With consumer and prescriber interest in GLP-1 receptor agonist drugs “soaring,” health plan managers have a new source of financial stress and clinical questions on their to-do list.
A team of Virta Health leaders held a webinar on 13th July 2023 to explain the results of a study the company just completed assessing health plan execs’ current views on Ozempic and other GLP-1 medicines with a view on both clinical outcomes and cost implications for this growing category of drugs that address diabetes and obesity.
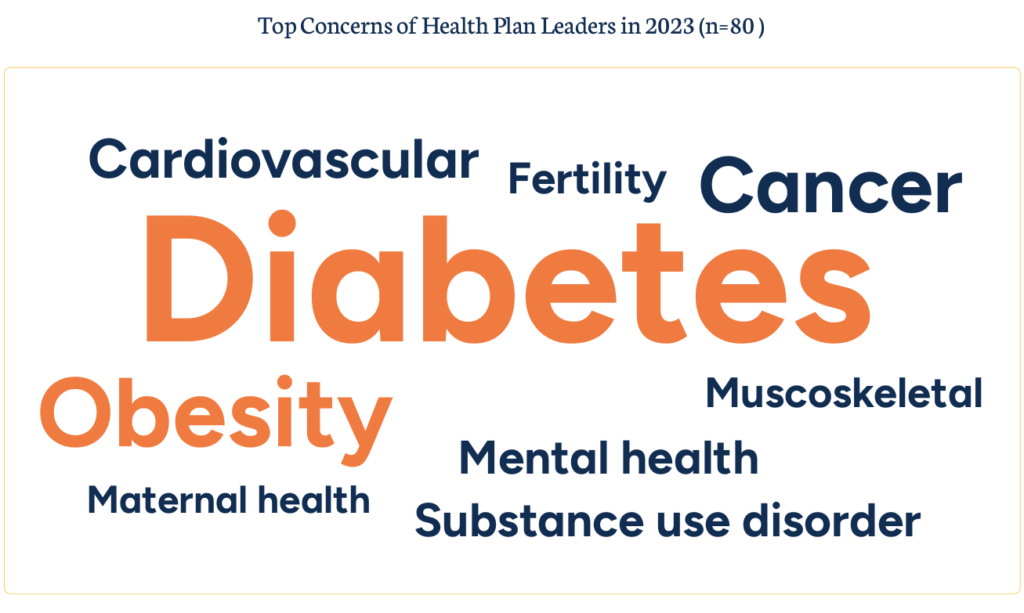
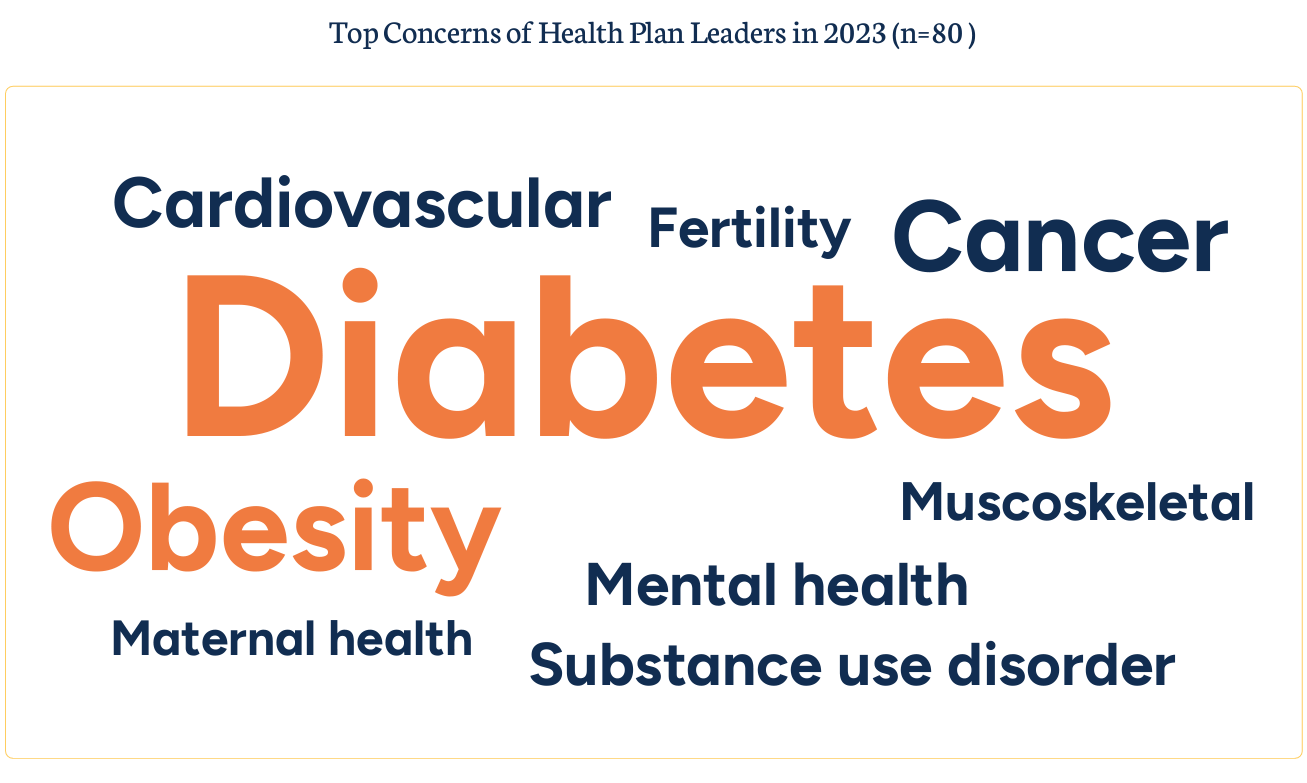
Indeed, diabetes and obesity are top health concerns among the 80 health plan executives that Virta Health surveyed by phone in March and April 2023. You can see other top condition concerns shown in the word cloud diagram here, included in the study report.
Why diabetes and obesity? Because of rising costs and the conditions downstream health impacts, Virta noted in the report.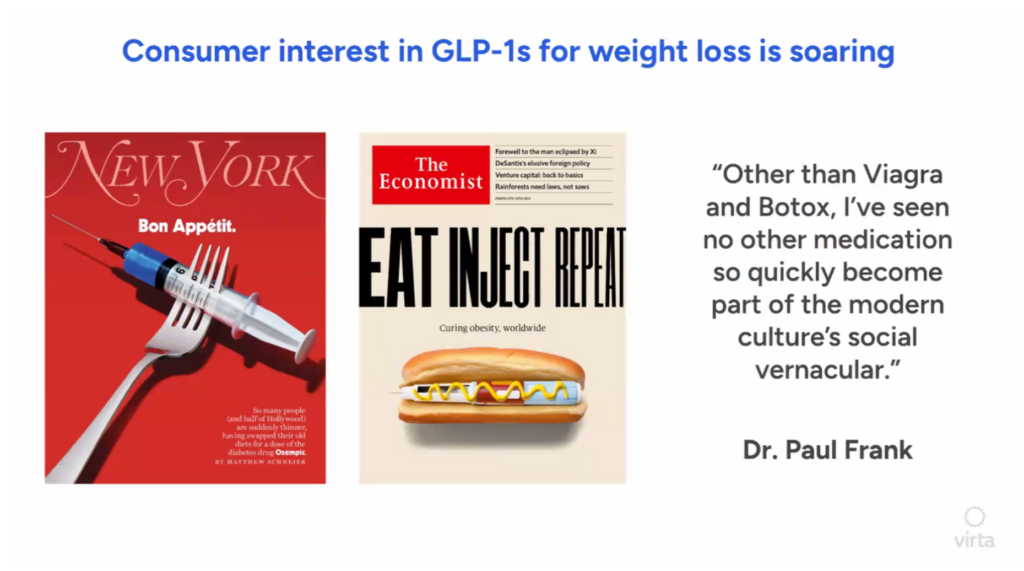
All health plan leaders interviewed were worried about the growth of GLP-1 meds for both clinical indications, with the surge in uptake “overwhelming” health plans’ ability to manage cost, the study observed.
The hockey-stick growth in adoption and media coverage of these new medicines has taken hold in popular culture: Dr. Paul Frank was quoted, saying that,
“Other than Viagra and Botox, I’ve seen no other medications so quickly become part of the modern culture’s social vernacular.” That quote is shown here with two magazine covers that punctuate the point Dr. Frank is making.
[An interesting sidebar FYI: Dr. Frank, a dermatologist, coined the phrase “Ozempic Face” as a side effect he observed in some of his patients who were experiencing a form of sagging or aging skin as a result of using the drug].
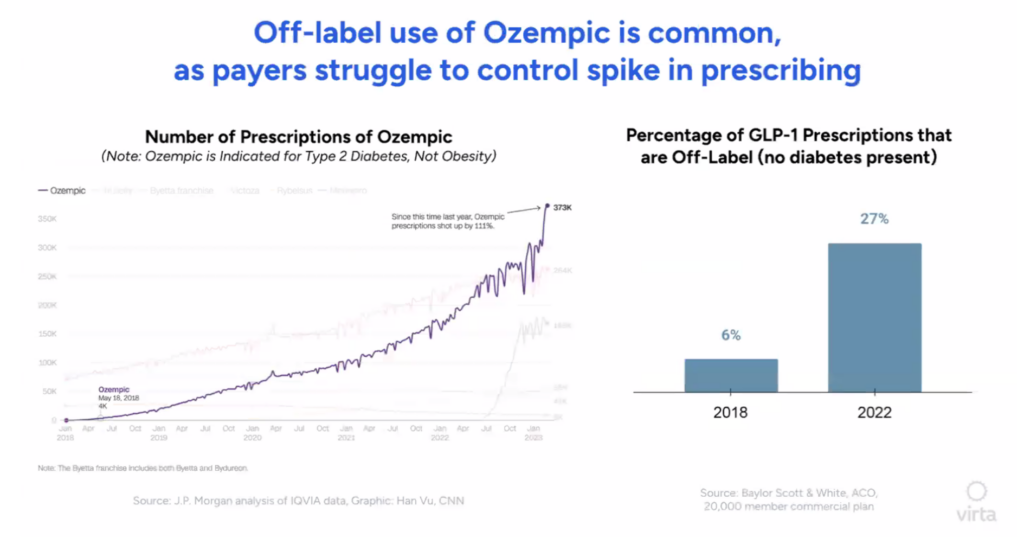
With the motivation to “Eat, Inject, and Repeat” that The Economist described in its cover story from 2nd March 2023, the story talks about the fast market growth of the GLP-1’s as shown in the line chart here, with the forecasted market for these drugs reaching $150bn by 2031 — about the market for today’s cancer therapies.
“Some think they could become as common as beta blockers or statins,” The Economist tells us.
With that bullish forecast comes the sobering health economics of the scenario. “The price rivals a mortgage payment,” Dr. Adam Wolfberg, Virta’s Chief Medical Officer, emphasized on the webcast.

To Dr. Wolfberg’s point, Virta calculated that for payors, GLP-1 costs could be “enormous” — to the tune of an additional $60 per member/per month based on assumptions in analysts’ forecasts.
In aggregate based on 100,000 covered lives in a plan, that would calculate to an additional $72 million in payor cost.
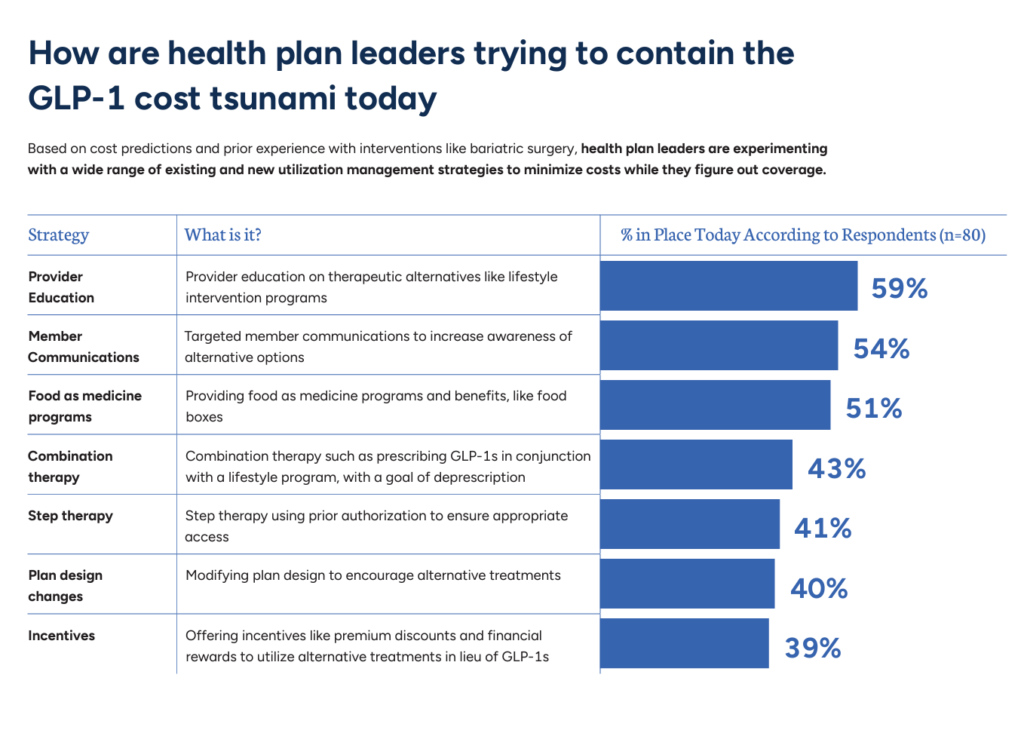
So then, how might health plan leaders deal with what Virta terms the GLP-1 cost tsunami?
The bar chart identifies the most common strategies health plans are deploying to contain the costs of GLP-1 drugs.
Start with provider education, when health plans focus efforts on updating prescribers’ knowledge of alternatives to the GLP-1 drugs — such as lifestyle programs. Provider education is used by 3 in 5 plans today.
Second, over over-half of health plans focus on member communications, informing health plan enrollees on alternative options to the expensive drugs.
In third place, one-half of health plans are prescribing food-as-medicine, which increasingly consumers are also keen to use for a variety of conditions — like heart disease, gut issues, and general energy and well-being.
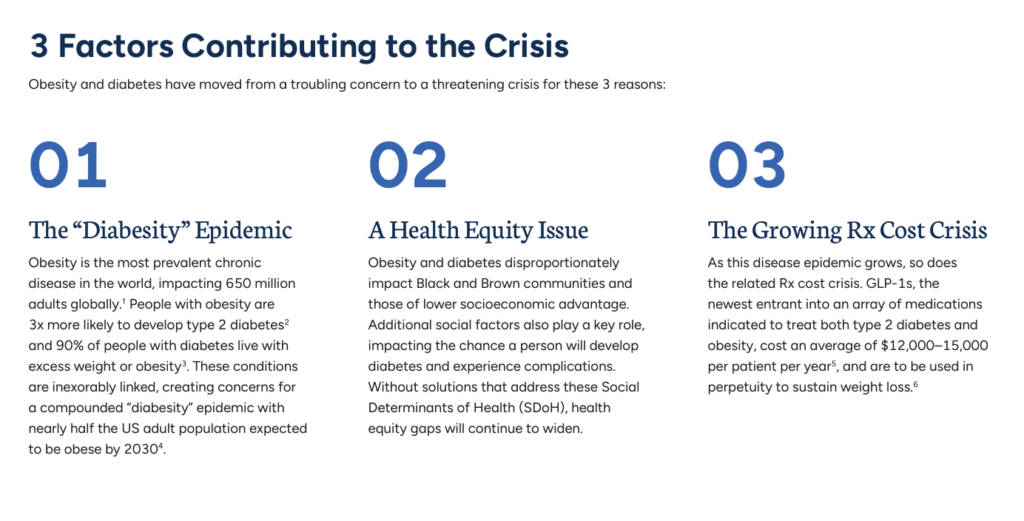
Health Populi’s Hot Points: The combined public health crisis of diabetes and obesity is associated with three converging driving forces:
- A diabesity epidemic, the actual convergence of the two conditions which is expected to impact nearly one-half of the U.S. adult population by 2030
- Health equity challenges, where diabetes and obesity disproportionately impact Black and Brown people living int he U.S. — largely caused by the risks of social determinants of health, from food security and healthy food availability to neighborhoods safe to play and be active outside along with access to primary care, as well as other factors.
- A growing prescription drug cost crisis, where in the case of the GLP-1s involve on average $12,000 to $15,000 per-patient per-year.
And this current generation of GLP-1 medicines is required to be taken for life….year after year for a lifetime….which compounds the cost over hundreds of thousands of patients for dozens of years.
Ken Mishler, formerly the Chief Pharmacist of Blue Cross and Blue Shield of Kansas, is quoted in the Virta report asserted that,
“This is a long game. Without lifestyle intervention, none of these drugs….will work to help you improve overall cost and quality.”
Here, “You” is both the health plan and the patient, each facing their respective unsustainable scenario for managing diabetes and obesity in an era when folks are looking for an easy fix, the miracle-in-a-pill-bottle or hypodermic hit.
For both patients and health plans, the drugs alone are an unsustainable model in terms of financial toxicity, whether we are talking about a patient-as-payor’s wallet for $12K+ a year, or to the health plan’s bottom-line and per-member/per-month medical trend spending.
This “long game” means lifestyle education and the ongoing bolstering of behavior change, which is bloody hard — but do-able — if we employ smart, clever, insightful design teams who deeply understand what’s underneath patients’ lives and daily choices. The rule of that long game have to do with enchanting and knowing design, empathy for patients and their families, and commitment to doing the right thing this year, even if a plan member might move on to a new job and health plan or be a difficult customer with a history of non-adherence. Meet folks where they are…with empathy and understanding and incredibly clever tools, delightful meal kits, and wondrous wearable technologies that engage people in wanting to own their health.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.