Sleep Trends

The world would be a better place if we had more, and better quality sleep. That’s the hopeful conclusion from the fifth annual Global Sleep Survey from ResMed. ResMed’s global reach with the sleeping public enabled the company to access the perspectives of over 30,000 respondents in 13 markets, finding that one in 3 people have trouble falling or staying asleep 3 or more times a week. We now live in “a world struggling with poor sleep” — “a world without rest,” ResMed coins our sleepless situation. The irony is that most people believe
Health/Care at Super Bowl LIX, GLP-1s, Kaiser and Tufts on Food-As-Medicine, and the RFK, Jr. Factor: A Health Consumer Check-In

In the wake of the always-creative ads for Super Bowl and last Sunday’s LIX bout, game-watchers got to see a plethora of commercials dedicated to the annual event’s major features: food and game-day eating. Oh, and what’s turned out to be the most controversial commercial, the one on GLP-1s from Hims & Hers. In that vein, and converging with many news and policy events, I’m trend-weaving the latest insights into that most consumer-facing of the social determinants of health: food, and in particular, health consumers viewing and adopting food as part of their health and well-being moves. First, to the
Some Bipartisan Concurrence on Health Care Issues in the U.S. – But Trust in Health Care Isn’t Bipartisan – KFF’s January 2025 Polls
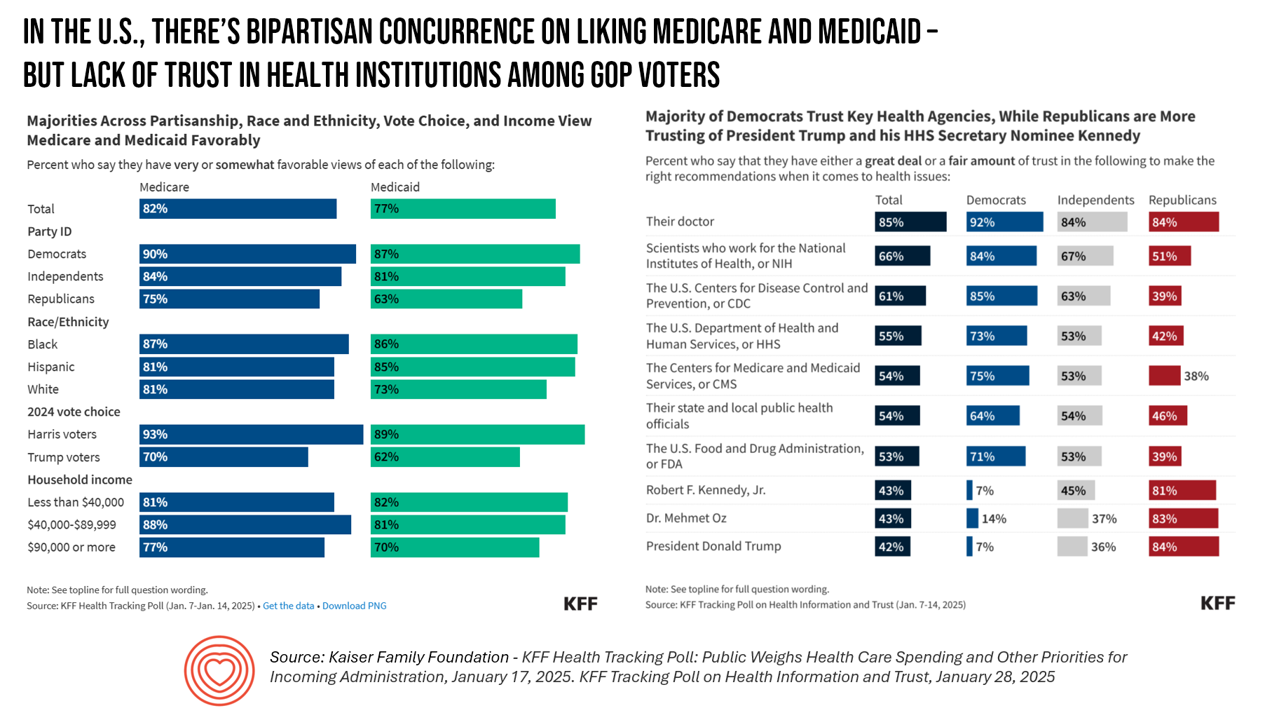
Two polls from one poll source paint at once a bipartisan and bipolar picture of U.S. health citizens when it comes to health care issues versus health care institutions in America. The Kaiser Family Foundation has hit the 2025 health policy ground running in publishing the January 2025 Health Tracking Poll last week and a poll on health care trust and mis-information yesterday. First, the health tracking poll which finds some concurrence between Democrats and Republicans on several big issues facing Americans and various aspects of their health care. As
Seeing Health/Care Everywhere at CES 2025: My Preview for #CES2025

Health/care is everywhere is the mantra on the back of my business card. And at #CES2025, that will indeed be the situation. The 2025 convening of CES (once known as the Consumer Electronics Show) in Las Vegas officially kicks off on 7 January 2025. But I’ll be there beginning 3rd January, scheduling pre-show meetings with innovators, analysts, and my own clients who will be attending the meeting. This will be my 15th year participating in CES, and marking over a decade as a member of the Consumer Technology Association (CTA). As someone who has tracked
The Rough Guide to Health/Care Consumers in 2025: The 2025 Health Populi TrendCast
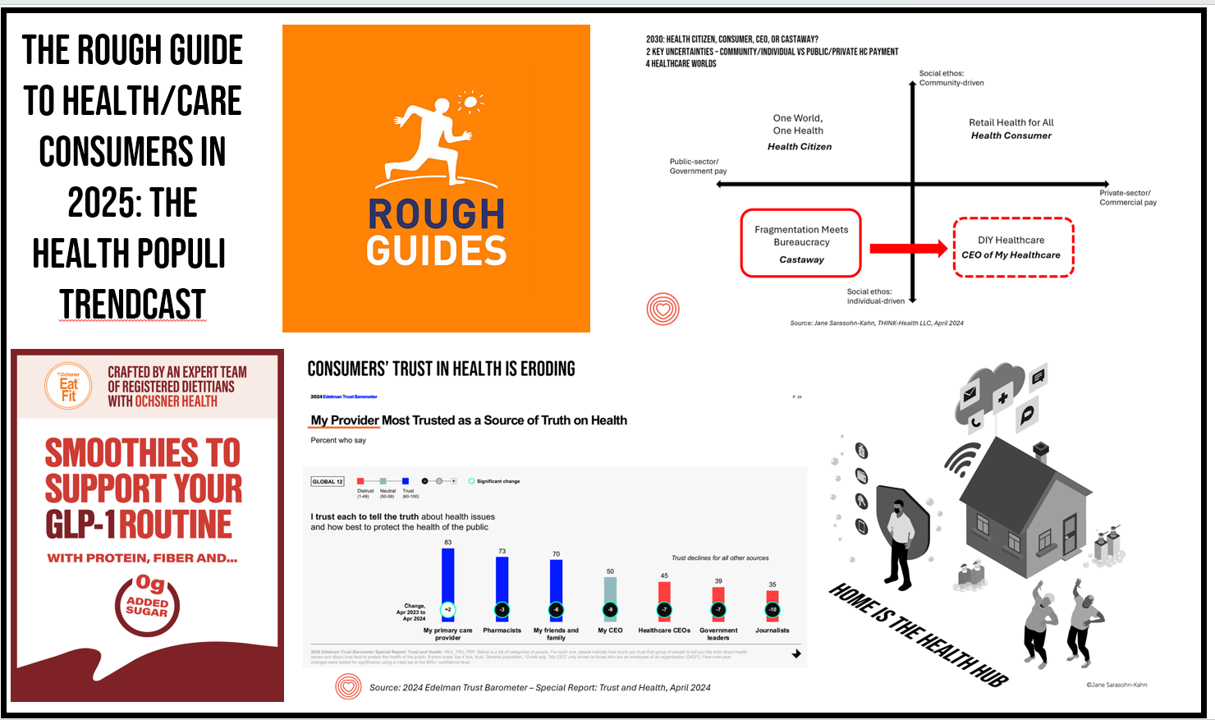
At this year-end time each year, my gift to Health Populi readers is an annual “TrendCast,” weaving together key data and stories at the convergence of people, health care, and technology with a look into the next 1-3 years. If you don’t know my work and “me,” my lens is through health economics broadly defined: I use a slash mark between “health” and “care” because of this orientation, which goes well beyond traditional measurement of how health care spending is included in a nation’s gross domestic product (GDP); I consider health across the many dimensions important to people, addressing physical,
National Healthcare Spending in the U.S. Was Nearly $5 Trillion (with a “T”) in 2023 – New Data from CMS
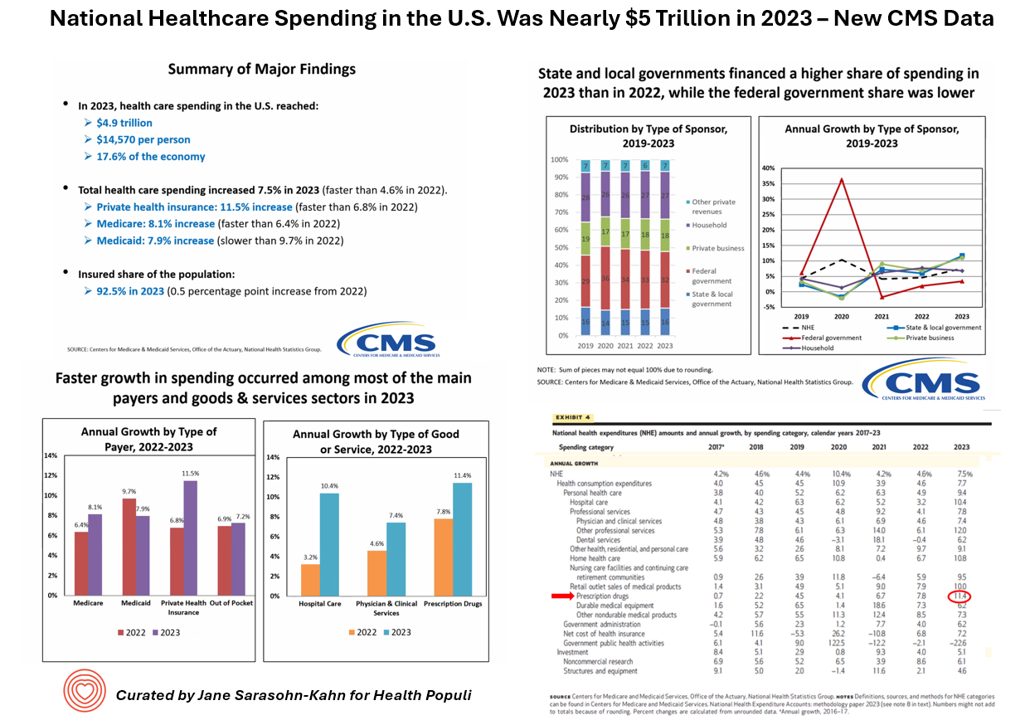
What would $5 trillion be valued around the world or on the stock market? The economy of Germany was gauged around $5 trillion in 2024. India could be the world’s 3rd largest economy by 2026 valued at $5 trillion. Nvidia could be a $5 trillion company in 2025, as could Amazon. But today we report out the latest data from the Centers for Medicare and Medicaid Services (CMS) that national health spending in America reached $4.9 trillion in 2023. The full report on national health expenditures (NHE) in the U.S. was published today in Health Affairs, which came off embargo
Americans’ Views on the Quality of Healthcare Fell to a Record Low — with Costs Ranking as the Most Urgent Problem for Health in the U.S.
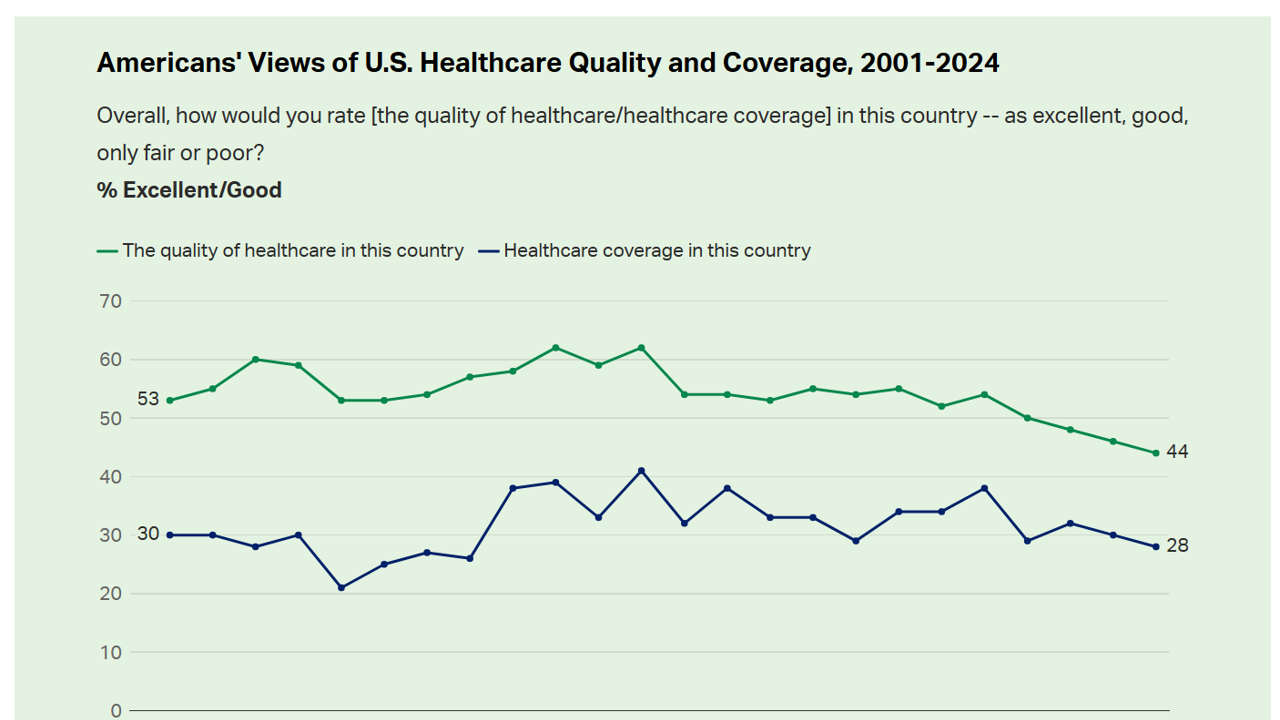
Americans’ perception of the quality of health care in the U.S. fell to the lowest level since 2001, Gallup found in a poll of U.S. health citizens’ views on health care quality, published December 6, 2024. In 2024, only 44% of Americans said that the quality of health care int he U.S. was excellent or good — conversely, 56% of Americans though health care quality was only fair or poor. By political party, that included 50% of Democrats evaluating the quality of care highly compared with 42% of Republicans. Only 28% of people in
Workers Feel “Stuck,” Under-Insured, Financially Stressed, and Neglecting Mental Health
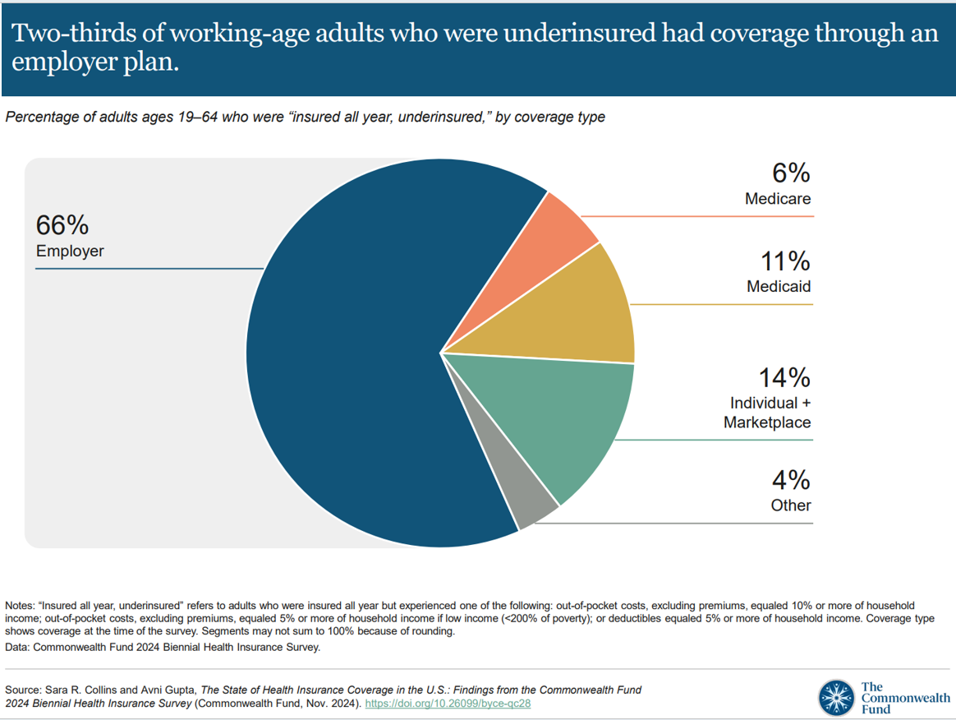
“It’s the economy stupid,” Jennifer Tescher, CEO of the Financial Health Network, titles her latest column in Forbes. Published two weeks after the 2024 U.S. elections, Jennifer’s assertion sums up what, ex post facto, we know about what most inspired American voters at the polls in November 2024: the economy, economics, inflation, the costs of daily living….pick your noun, but it’s all about those Benjamins right now for mainstream American consumers across many demographic cuts. With that realization, we must remind ourselves as we enter a new year under a second-term President Trump that health care spending for everyday people
What Stays True for U.S. Health Care Post #Election2024 (1) – Consumers’ Dissatisfaction with Drug Prices
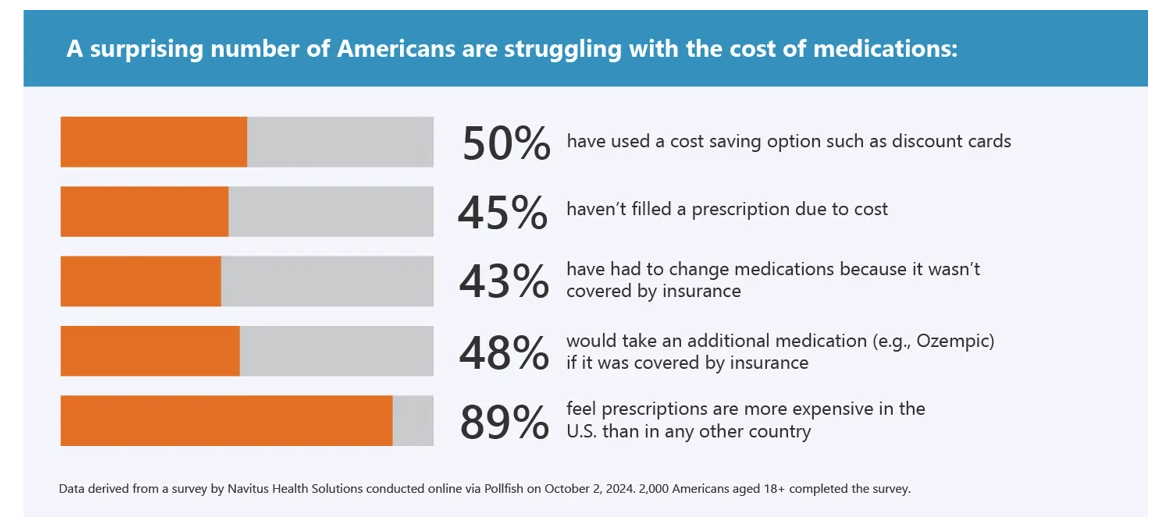
For health care, there are many uncertainties as we reflect, one week after the 2024 U.S. elections, on probably policy and market impacts that we can expect in 2025 and beyond. In today’s Health Populi post, I’ll reflect on the first of several certainties we-know-we-know about U.S. health citizens and key factors shaping the American health ecosystem. In this first of several posts on “What Stays True for U.S. Health Care Post #Election2024,” I’ll focus on U.S. consumer dissatisfaction with drug prices — across political party identification. Let’s set the context with data from a recently-published
Health Care Costs and Access On U.S. Voters’ Minds – Even If “Not on the Ballot” – Ipsos/PhRMA
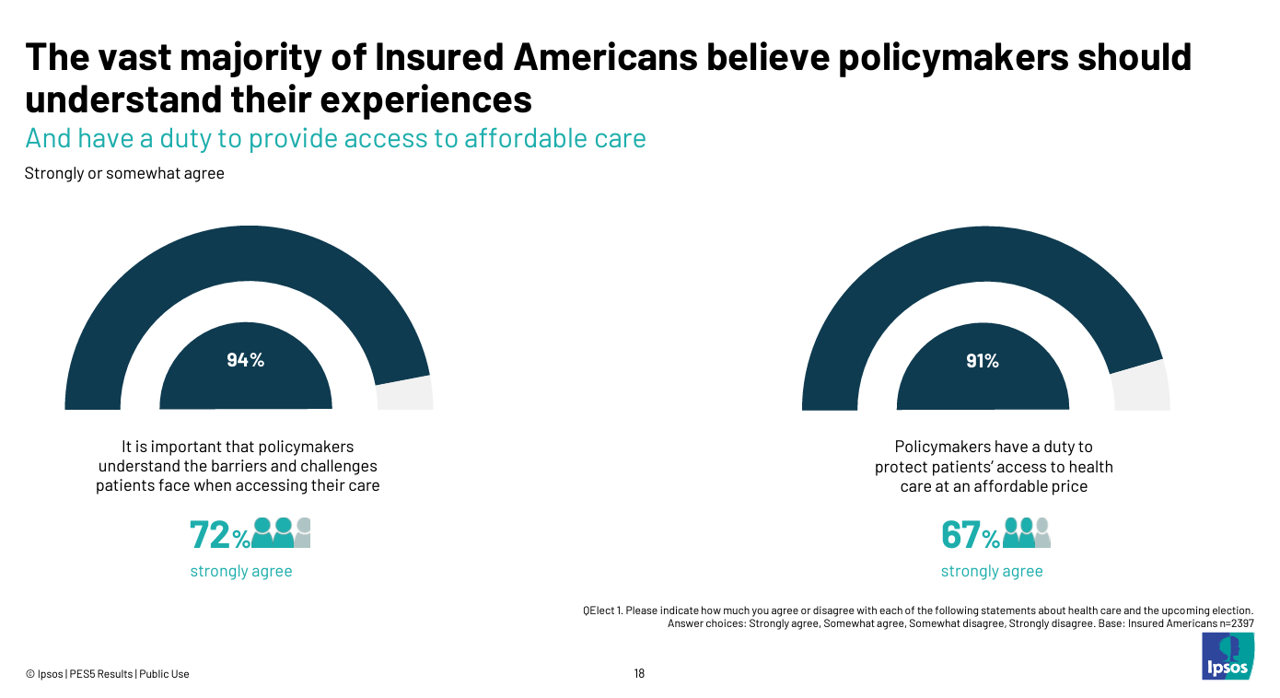
Today marks eight days before #Election2024 in the U.S. While many political pundits assert that “health care is not on the ballot,” I contend it is on voters’ minds in many ways — related to the economy (the top issue in America), social equity, and even immigration (in terms of the health care workforce). In today’s Health Populi blog, I’m digging into Access Denied: patients speak out on insurance barriers and the need for policy change, a study conducted by Ipsos on behalf of PhRMA, the Pharmaceutical Research and Manufacturers of America — the pharma industry’s advocacy organization (i.e., lobby
Closing the Chasm Between Patients and Clinicians With Digital Health Tools – Some Health Consumer Context for #HLTHUSA

As the annual HLTH conference convenes this week in Las Vegas, numerous reports have been published to coincide with the meeting updating various aspects of technology, health care, providers and patients. In this post, I’m weaving together several of the papers that speak to the intersection of health care, consumers, and technology – the sweet spot here on Health Populi. I hope to provide attendees of HLTH 2024 along with my readers who aren’t in Vegas useful context for assessing the new ideas and business model announcements as well as a practical summary for those of you in planning mode for
Obesity is a Public Health Epidemic in the U.S. — The Case for GLP-1 Coverage, Affordability and Equity
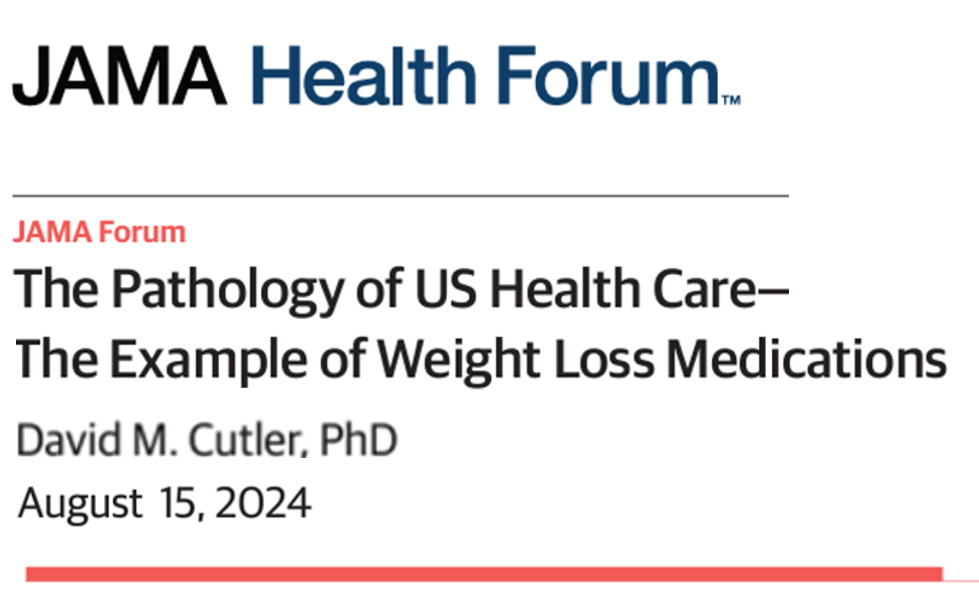
“If the U.S. were sensible, weight management would be treated as a public health issue,” David Cutler writes in the JAMA Health Forum dated August 15, 2024. Dr. Cutler, distinguished economics professor at Harvard, talks about “the pathology of U.S. health care” citing the example of weight loss medications — in short, the uptake of GLP-1 drugs to address Type 2 diabetes first, and subsequently obesity. Dr. Cutler notes that the price of these drugs in the U.S. “far exceeds” that of other countries: specifically, 9 times that of the prices in Germany and the Netherlands
Where Democrats and Republicans Agree on Health Care Policies – From Medicare and Prescription Drugs to Gun Safety
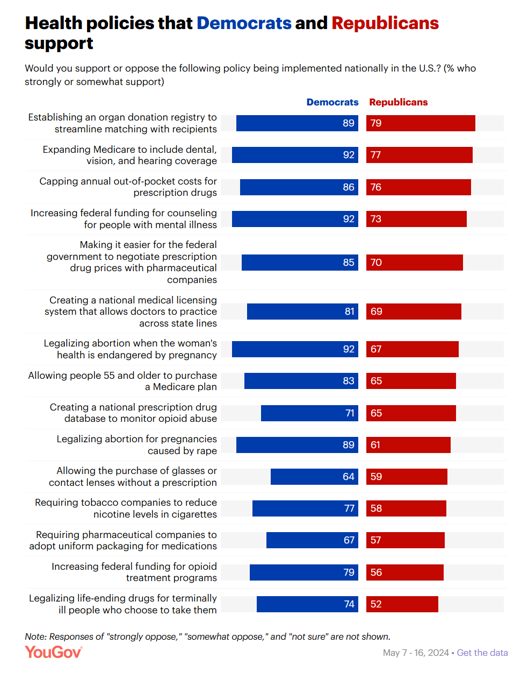
In a super-divided electorate like the U.S. with about 60 days leading up to the 2024 Elections, we might assume there are no “purple” areas of agreement between the Red (Republicans) and the Blue (Democrats) thinking in PANTONE color politics. Surprisingly, there are many health policies on which Democrats and Republicans concur, as found in a series of YouGov polls conducted in May 2024. YouGov fielded the health policies poll in five waves online, each among roughly 1,100 U.S. adults in May 2004. This bar chart summarizes health
The Health Care Costs for Someone Retiring in 2024 in the U.S. Will Reach $165,000 – Fidelity’s 23rd Annual Update
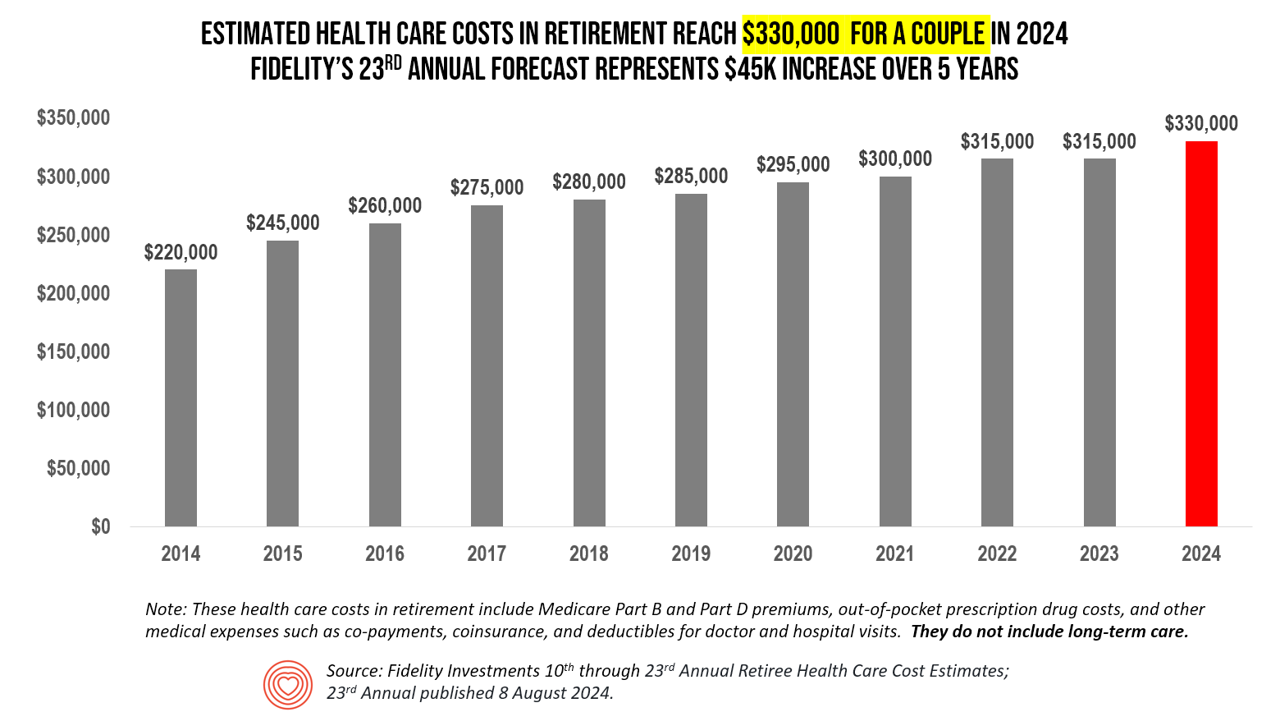
The average person in the U.S. retiring in 2024 will need to bank $165,000 to pay for health care costs in retirement — a sum that does not include long-term care, Fidelity Investments advises us in the 23rd annual look at this always-impactful (and sobering) forecast. I’ve covered this study every year since 2011 here in Health Populi, continuing to add to this bar chart; in the interest of space and legibility, I started this year’s version of the chart at 2014, when the cost for a couple was gauged at $220K. Fidelity began
What’s Expected to Drive Up Health Plan Costs in 2025: GLP-1s, Behavioral Health, and Inflationary Pressures for Hospitals and Doctors – PwC’s Behind the Numbers 2025
The U.S. Bureau of Labor Statistics had good news for American consumers long-facing inflation for household spending over the past couple of years, announcing on July 11, 2024, that the general consumer price index (CPI) fell, lowering real prices for people buying airline tickets, used cars and trucks, communication, and petrol to fill auto tanks. That positive economic news did not extend to medical care and personal care, the BLS reported, whose costs increased by 3.3% and 3.2%, respectively. (Motor vehicle insurance costs grew a whopping 19.5% in the report, FYI). Following the
Medical Debt, Aflac on Eroding Health Benefits, the CBO’s Uninsured Forecast & Who Pays for Rising Health Care Prices: A Health Consumer Financial Update
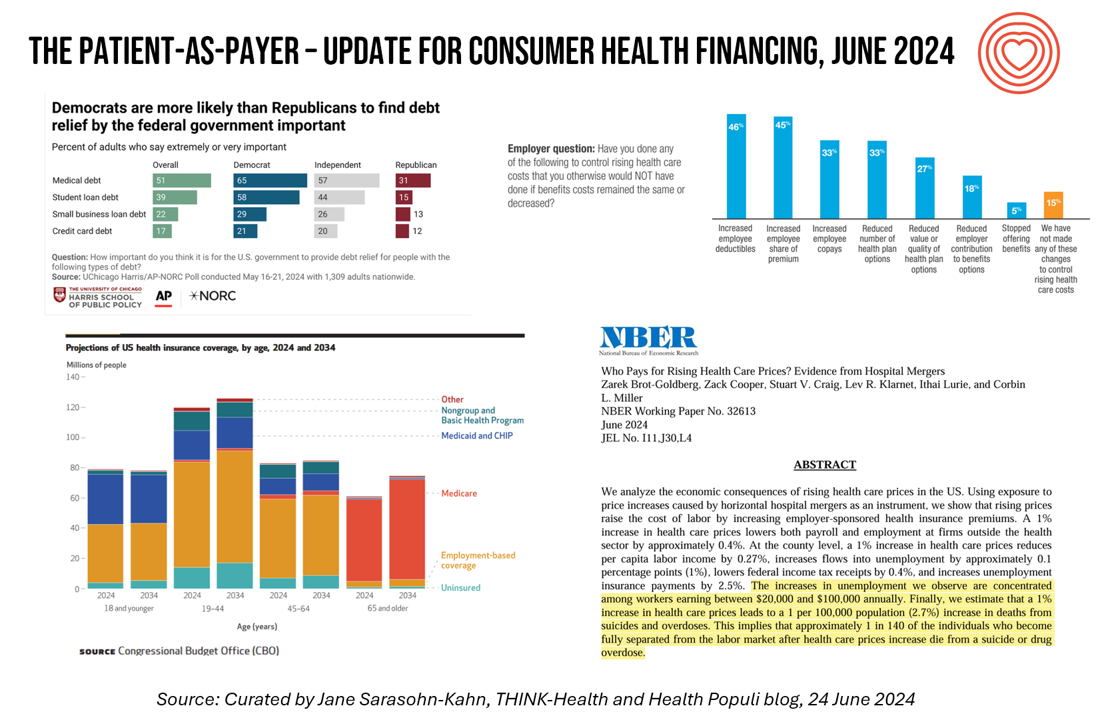
On June 11, Rohit Chopra, the Director of the Consumer Financial Protection Bureau (CFPB) announced the agency’s vision to ban Americans’ medical debt from credit reports. He called out that, “In recent years, however, medical bills became the most common collection item on credit reports. Research from the Consumer Financial Protection Bureau in 2022 showed that medical collections tradelines appeared on 43 million credit reports, and that 58 percent of bills that were in collections and on people’s credit records were medical bills.” Chopra further explained that medical debt on a consumer credit report was quite different than other kinds
A 2025 Subaru Forester, a Year at U-New Mexico, or a Health Plan for a Family of Four: the 2024 Milliman Medical Index
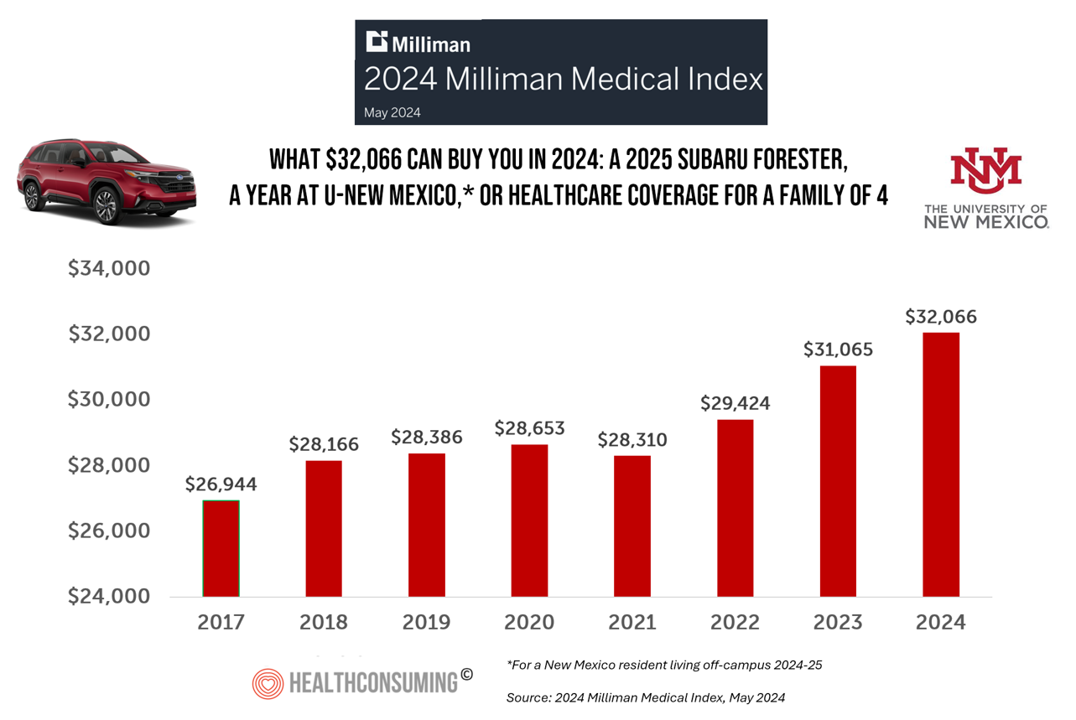
Health care costs for an “average” person covered by an employer-sponsored PPO in the U.S. rose 6.7% between 2023 and 2024, according to the 2024 Milliman Medical Index. Milliman also calculated that the largest driver of cost increase in health care, accounting for nearly one-half of medical cost increases, was pharmacy, the cost of prescription drugs, which grew 13% in the year. The big number this year is $32,066, which is the cost of that employer-sponsored PPO for a family of 4 in 2024. I’ve curated the chart of the MMI statistic for many
The Thematic Roadmap for AHIP 2024: What the Health Insurance Conference Will Cover

Health insurance plans make mainstream media news every week, whether coverage deals with the cost of a plan, the cost of out-of-network care, prior authorizations, or cybersecurity and ransomware attacks, among other front-page issues. This week, AHIP (the acronym for the industry association of America’s Health Insurance Plans) is convening in Las Vegas for its largest annual 2024 meeting. We expect at least 2,400 attendees registered for the meeting, and they’ll not just be representing the health insurance industry itself; folks will attend #AHIP2024 from other industry segments including pharmaceuticals, technology, hospitals and health systems, and the investment and financial services
The ROI on Patient Experience = Loyalty, Trust and Revenue – Listening to Accenture
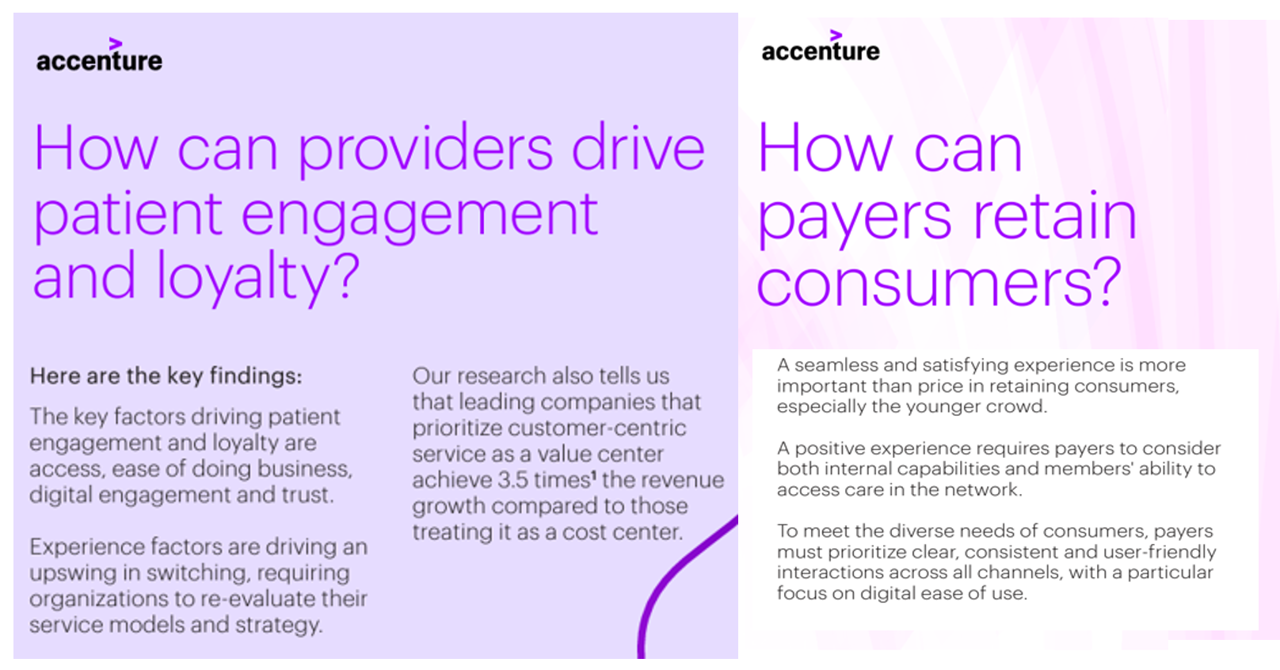
When health care providers and payers make patients’ lives easier, there’s a multiplying factor for loyalty and revenue growth, according to Accenture’s latest look into the value of experience in The Power of Trust: Unlocking patient loyalty in healthcare. Accenture conducted two surveys for this research, assessing nearly 16,000 U.S. adult consumers’ views on healthcare providers and health insurance plans. Several factors underpin patients’ selection of a new health care provider, especially: Access (70%), with a convenient location, quickly available appointments, digital/mobile/social interactions, and virtual care availability; and, The provider being a trusted source
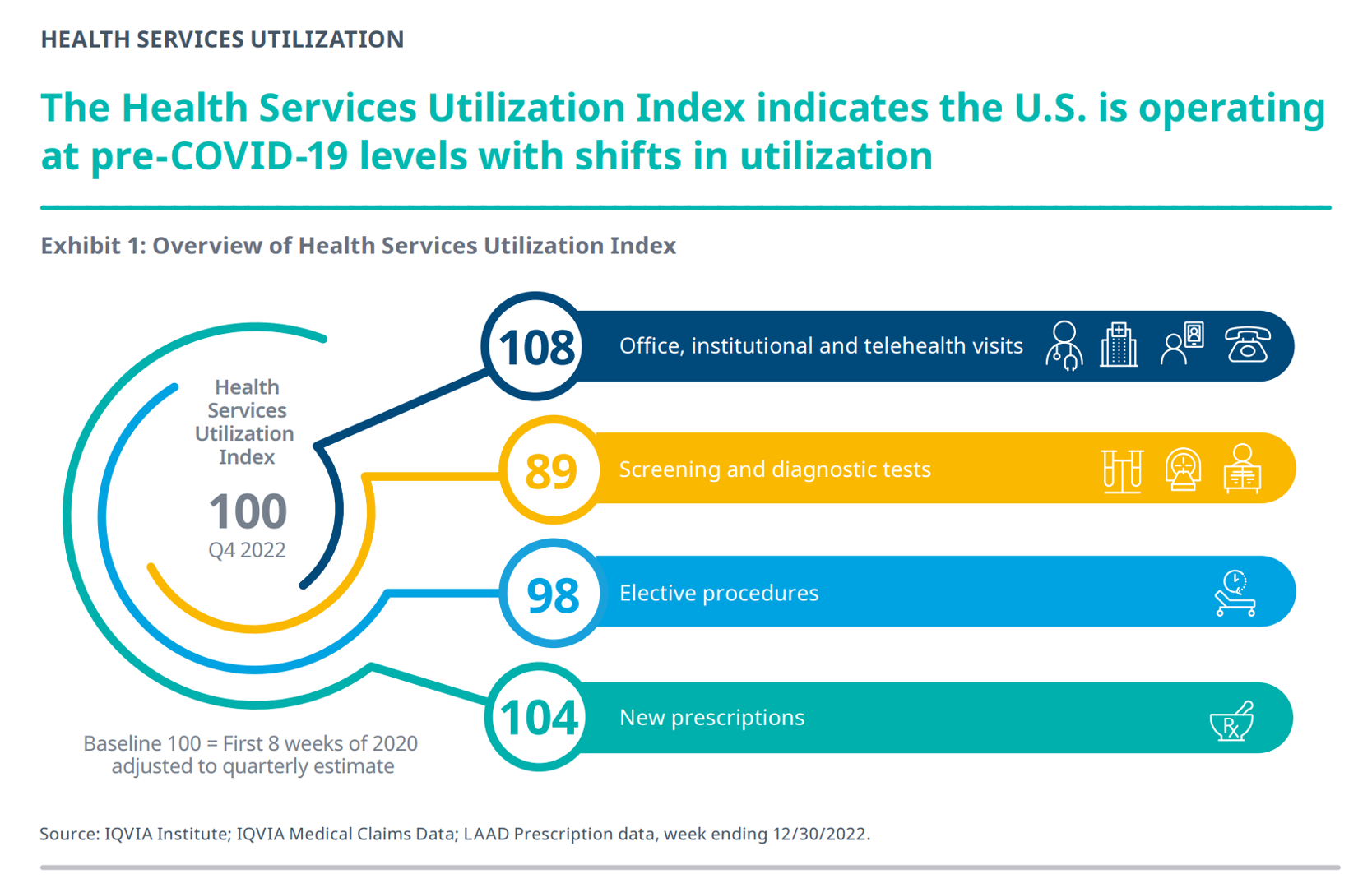
Prescriptions Are Up, Health Services Utilization Down, and GLP-1s Are a Major Growth Driver: IQVIA’s 2024 Update
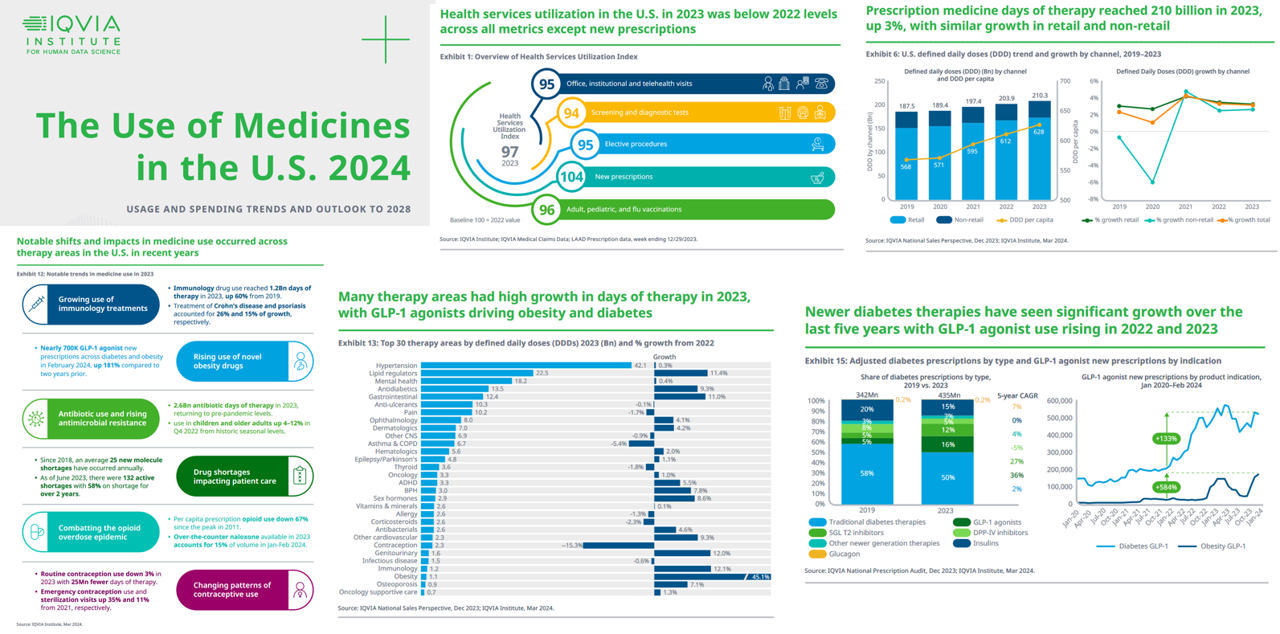
In the past year, the growth of prescription drug utilization and spending has much to do with the use of GLP-1 agonists to treat diabetes and obesity, along with immunology therapy, and lipid meds, along with specialty medicines now accounting for over half of spending — up from 49% in 2018. This update comes from The Use of Medicines in the U.S. 2024 from the IQVIA Institute for Human Data Science. The annual report details trends in health services utilization, the use of prescription drugs, patient financing of those costs, the drivers underpinning the medicines spending, and an outlook to 2028.
Inflation, Health, and the American Consumer – “The Devil Wears Kirkland”
The Wall Street Journal reported yesterday that surging hospital prices are helping to keep inflation high. Hospital costs rose 7.7% last month, the highest increase in 13 years. This chart from WSJ’s reporting illustrates the >2x change in the CPI for hospitals vs the overall rate of price increases. Hospitals are not alone in price cliffs, with health insurance premiums spiking last year at the fastest rate in a decade, the Labor Statistics data showed. “For patients and their employers, the increases have meant higher health-insurance premiums, as well as limiting wage
The Cost of Medical Care, Long-Term Care, and Prescription Drugs Top Older Americans’ Health-Related Concerns – With Social Security and Medicare Top of Mind
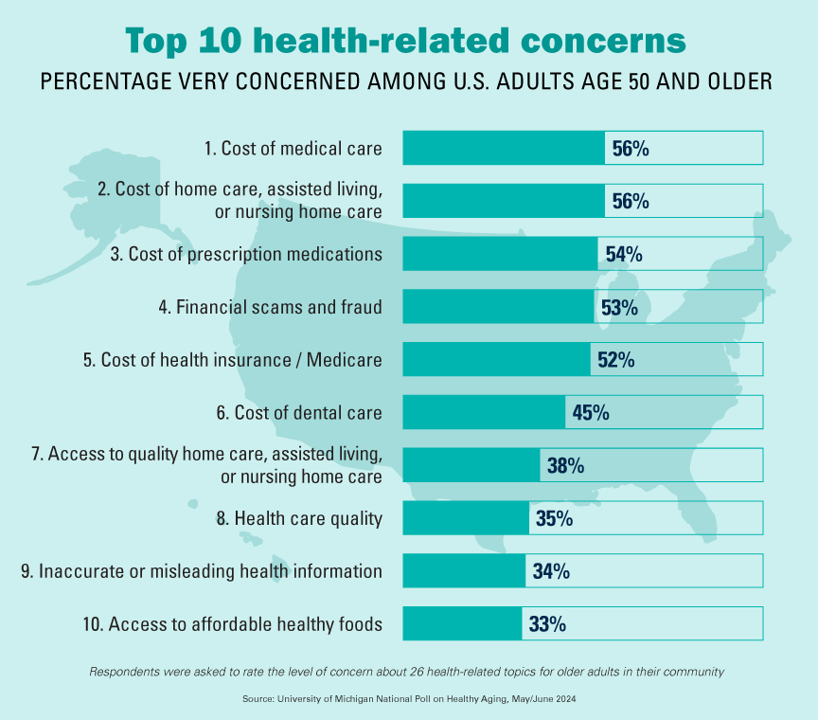
Among Americans 50 years of age and over, the top health-related concerns are Cost, Cost, and Cost — for medical services, for long-term and home care, and for prescription medications. Quality of care ranks lower as a concern versus the financial aspects of health care in America among people 50 years of age and older, as we learn what’s On Their Minds: Older Adults’ Top Health-Related Concerns from the University of Michigan Institute for Healthcare Policy and Innovation. AARP sponsors this study, which is published nearly every month of the year on the Michigan Medicine portal.
A Tax on Moms’ Financial and Physical Health – The 2024 Women’s Wellness Index
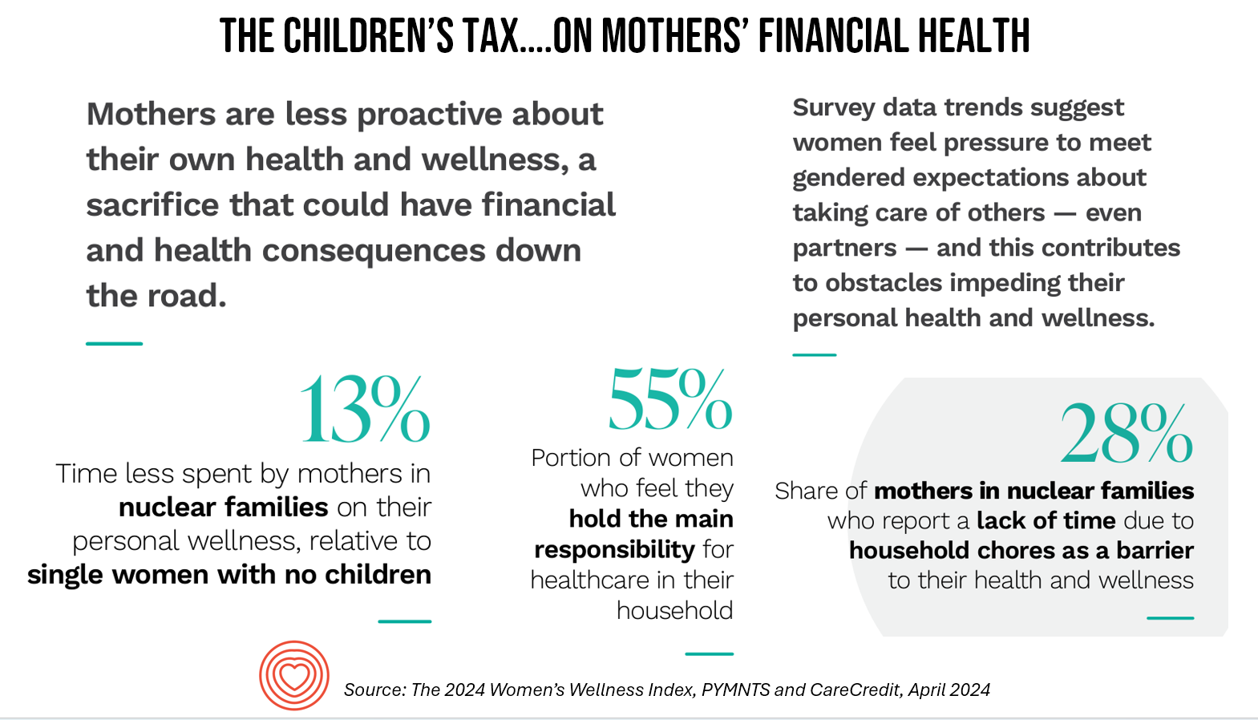
“Motherhood is the exquisite inconvenience of being another person’s everything” is a quote I turn to when I think about my own Mom and the remarkable women in my life raising children. With Mother’s Day soon approaching, the 2024 Women’s Wellness Index reminds us that the act of “being another person’s everything” has its cost. The Index, sponsored by PYMNTS in collaboration with CareCredit, was built on survey responses from 10,045 U.S. consumers fielded in November-December 2023. The study gauged women’s perspectives on finances, family, social life impacts on health and well-being. My key takeaway from
Healthcare 2030: Are We Consumers, CEOs, Health Citizens, or Castaways? 4 Scenarios On the Future of Health Care and Who We Are – Part 2
This post follows up Part 1 of a two-part series I’ve prepared in advance of the AHIP 2024 conference where I’ll be brainstorming these scenarios with a panel of folks who know their stuff in technology, health care and hospital systems, retail health, and pharmacy, among other key issues. Now, let’s dive into the four alternative futures built off of our two driving forces we discussed in Part 1. The stories: 4 future health care worlds for 2030 My goal for this post and for the AHIP panel is to brainstorm what the person’s
Considering Equity and Consumer Impacts of GLP-1 Drugs – A UBS Economist Weighs In
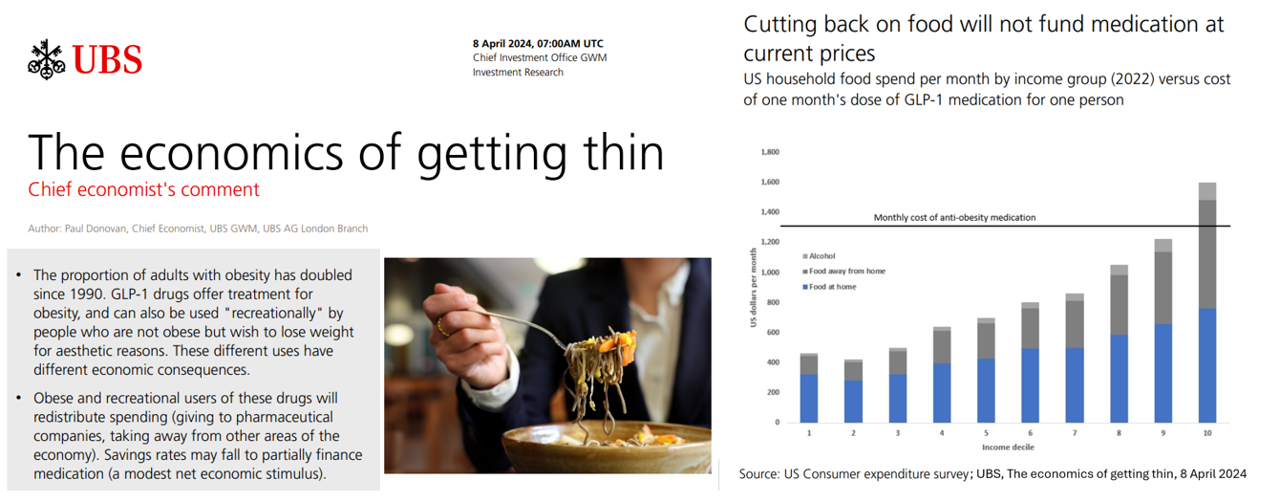
Since the introduction of GLP-1 drugs on the market, their use has split into two categories: for obesity and “recreationally,” according to the Chief Economist with UBS (formerly known as Union Bank of Switzerland). Paul Donovan, said economist, discusses The economics of getting thin in his regularly published comment blog. “These different uses have different economic consequences,” Donovan explains: Obese patients who use GLP-1s should become more productive employees, Donovan expects — less subject to prejudice, and less likely to be absent from work. While so-called recreational GLP-1 consumers may experience these
Consumers Are So Over Their Paper Chase in Health Care Payments

As we start the month of April 2024 in the U.S., it’s tax season in America with Federal (and other) income taxes due on the 15th of the month. This is also the time my research clock alarm goes off for an important annual report that describes the latest profile of the patient-as-payer in the U.S. ‘Tis the season for J.P. Morgan’s InstaMed team to analyze health care payments data, describing the experiences of consumers, providers and payers in the Trends in Healthcare Payments Fourteenth Annual Report. The overall takeaway for
The Economic Contours of the Change Healthcare Cyber Attack: Taking Stock So Far

On February 22, 2024, I went to a CVS Pharmacy-Inside-Target in my community to fill a prescription for benzonatate 200 mg capsules. I had caught a bad case of the flu the week before, and subsequently suffered a very long tail of a cough. That’s TMI for me to write about in the Health Populi blog, but this story has a current-events twist: the pharmacist could not electronically link with my insurance company to transact my payment. He tried a few work-flows, and ended up using a discount card which in the moment worked for us, and I paid the
A Health Consumer Bill of Rights: Assuring Affordability, Access, Autonomy, and Equity
Let’s put “health” back into the U.S. health care system. That’s the mantra coming out of this week’s annual Capitol Conference convened by the National Association of Benefits and Insurance Professionals (NABIP). (FYI you might know of NABIP by its former acronym, NAHU, the National Association of Health Underwriters). NABIP, whose members represent professionals in the health insurance benefits industry, drafted and adopted a new American Healthcare Consumer Bill of Rights launched at the meeting. While the digital health stakeholder community is convening this week at VIVE in Los Angeles to share innovations in health tech, NABIP
People With Medical Debt Are Much More Likely to Be in Financial Distress in America
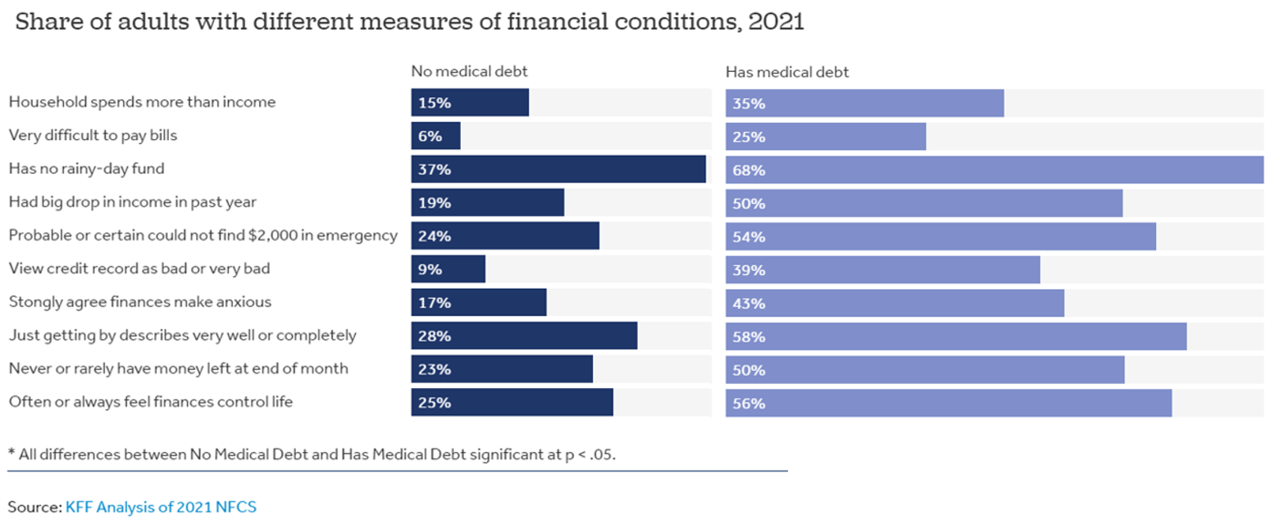
How financially vulnerable are people with medical debt in the U.S.? Significantly more, statistically speaking, we learn from the latest survey data revealed by the National Financial Capabilities Study (NFCS) from the FINRA Foundation. The Kaiser Family Foundation and Peterson Center on Healthcare analyzed the NFCS data through a consumer health care financial lens with a focus on medical debt. Financial distress takes many forms, the first chart inventories. People with medical debt were most likely lack saving for a “rainy day” fund, feel they’re “just getting by” financially, feel their finances control their life, and
Why Elevance Health is “Prescribing” Phones for Members
You’ve heard of food-as-medicine and exercise-as-medicine. Now we see the emergence of telecomms-as-medicine — or more specifically, a driver of health, access, and empowerment. Elevance Health, the health plan organization serving 117 million members, launched a program to channel mobile phones and data plans into the hands of some Medicaid plan enrollees, explained in the organization’s press release on the program. To implement this program and get connectivity into consumers’ hands and homes, Elevance Health is collaborating with several telecomms companies including Verizon, AT&T, Samsung, and T-Mobile. Funding is supported by the FCC’s Affordable Connectivity Program.
In 2024 U.S. Consumers Will Mash Financial Resolutions With Those For Physical Health and Mental Health, Fidelity Finds
One-third of U.S. consumers feel in worse financial shape now than in 2022, with inflation a top concern, discovered in the 2024 New Year’s Financial Resolutions Study from Fidelity Investments. In this 15th annual update of Fidelity’s research into Americans’ New Year’s resolutions for financial health, we learn the mantra that 2024 will be the year of living practically, opening new chapters for saving and paying down debt. Fidelity conducted an online poll among 3,002 U.S. adults 18 and over in October 2023 to gauge peoples’ perspectives on personal finances, and well-being currently and into 2024. This
Healthcare Bills, Affordability, and Self-Rationing Care Will Continue to Challenge U.S. Health Consumers in 2024
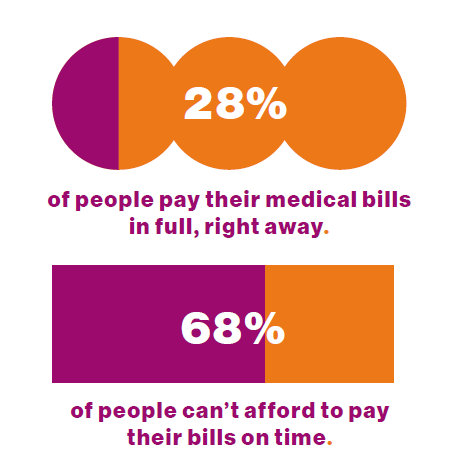
Two-thirds of U.S. consumers say they can’t afford to pay their medical bills on-time, based on the 2023 Consumer Survey from Access One, a financial services company focused on healthcare payments. The report’s title page asks the question, “What options do consumers really want for paying healthcare expenses?” The survey report responds to that question, finding out that nearly one-half of patients have taken some kind of action to reduce their medical expenses. Furthermore, one-third of consumers are not confident they could pay a medical bill of $500 or more. Access One fielded
Everybody is Stressed in America, and It’s Not Good for Our Health: the 2023 Update from the American Psychological Association

The U.S. is “a nation recovering from collective trauma,” the according to the latest survey on Stress in America 2023 from the American Psychological Association (APA). The APA has been quantifying Stress in America since 2007; for context, at the end of that year The Great Recession kicked in, and in response President Obama’s team put together assistance to bolster the national economy, jobs, and health technology (codified in the American Recovery and Reinvestment Act). American health citizens are experiencing a deja vu in 2023 akin to their financial stress experienced in the APA 2008 Stress
How Healthcare and Patients Can Benefit From a “Simplicity Premium”
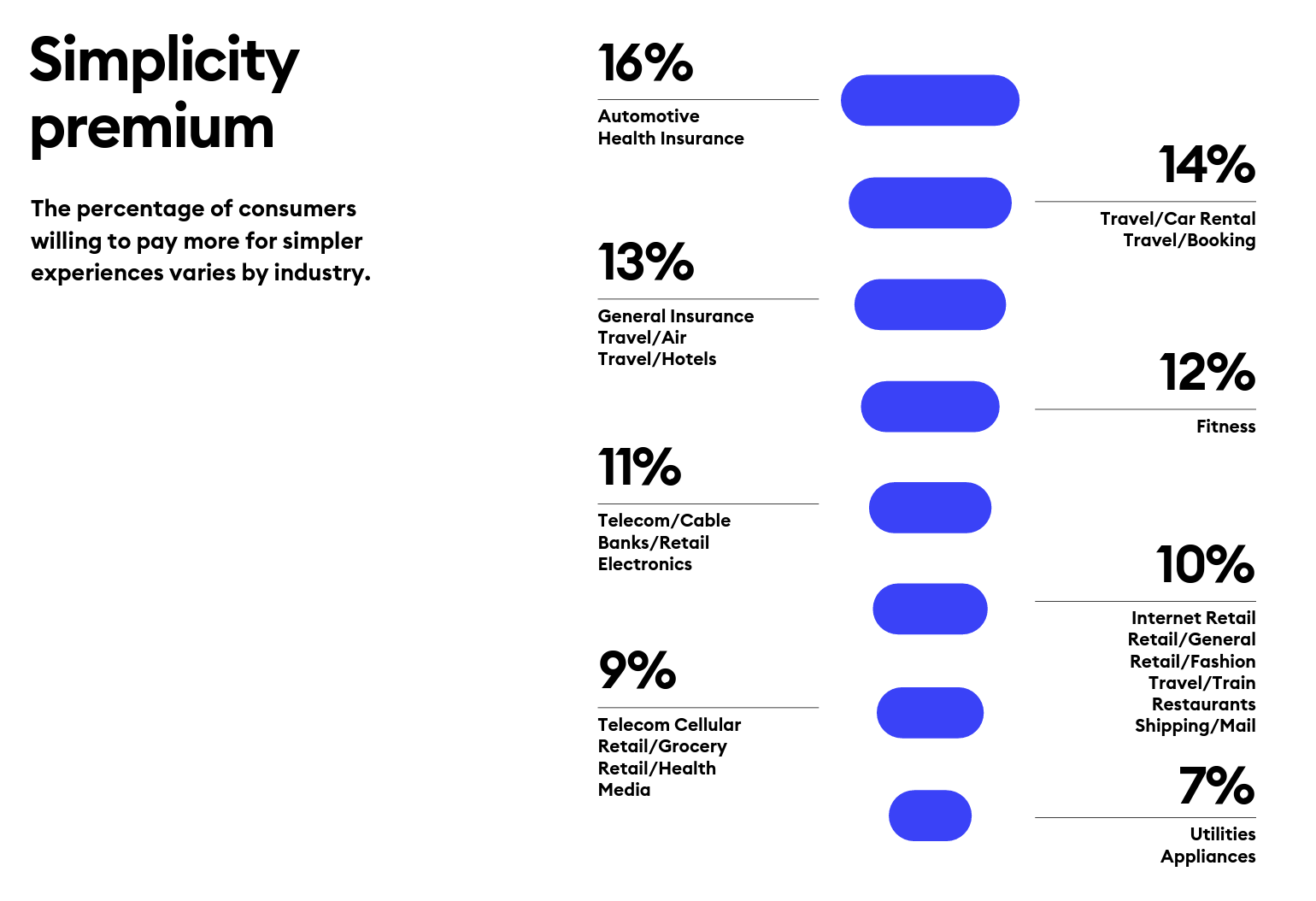
“Simplicity is the ultimate sophistication,” Leonardo DaVinci wrote through his lens on innovation. Simplicity can be a transformational cornerstone of health/care innovation, we learn from Siegel+Gale’s report on the World’s Simplest Brands Tenth Edition (WSBX). Siegel+Gale found the most consumers are willing to pay more for simpler brand experiences and are more likely to recommend a brand for those simpler experiences, as well. Across the 15,000 consumers the firm polled globally (across nine countries), five key factors underpin peoples’ experiences with the enchantingly “simple” companies: they are, Easy to understand Transparent and honest Caring for
Slip Slidin’ Away: the Reputations of Pharma and Healthcare in the U.S. Decline in the Latest Gallup Poll
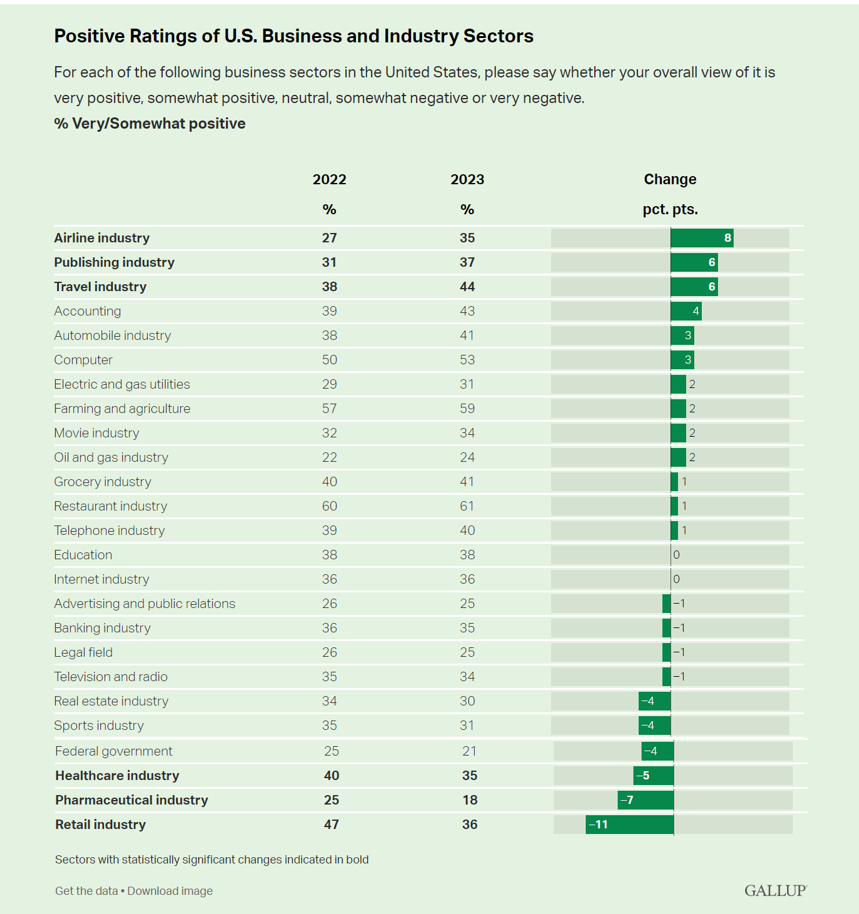
Oh, how quickly people forget…and slow to forgive. U.S. consumers’ positive views for healthcare, pharma and retail have significantly fallen in just one year, the latest annual Gallup poll of industry rankings in America found as of August 2023. This stat for the pharma industry was the lowest Gallup ever recorded for the sector since 2001. I can’t help hearing Paul Simon’s lyrics to Slip Slidin’ Away….”you know the nearer your destination, the more you’re slip slidin’ away” when it comes to health citizens’ perceptions of pharma and the healthcare
Large Employers Expect More Employees Will Experience Prolonged Health Impacts Due to COVID-19. and a Note About Telehealth Engagement
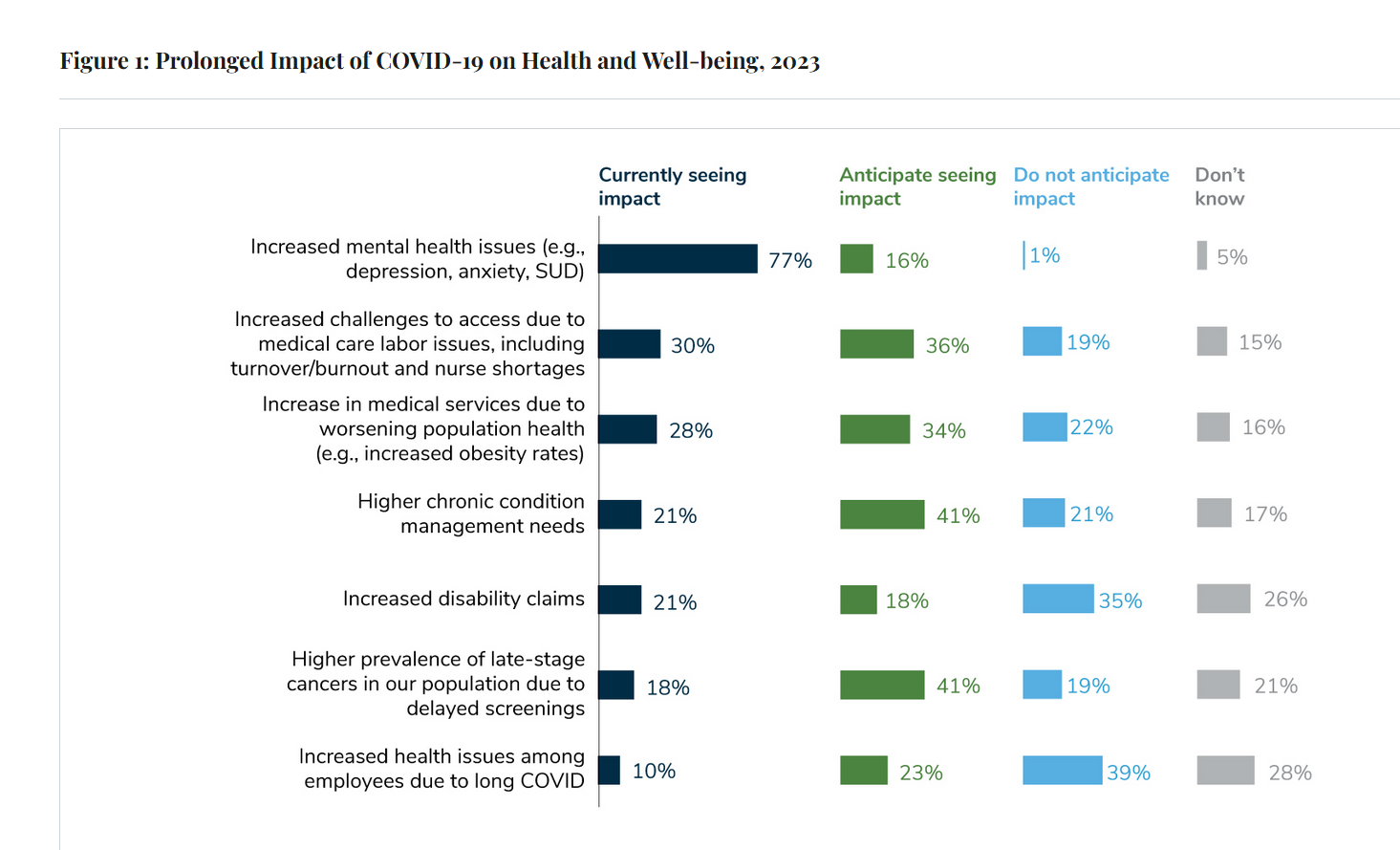
Due to their delayed return to medical services and diagnostic testing in the COVID-19 pandemic era, U.S. employees are expected to sustain serious health impacts that will drive employers’ health care costs, envisioned in the 2024 Large Employer Health Care Strategy Survey from the Business Group on Health (BGH). Dealing with mental health issues is the top health and well-being impact workers in large companies are addressing in 2023. Looking forward, large employers foresee their workers will be seeking care for chronic conditions and later-stage cancers that are diagnosed due to delayed screenings.
Personalizing Health Means Personalizing Health Insurance for Patient-Members – Learning from HealthEdge
As patients assume more financial skin in their personal healthcare, they take on the role of demanding consumer, or “impatient patients.” HealthEdge’s latest research into health consumers’ perspectives finds peoples’ satisfaction with their health insurance plans lacking, with members seeking easier access their personal health information, high levels of service, and rewards for healthy behaviors. Health plans would also boost consumers’ satisfaction by channeling patients’ access to the kinds of medical providers that align with consumers’ preferences and personal values, and by personalizing information to steer people toward lower-cost care.
To Avert a GLP-1 Cost Tsunami, Add Lifestyle Interventions: Learning from Virta Health
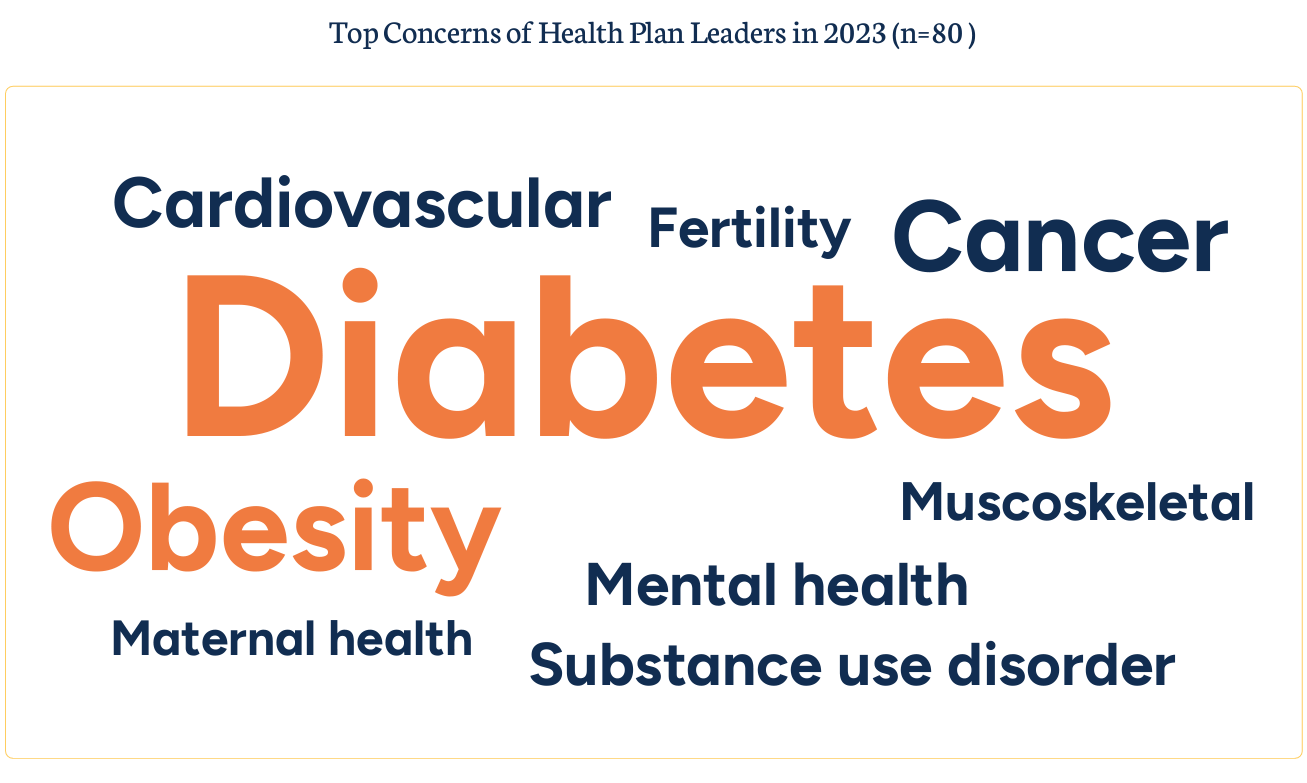
With consumer and prescriber interest in GLP-1 receptor agonist drugs “soaring,” health plan managers have a new source of financial stress and clinical questions on their to-do list. A team of Virta Health leaders held a webinar on 13th July 2023 to explain the results of a study the company just completed assessing health plan execs’ current views on Ozempic and other GLP-1 medicines with a view on both clinical outcomes and cost implications for this growing category of drugs that address diabetes and obesity. Indeed, diabetes and obesity are top health concerns among the
The Latest KFF Poll on Consumer Experiences with Health Insurance Speaks Volumes About Patients’ Administrative Burden
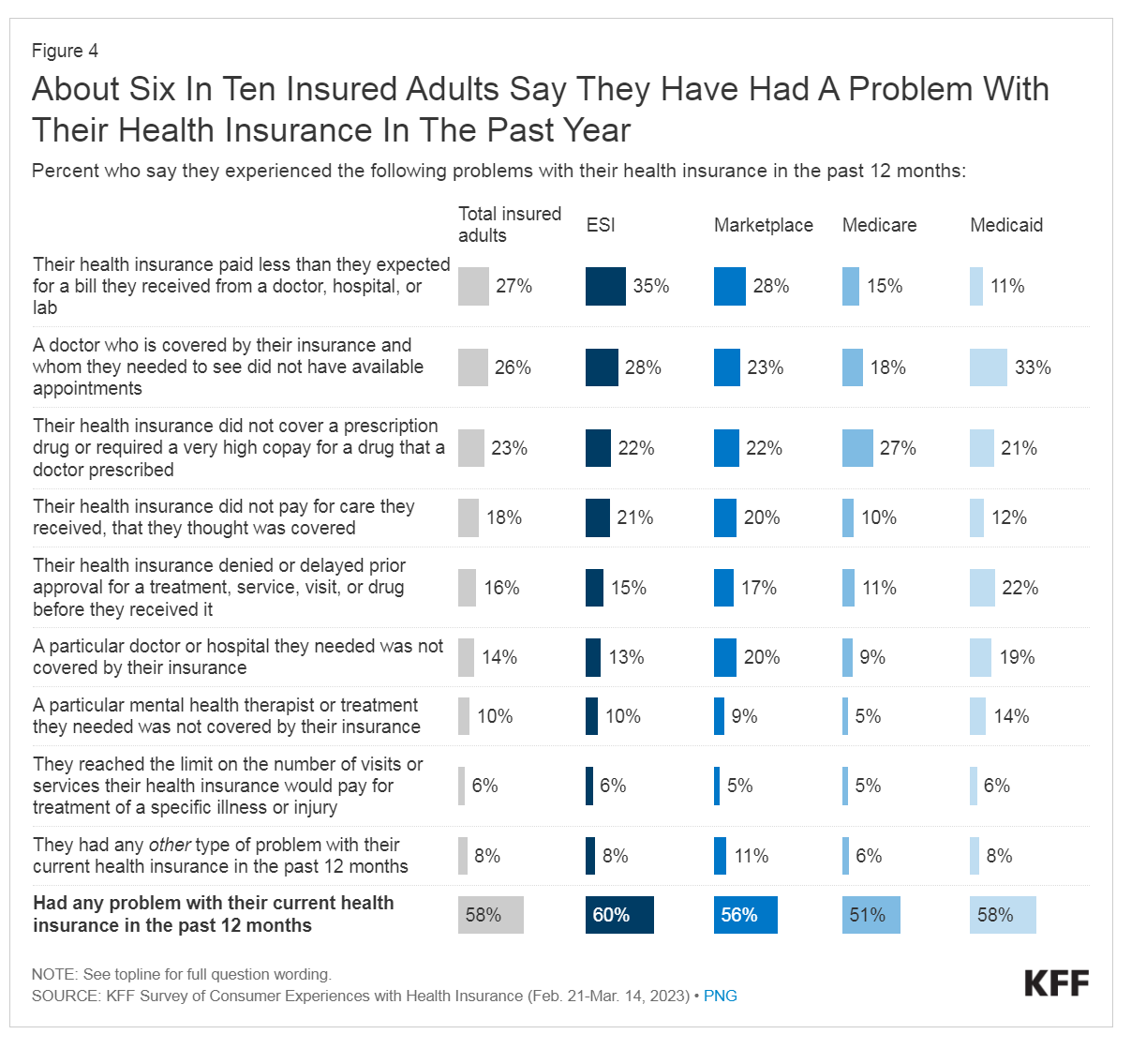
People love being health-insured, but their negative experiences with health plans create serious burdens on patients-as-consumers. And those burdens impact even more people who are unwell than healthier folks. The 2023 Kaiser Family Foundation Survey of Consumer Experiences with Health Insurance updates our understanding of and empathy for insured peoples’ Patient Administrative Burdens (PAB). For this study, KFF polled 3,605 U.S. adults 18 and over in February and March 2023 who had health insurance across different plan types. Over the past several years, I’ve come to appreciate the concept of PAB by listening to and learning from colleagues Dr, Grace
The State of Healthcare in America, State-By-State
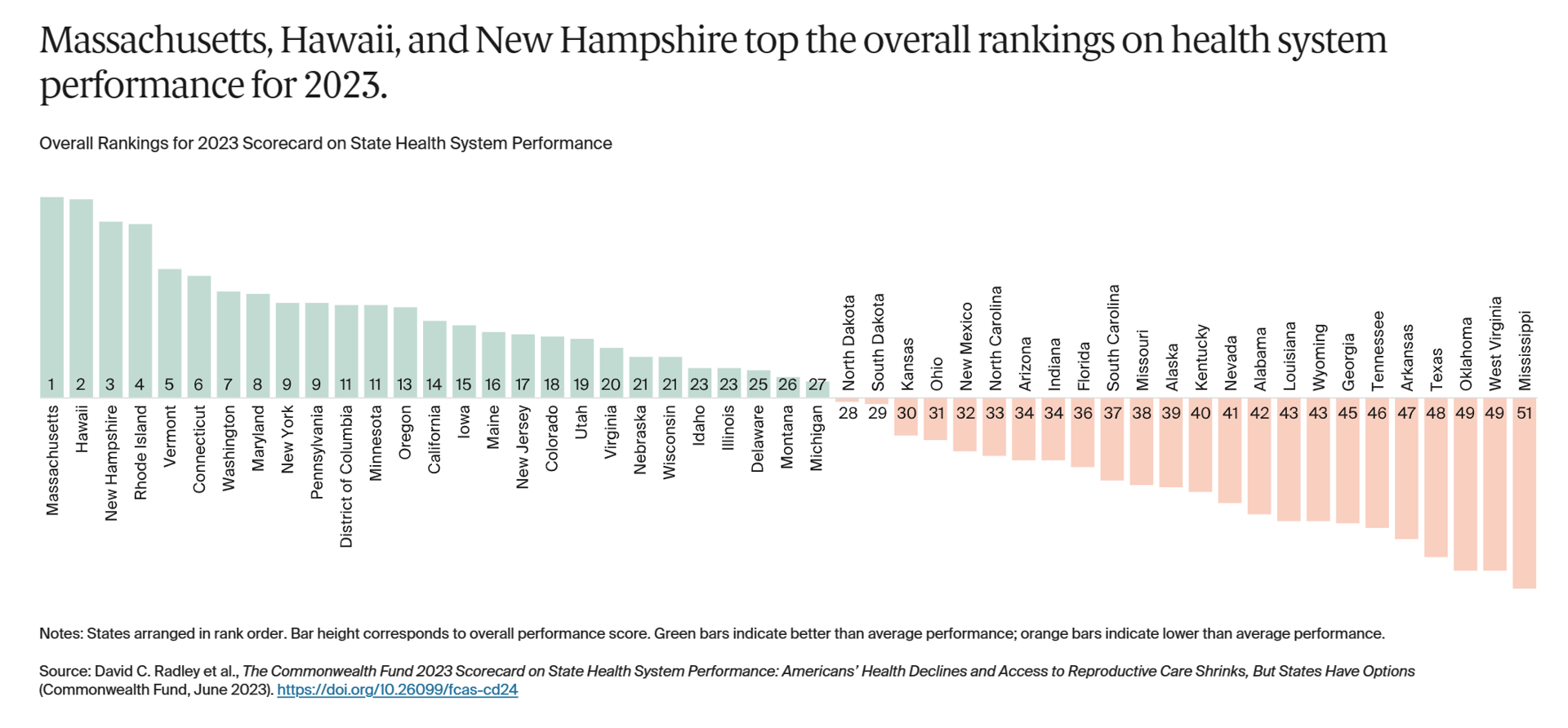
If you live in Massachusetts, Hawaii, and New Hampshire, you win a kind of state lottery for public health and well-being, based on this year’s read of the 2023 Scorecard on State Health System Performance from The Commonwealth Fund. Here’s a picture of the annual study’s top-line findings, a roster of the fifty U.S. states ranked by a mash-up of health system indicators. As Annie Burkey of FierceHealthcare succinctly summed it up, the “Commonwealth Fund gives healthcare in southeastern states failing grades across the board.” I’ll give you more details about the Top and Bottom
Consumers and Cancer: 3 Patient-Focused Charts From IQVIA on the State of the Oncology in 2023 – and Introducing CancerX
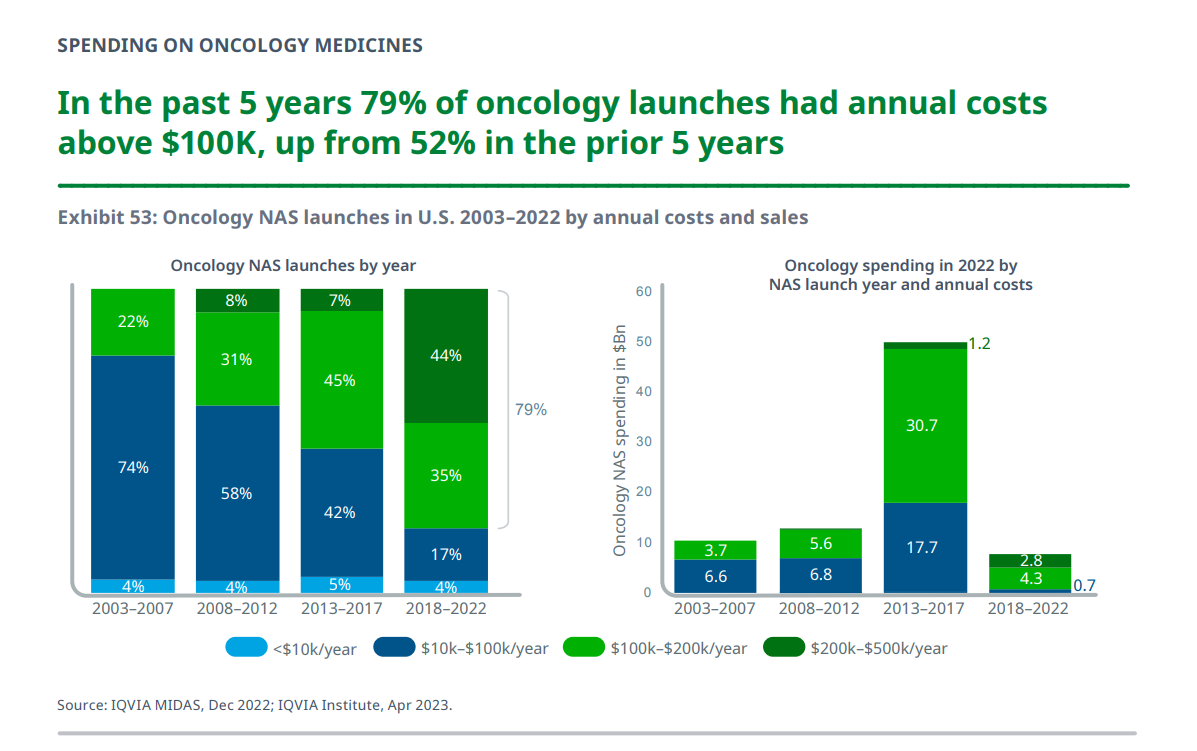
It’s time for the annual ASCO conference, currently convening the American Society for Clinical Oncology in Chicago. Starting 2nd June, there have been dozens of positive announcements updating research and therapies bringing hope to the 2 million new patients who will be diagnosed with cancer in the U.S. in 2023, and millions of more people worldwide. Just in time for #ASCO2023, the IQVIA Institute published their annual report on Global Oncology Trends 2023 – Outlook to 2027, an update featuring pipelines, therapy approvals, research updates, costs of oncology products, and patients.
What $31,065 Can Buy You: a Toyota Corolla Cross Hybrid, a Year at Gnomon School, or Healthcare for a Family of 4 in America
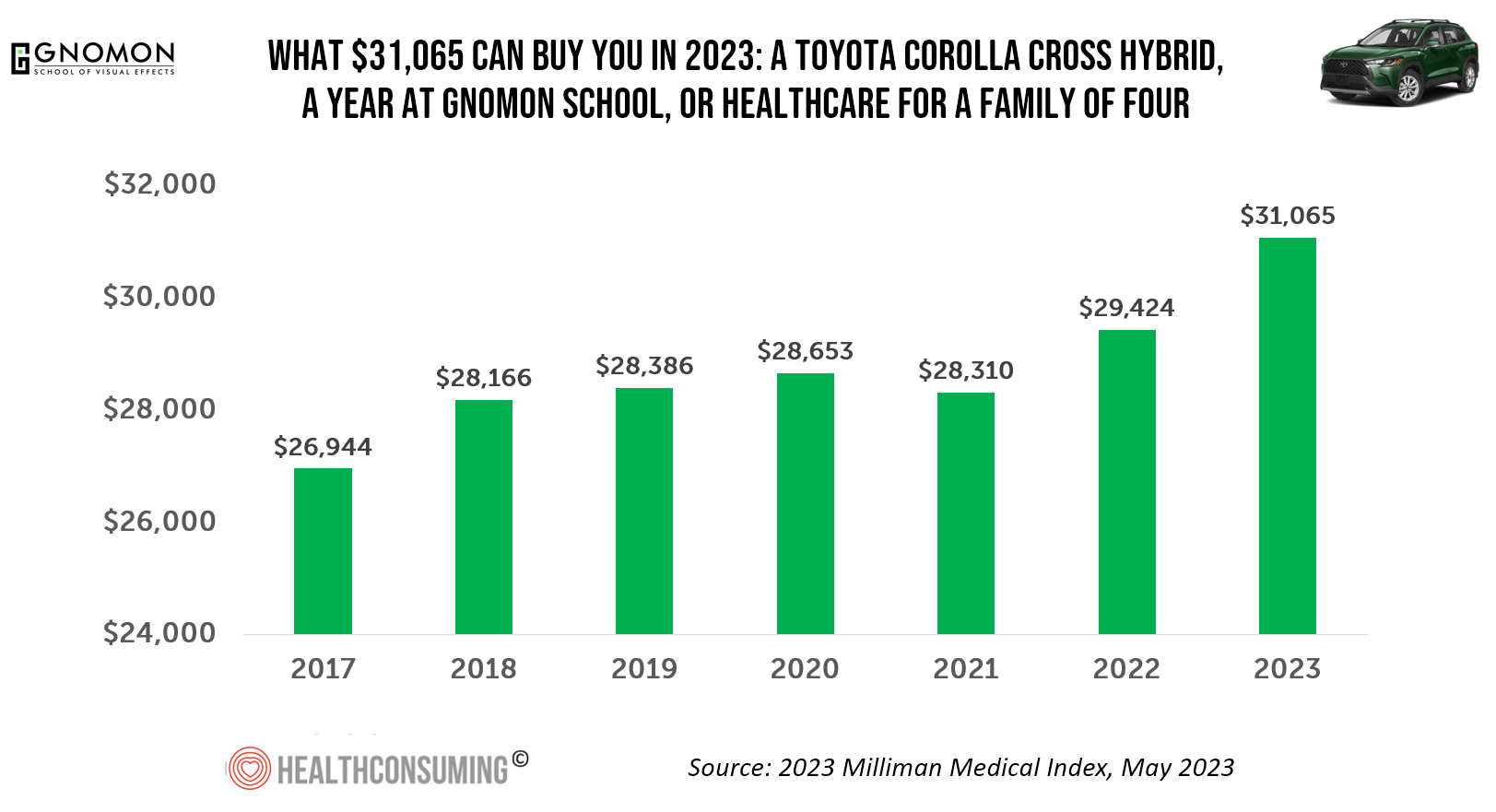
“Healthcare costs came roaring back in 2021” after falling in 2020. In 2023, that roaring growth in health care costs continues with expected growth of 5.6%. For 2023, you could take your $31K+ and buy a Toyota Corolla Cross Hybrid auto, fund a year at the Gnomon School in Hollywood toward a degree in animation or game design, or buy healthcare for your family of 4. Welcome to this year’s annual look at health care costs for a “typical” U.S. family explained in the 2023 Milliman Medical Index (MMI).
The Growing Pet Economy – What It Means for Human Health, Well-Being, and Healthcare Costs

Our pets can be personal and family drivers of health and health care cost savings, according to a new study from according to a new report from researchers at George Mason University published in their paper, Health Care Cost Savings of Pet Ownership. Reviewing this new paper inspired me to explore the current state of the pet/health market and implications for their human families, my weaving of various stories explored in this Health Populi blog post. Some of the key signposts we’ll cover are: The report on pet ownership driving owners’ health care cost savings A new market analysis of
A Public Health Wake-Up Call: Reading Between the Lines in IQVIA’s 2023 Use of Medicines Report
Reviewing the annual 2023 report from the IQVIA Institute for Human Data Science discussing The Use of Medicines in the U.S. is always a detailed, deep, and insightful dive into the state of prescription drugs. It’s a volume speaking volumes on the current picture of prescribed meds, spending and revenues, health care utilization trends, and a forecast looking out to 2027. In my read of this year’s review, I see a flashing light for U.S. health care: “Wake up, public health!” I’ve pulled out a few of the data points that speak to me about population health, prevention and early
We Are All Health Consumers Now – Toluna’s Latest Look at Consumers’ Health & Well-Being
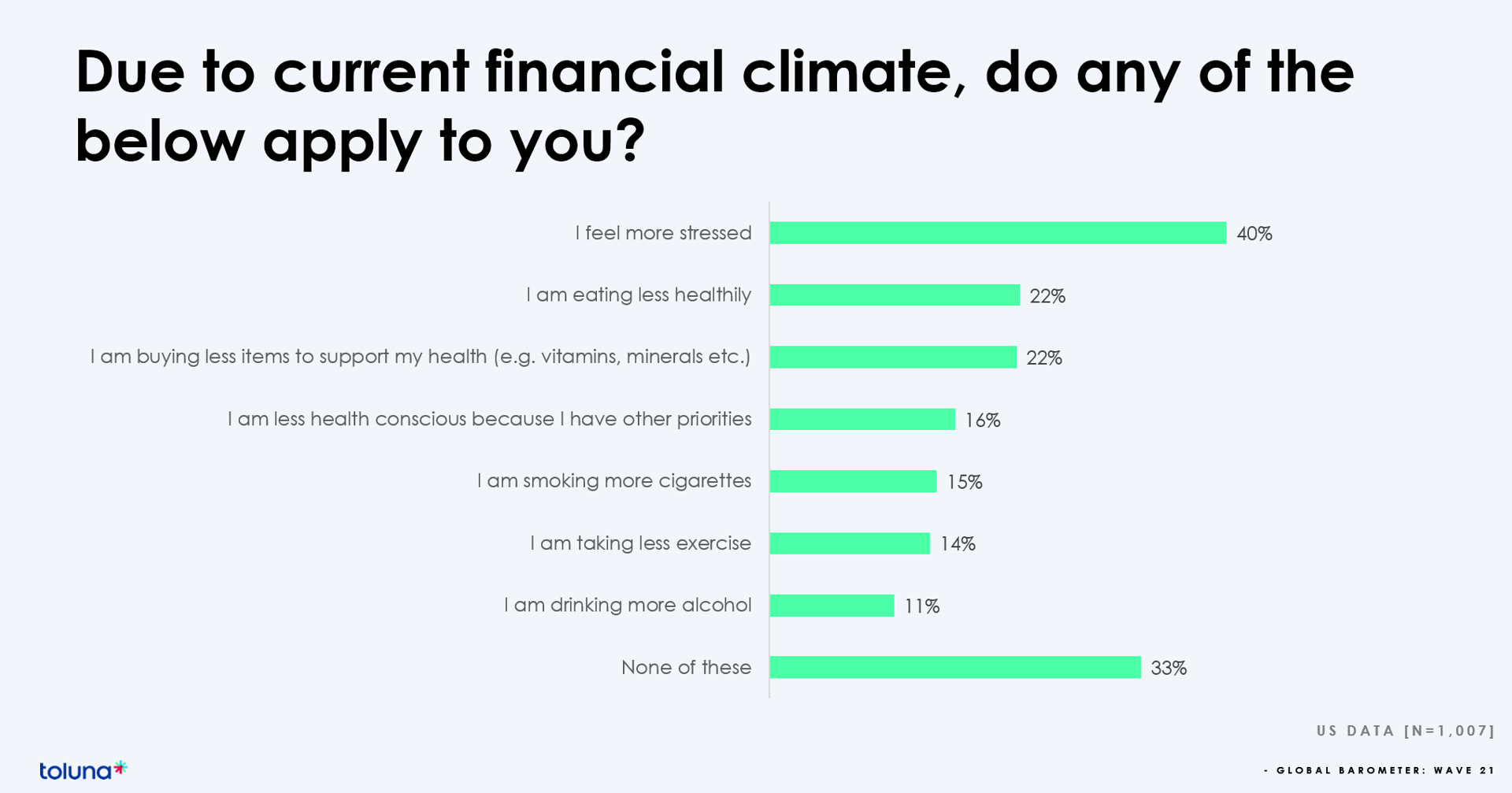
The challenging financial climate at the start of 2023 is impacting how people, globally, are perceiving, managing, and spending money on health and well-being, based on the latest (Wave 21) Global Consumer Barometer survey conducted by Toluna, a sister company of Harris Interactive. Globally, one-third of health citizens the world over are confronting greater stress levels due to the higher cost of living in their daily lives. One in two people say that rising cost of living is negatively impacting their health and well-being. On the positive side, one in three people believe
When Household Economics Blur with Health, Technology and Trust – Health Populi’s 2023 TrendCast

People are sick of being sick, the New York Times tells us. “Which virus is it?” the title of the article updating the winter 2022-23 sick-season asked. Entering 2023, U.S. health citizens face physical, financial, and mental health challenges of a syndemic, inflation, and stress – all of which will shape peoples’ demand side for health care and digital technology, and a supply side of providers challenged by tech-enabled organizations with design and data chops. Start with pandemic ennui The universal state of well-being among us mere humans is pandemic ennui: call it languishing (as opposed to flourishing), burnout, or
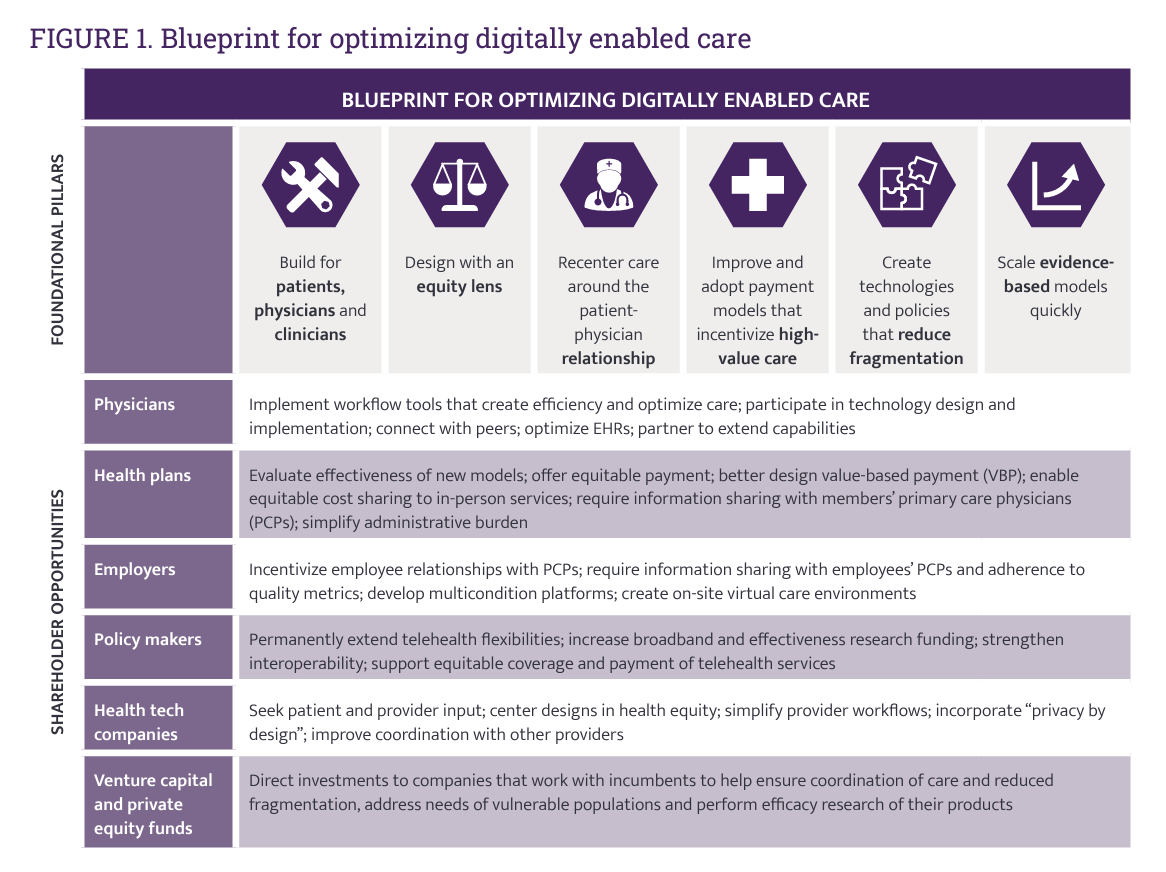
Omnichannel, Hybrid Health Care Is Happening – Let’s Bake It with Access and Equity
In just the past few months, we’ve seen the launch of Amazon Care, Instacart adding medical deliveries, and The Villages senior community welcoming virtual care to their homes. Welcome to the growing ecosystem of hybrid health care, anywhere and everywhere. In my latest post on the Medecision portal, I discuss the phenomenon and examples of early models, focusing in on Evernorth, a Cigna company. As we add new so-called “digital front doors” to health care delivery, we should be mindful to design in access and equity and avoid further fragmentation of an already-fragmented
Men Work in Retirement for Healthy Aging; Women, for the Money – Transamerica Looks at Retirement in 2022
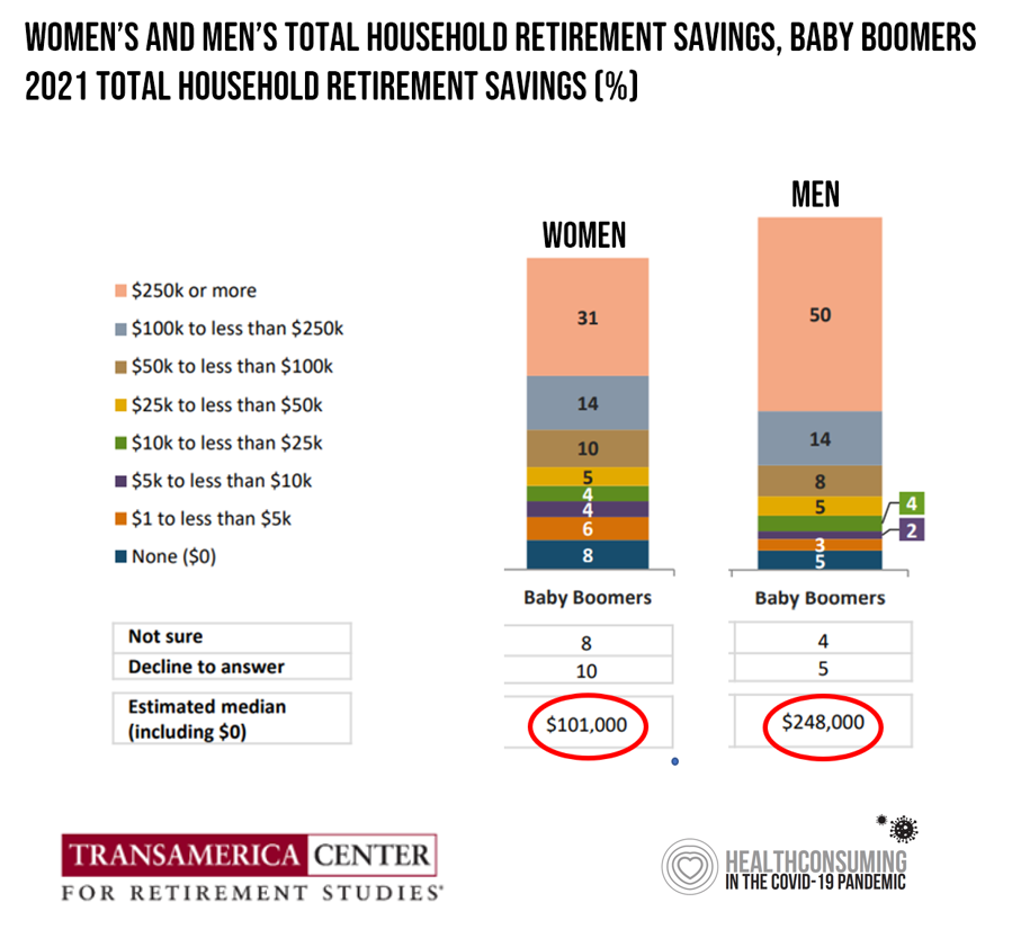
Due to gender pay gaps, time away from the workforce for raising children and caring for loved ones, women in the U.S. face a risky retirement outlook according to Emerging from the COVID-19 Pandemic: Women’s Health, Money, and Retirement Preparations from the Transamerica Center for Retirement Studies (TCRS). As Transamerica TCRS sums up the top-line, “Societal headwinds are undermining women’s retirement security.” Simply said, by the time a woman is looking to retire, she has saved less than one-half of the money her male counterpart has put away for aging after work-life. The
Consumers Rank Healthcare Experiences in the Bottom-Third of All Industries – the ACSI 2021-2022 Index
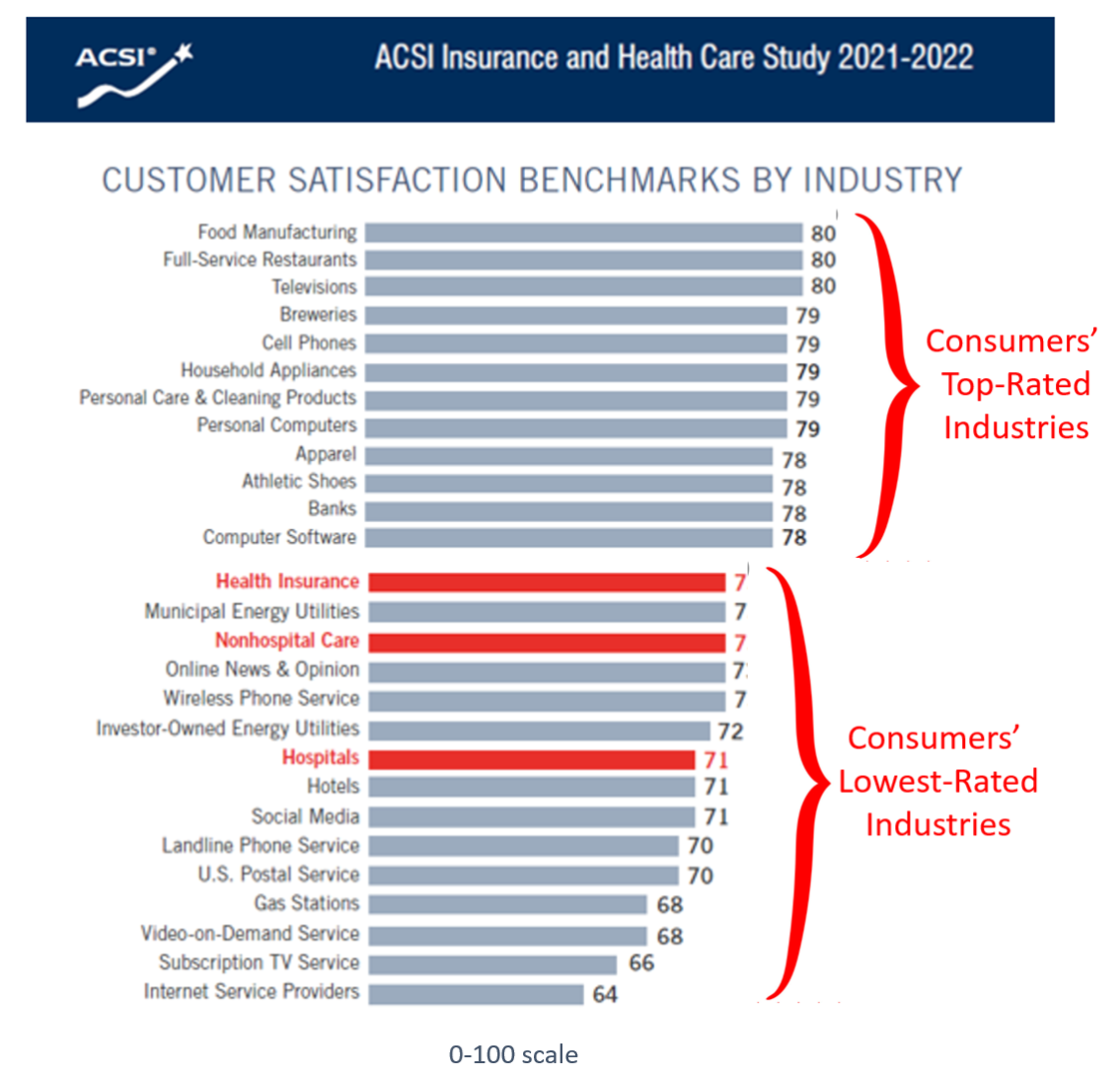
While consumers’ satisfaction with inpatient care experiences improved a few points over the past year, health insurance and hospitals still fall in the bottom-third of all industries with which people interact, according to the American Customer Satisfaction Index (ACSI) Insurance and Health Care Study 2021-2022. “With visitor restrictions relaxing and more elective procedures going forward, hospitals are slowly coming out of a COVID-induced satisfaction slump,” the study press released quoted Forrest Morgeson, Assistant Professor of Marketing at Michigan State University. This year’s ACSI Insurance and Health Care Index was developed through 12,840 consumer interviews
$22,463 Can Get You a Year of College in Connecticut, a Round of Ref Work in the Stanley Cup Playoffs, or Health Benefits for a Worker’s Family
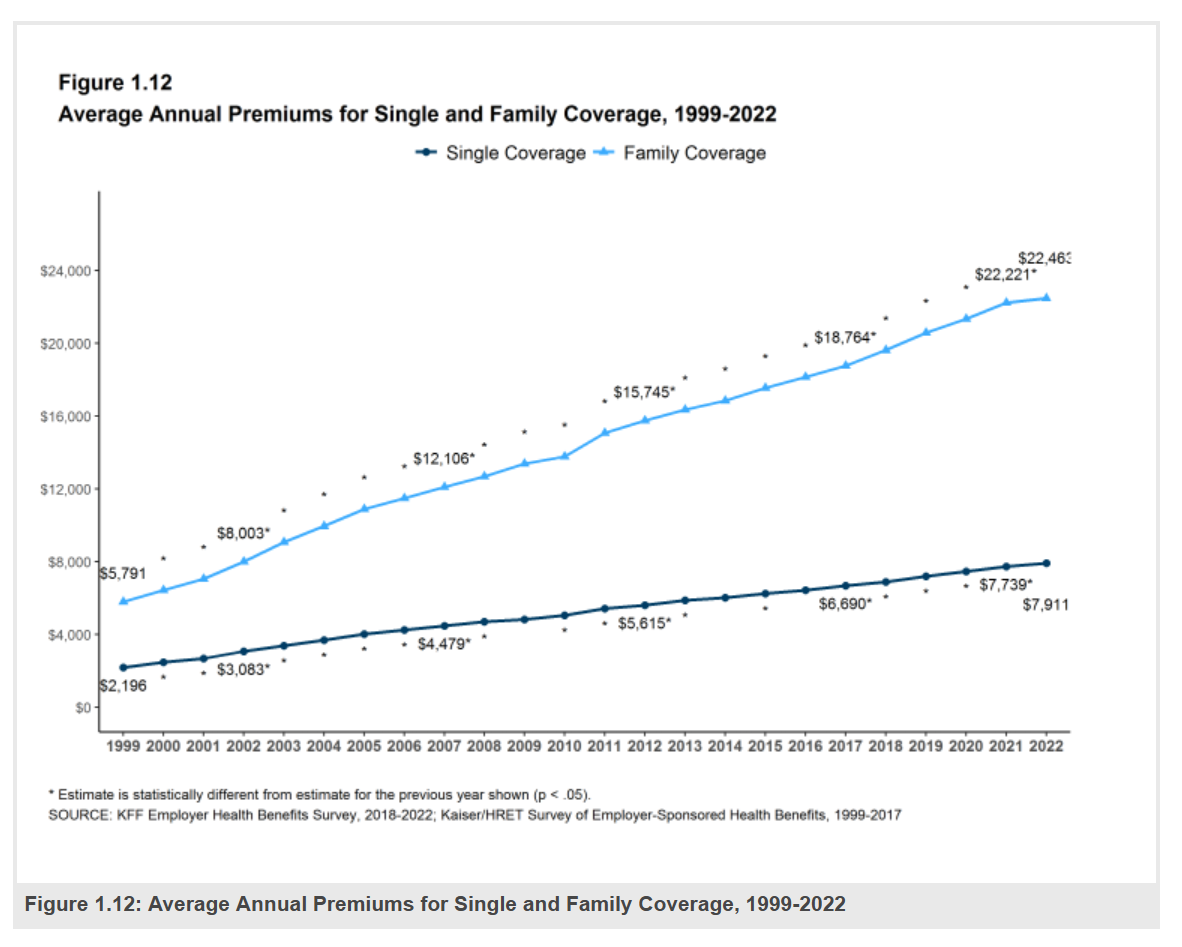
Employers covering health insurance for workers’ families will face insurance premiums reaching, on average, $22,463. That is roughly what a year at an independent college in Connecticut would cost, or a round of pay for a ref in the Stanley Cup playoffs. With that sticker-shock level of health plan costs, welcome to the 2022 Employer Health Benefits Survey from Kaiser Family Foundation, KFF’s annual study of employer-sponsored health care. Each year, KFF assembles data we use all year long for strategic and tactical planning in U.S. health care. This mega-study looks at
Consumers’ and the White House’s Growing Focus on Food and Nutrition
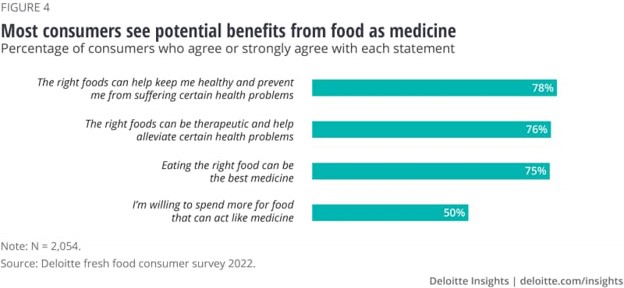
Today, the White House is convening a Conference on Hunger, Nutrition and Health. So it’s a propitious time to weave together some of the latest research and insights into food-as-medicine and a key determinant of health and well-being. This is the first White House conference focused on nutrition and food in over 50 years. The National Strategy was released today, and covers a range of programs that bake health and nutrition into Federal policies going beyond “food” itself: we see various determinants of health embedded into the Strategy, such as supporting physical activity,
The Patient As the Payer: Self-Pay, Bad Debt, and the Erosion of Hospital Finances
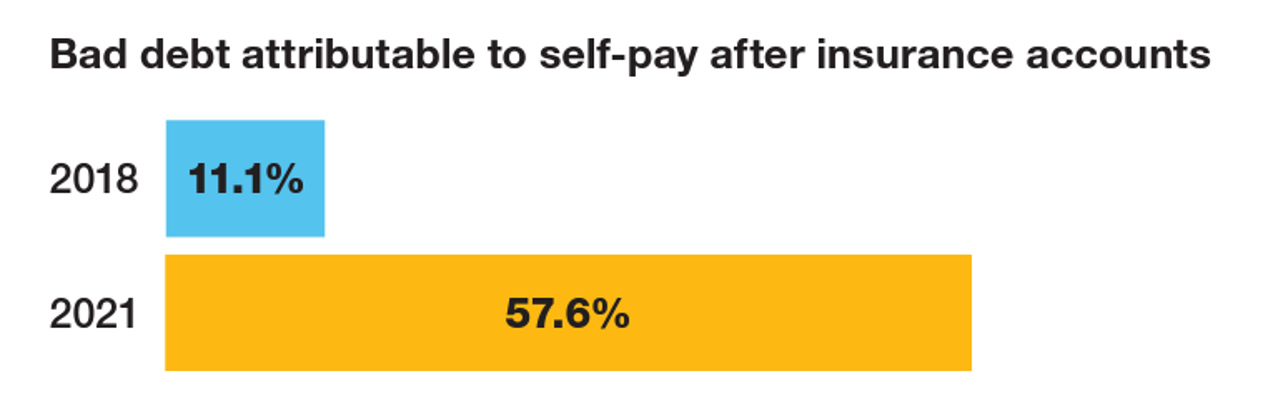
“The odds are against hospitals collecting patient balances greater than $7,500,” the report analyzing Hospital collection rates for self-pay patient accounts from Crowe concludes. Crowe benchmarked data from 1,600 hospitals and over 100,00 physicians in the U.S. to reveal trends on health care providers’ ability to collect patient service revenue. And bad debt — write-offs that come out of uncollected patient bill balances after “significant collection efforts” by hospitals and doctors — is challenging their already-thin or negative financial margins. The first chart quantifies that bad debt attributable to patients’ self-pay payments
The More Chronic Conditions, the More Likely a Patient Will Have Medical Debt
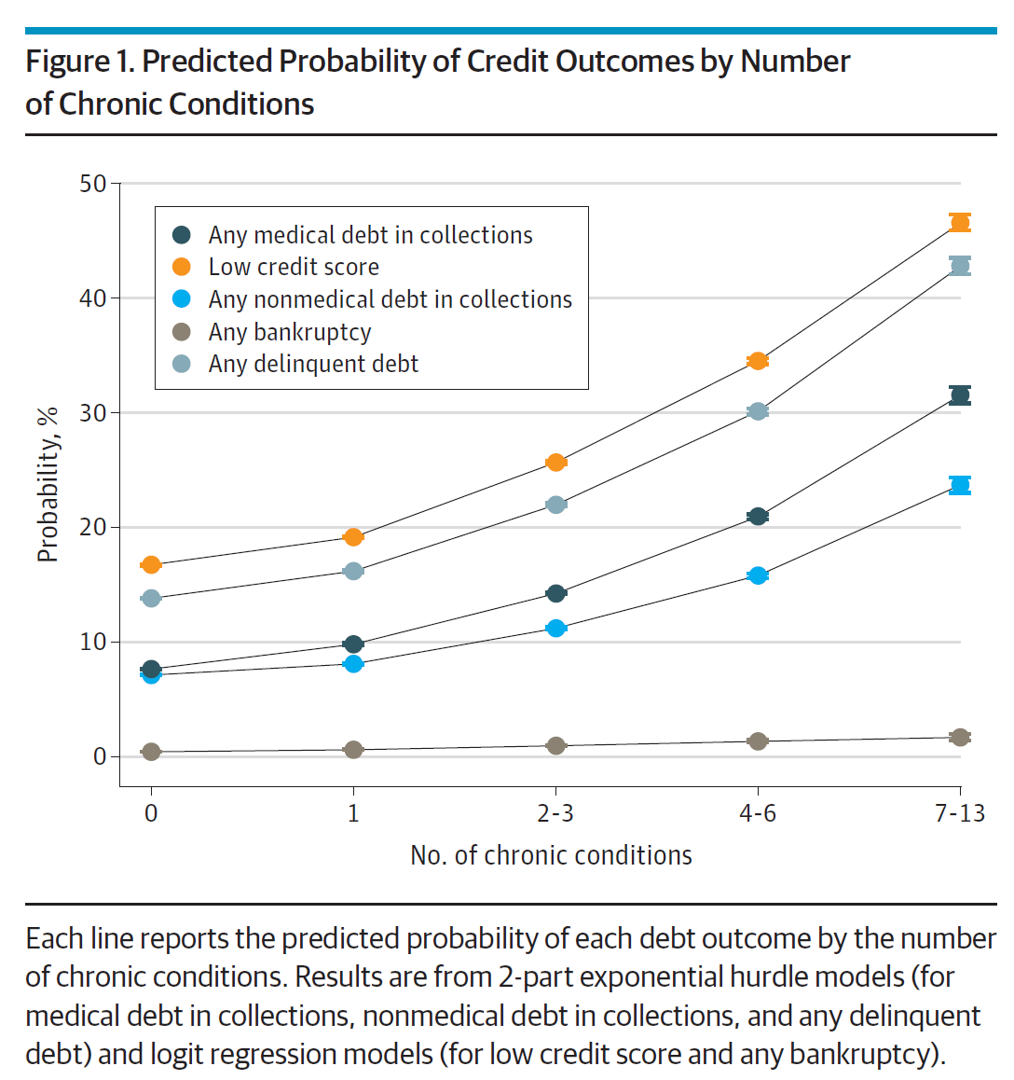
There is a direct association between a person’s health status and patient outcomes and their financial health, quantified in original research published this week in JAMA Internal Medicine. Researchers from the University of Michigan (my alma mater) Medical School and Institute for Healthcare Policy and Innovation analyzed two years of commercial insurance claims data generated between January 2019 and January 2021, linking to commercial credit data from January 2021 for patients enrolled in a preferred providers organization in Michigan. The first chart illustrates the predicted probability of credit outcomes based on the
Gas ‘N Healthcare – How Transportation Links to Health Care Access and Financial Health
Some patients dealing with cancer at Mercy Health’s Lourdes Hospital have been supplied with gas cards. This gesture is enabling families to get to medical appointments around Paducah, Kentucky where, this week, car drivers faced regular gas priced at an average of $4.16 a gallon compared with $2.92 one year ago. Here’s the Hospital’s Facebook page featuring their gratitude to FiveStar Food Mart, the American Cancer Society, and the Mercy Health Foundation. “By providing cancer patients with gas cards, the cancer care team at Mercy Health Lourdes Hospital in Paducah hopes to mitigate financial challenges
Changing Views of Retirement and Health Post-COVID: Transamerica’s Look At Workers’ Disrupted Futures
As more than 1 in 3 U.S. workers were unemployed during the pandemic and another 38% had reductions in hours and pay, Americans’ personal forecasts and expectations for retirement have been disrupted and dislocated. In its look at The Road Ahead: Addressing Pandemic-Related Setbacks and Strengthening the U.S. Retirement System from the Tramsamerica Center for Retirement Studies (TCRS), we learn about the changing views of U.S. workers on their future work, income, savings, dreams and fears. Since 1988, TCRS has assessed workers’ perspectives on their futures, this year segmented the 10,003 adults
Use of Preventive Health Services Declined Among Commercially Insured People – With Big Differences in Telehealth for Non-White People, Castlight Finds
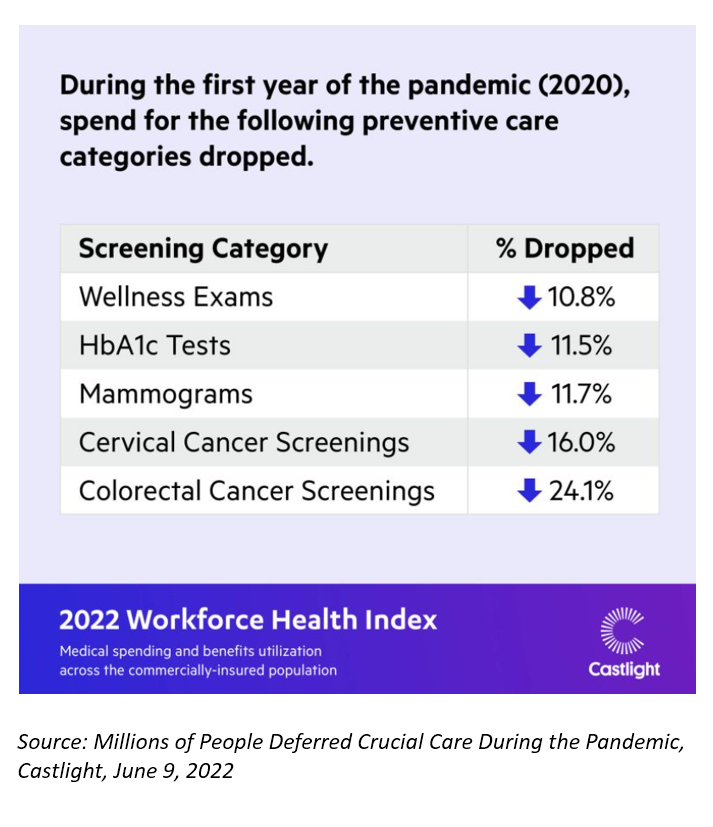
Declines in preventive care services like cancer screenings and blood glucose testing concern employers, whose continued to cover health insurance for employees during the pandemic. “As we enter the third year of the COVID-19 pandemic, employers continue to battle escalating clinical issues, including delayed care for chronic conditions, postponed preventive screenings, and the exponential increase in demand for behavioral health services,” the Chief Medical Officer for Castlight Health notes in an analysis of medical claims titled Millions of People Deferred Crucial Care During the Pandemic, published in June. The
A New Chevy Equinox SUV, a Year in Grad School, or Health Care for Four – The 2022 Milliman Medical Index
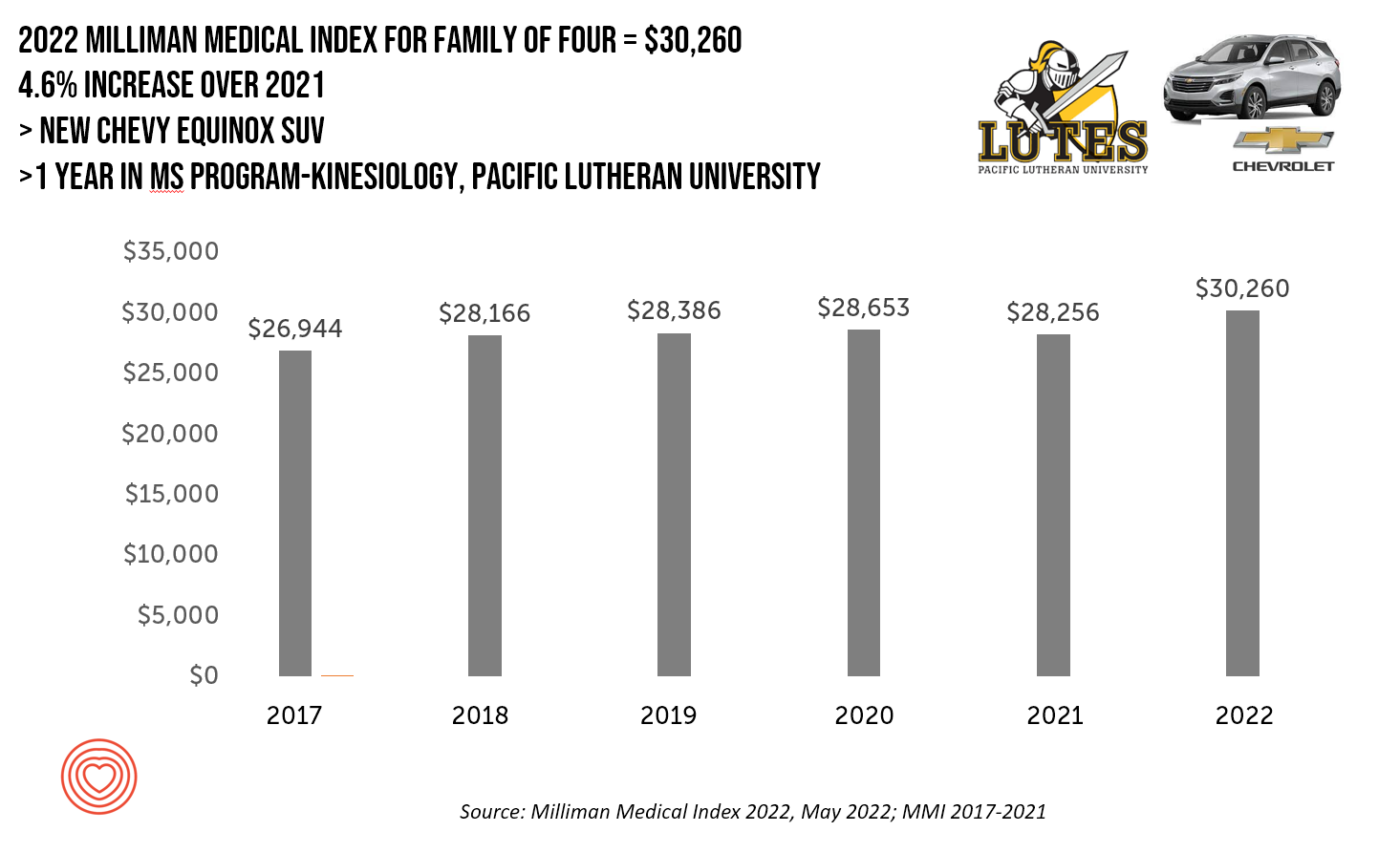
A new Chevy Equinox SUV, a year in an MS program in kinesiology at Pacific Lutheran U., or health care for a family of four. At $30,260, you could pick one of these three options. Welcome to this year’s 2022 Milliman Medical Index, which annually calculates the health care costs for a median family of 4 in the U.S. I perennially select two alternative purchases for you to consider aligning with the MMI medical index. I have often picked a new car at list price and a year’s tuition at a U.S. institution of
The Patient as Consumer and Payer – A Focus on Financial Stress and Wellbeing
Year 3 into the COVID-19 pandemic, health citizens are dealing with coronavirus variants in convergence with other challenges in daily life: price inflation, civil and social stress, anxiety and depression, global security concerns, and the safety of their families. Add on top of these significant stressors the need to deal with medical bills, which is another source of stress for millions of patients in America. I appreciated the opportunity to share my perspectives on “The Patient As the Payer: How the Pandemic, Inflation, and Anxiety are Reshaping Consumers” in a webinar hosted by CarePayment on 25 May 2022. In this
How Business Can Bolster Determinants of Health: The Marmot Review for Industry

“Until now, focus on….the social determinants of health has been for government and civil society. The private sector has not been involved in the discussion or, worse, has been seen as part of the problem. It is time this changed,” asserts the report, The Business of Health Equity: The Marmot Review for Industry, sponsored by Legal & General in collaboration with University College London (UCL) Institute of Health Equity, led by Sir Michael Marmot. Sir Michael has been researching and writing about social determinants of health and health equity for decades, culminating publications





 Thanks to Jennifer Castenson for
Thanks to Jennifer Castenson for  yeva, digital storyteller, for engaging in
yeva, digital storyteller, for engaging in  Jane joined host Dr. Geeta "Dr. G" Nayyar and colleagues to brainstorm the value of vaccines for public and individual health in this challenging environment for health literacy, health politics, and health citizen grievance.
Jane joined host Dr. Geeta "Dr. G" Nayyar and colleagues to brainstorm the value of vaccines for public and individual health in this challenging environment for health literacy, health politics, and health citizen grievance.