As Adult Vaccination Levels Fall, We Must Assert the Value of Vaccines
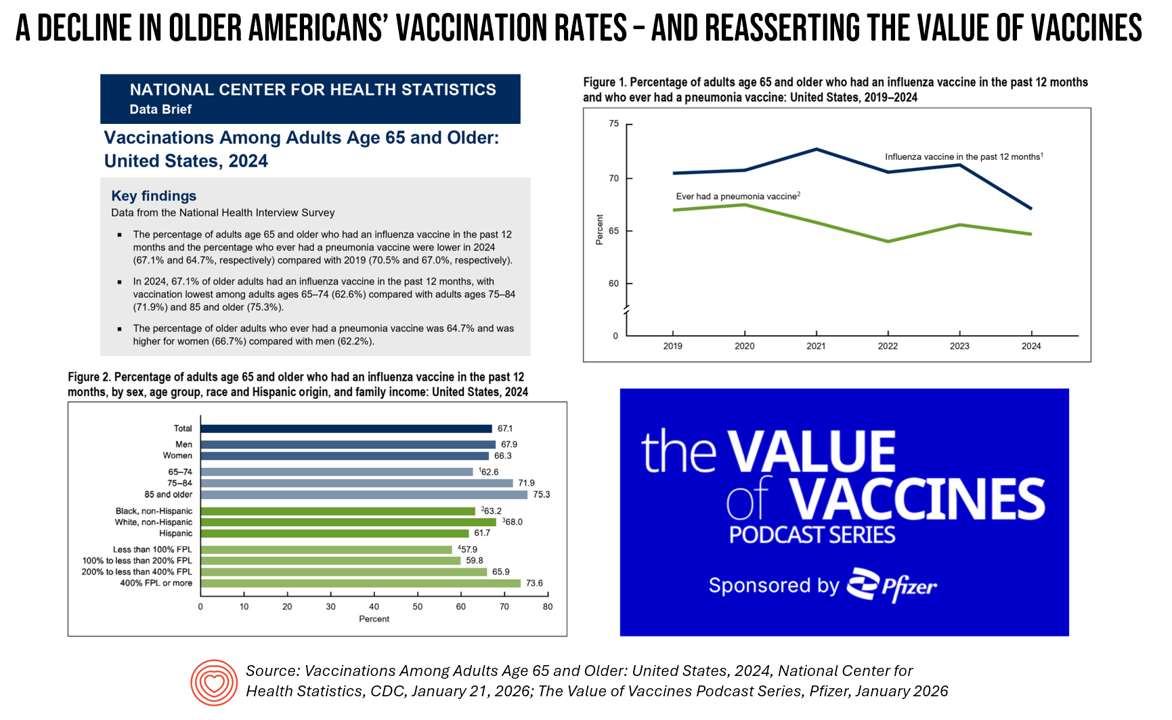
The rate of vaccinations among people 65 years of age and older has declined since 2019 — a personal health challenge for aging Americans and their caregivers and families, and a public health problem for the U.S. The Centers for Disease Control’s National Center for Health Statistics published Data Brief 547 on the situation on January 21, 2026. In the meantime, serendipity and timing are uncanny in the moment as The Value of Vaccines conversation series from Pfizer was launched this week. I am grateful to have participated in this project with several sisters-in-expertise: Elif Alyanak from Avalere, Venesa Day
Dr. Osterholm Explains “The Big One” – A Deja Vu Moment with a True North Public Health Expert
“The truism that no one is completely safe until everyone is safe is a truism because it happens to be true.” So caution Michael Osterholm, epidemiologist, professor at the University of Minnesota School of Public Health, and director of CIDRAP (the Center for Infectious Disease Research and Policy at the U-MN) and collaborating writer Mark Olshaker in their new book, The Big One. (In this post, for the sake of brevity, I’ll refer to the two authors as “O&O”). Simply put, the tagline tells us what we are about to read: a
Expect Double-Digit Prescription Drug Trend Increases in 2026 – The Update from HUB International
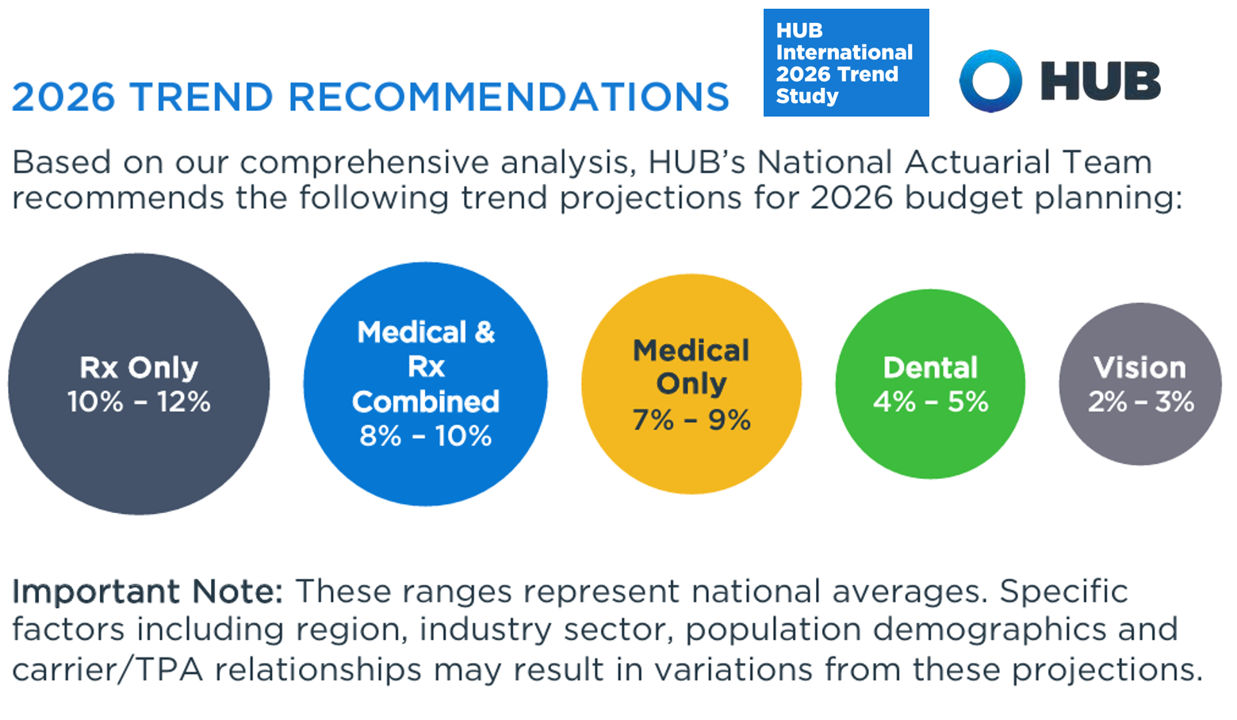
Prescription drug price trend for 2026 will be between 10% and 12% according to the 2026 Trend Study from HUB International, a global insurance and financial services firm. Here’s HUB’s line chart of the combined medical and Rx trend, illustrating nearly double trend growth since 2022 following the peak of 10.1% (combined) in 201 as patients returned to health care services and encounters when feeling safe in the fading out of the COVID-19 pandemic. That precipitous low-point in 2022 of 3.4% was the peak of the coronavirus stay-at-home period, representing the “medical distancing” felt across
The Patient as Consumer – Updates from Fidelity on Retiree Health Care Costs ($172,500), Delaying Care, Tariff Impacts on Spending, and Roche Going DTPatient for Rx’s?

As of August 2025, U.S. patients of all demographics and geographies face many uncertainties with respect to their care. Issues such as health plan coverage, prescription drug costs, and access to services, among other challenges, continue to re-shape patients-as-health-consumers seeking transparency, clinical choices, and trust-worthy relationships with touchpoints in their personal health ecosystems. Four just-breaking stories across the health/care ecosystem illustrate several of these uncertainties and forces in U.S. health care — some adding friction and angst in a patient’s life, others perhaps providing some relief for certain health consumers. These news items address health care costs in retirement, the
What Children Can Teach Us About Using GenAI – Insights from The Alan Turing Institute and LEGO

“While children are the group that may be most impacted by the widespread deployment of generative AI, they are simultaneously the group least represented in decision-making processes relating to the design, development, deployment or governance of AI,” we learn in Understanding the Impacts of Generative AI Use on Children, research conducted by The Alan Turing Institute in partnership with the LEGO Group. But it’s the children who shared their perspectives who can teach adults about some potential positive and negative aspects of GenAI, and help inform us in managing downside risks. FYI, The Institute is headquartered in the British Library
Consumers Are Keen to Invest in Health and Well-Being – But Show Them the Evidence

Consumers around the world feel more invested than ever in what makes people feel both well and prosperous, we learn in the NielsenIQ Global State of Health & Wellness 2025 survey report. But there’s a trust deficit that must be healed in order for a health consumer to invest in services and products that feed health and well-being. NIQ fielded the survey research online in January and February 2025 among nearly 19,000 adults living in 19 countries: Brazil, Canada, China, the Czech Republic, France, Germany, Hungary, India, Indonesia Italy, Mexico, Netherlands, Poland, South Africa, Spain, Turkiye, UAE, United Kingdom, and
U.S. Health Care in 2025 Requires Scenario Planning: The Uncertainties (AI!?) That Inspire DIY Healthcare

As Weight Watchers prepares to initiate bankruptcy proceedings, I file the news event under “thinking the unthinkable.” “Thinking about the unthinkable” is what Herman Kahn, a father of scenario planning, asked us to do when he pioneered the process. In this book, for Kahn, “the unthinkable” was thermonuclear war, and the year was 1962. The book was tag-lined as “must reading for an informed public” and in it, Kahn I’ve been drawn back to this book lately because of a more intense workflow using
From Bowling Alone to Eating Alone – What the Shift to Take-Out Food Means for Our Social Well-Being and Mental Health
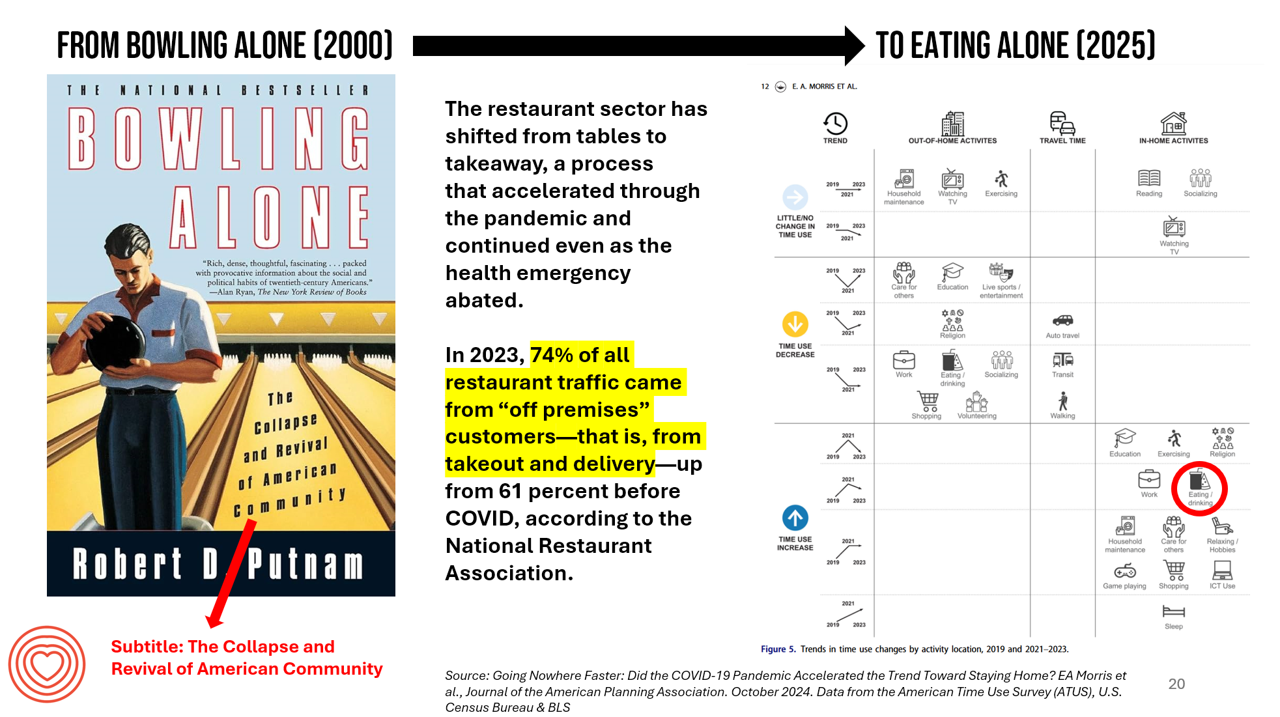
New data from the American Time Use Survey, research conducted by the U.S. Census Bureau and the Bureau of Labor Statistics, shows that Americans now favor eating in-home compared with eating out at restaurants. Corroborating this shift is other data from the National Restaurant Association sharing that 74% of all restaurant traffic in 2023 came from “off premises” customers — that is, from takeout and delivery — up from 61% in the pre-COVID era. What does this mean for our health, well-being, and sense of community and connectivity? I’m preparing a new talk to
One Way to Improve U.S. Healthcare, Lower Costs and Drive Outcomes? “Unvendor,” Asserts Dr. Harm Scherpbier in His New Book

Health information technology professionals charged with selecting, implementing, updating, and paying for health IT in hospital and care delivery settings are essentially the first-line “consumers” of health IT – specifically, electronic health records. But these health IT leaders feel far from empowered and choiceful as consumers in todays EHR vendor “monoculture,” Harm Scherpbier, MD, explains in his book, Unvendor. I spent time with Harm to discuss the book, its backstory, and what he hopes to accomplish by raising the issue of single-vendor health IT and how clinicians, health IT staff, and
The New “Paging Dr. Google?” DTC-AI for Health Care

While most people in the U.S. who have used large language models (like ChatGPT) for informal learning, entertainment, and getting information about products and services, 39% of U.S. adults have also tapped into LLMs to source information about physical or mental health. This insight is brought to us in the brilliantly titled report, Close encounters of the AI kind, from the Imagining the Digital Future Center at Elon University. The principle author of the survey report is the Center’s Director, Lee Rainie, whose name many of you will know from his two+ decade career at the Pew Research Center (and
The Growth of DIY Digital Health – What’s Behind the Zeitgeist of Self-Reliance?
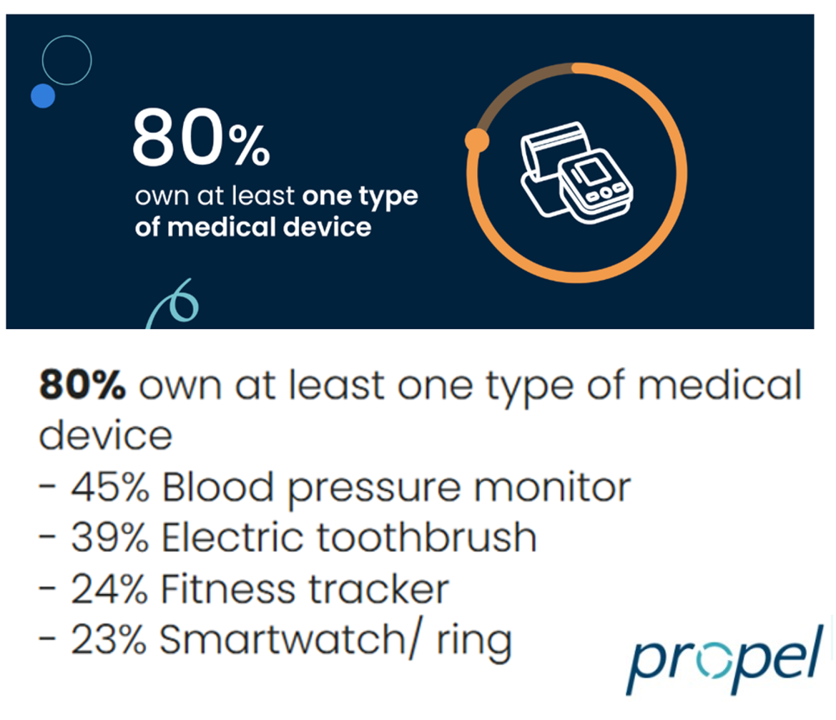
Most people in the U.S. use at least one medical device at home — likely a blood pressure monitor. used by nearly one-half of people based on a survey of 2,000 consumers conducted for Propel Software. The Propel study’s insights build on what we know is a growing ethos among health consumers seeking to take more control over their health care and the rising costs of medical bills and out-of-pocket expenses. That includes oral health and dental bills: 2 in 5 U.S. consumers use electric toothbrushes (a growing smart-device category at the
Trust and Grievance in 2025: The Edelman Trust Barometer on MLK Jr. Day Converging with the World Economic Forum Kick-Off and the Inauguration of the 47th U.S. President
At the start of each new year comes the World Economic Forum meet-up in Davos, Switzerland and with that conference start today, 20 January 2025, the publication of the Edelman Trust Barometer. Now in the study’s 25th annual edition, the Edelman Trust Barometer this year finds us, globally, in a Crisis of Grievance which is eroding trust. Edelman surveyed 1,150 residents (plus or minus) in each of 28 countries around the world, yielding over 33,000 citizens’ voices sharing perspectives on trust and institutions. Interviews were fielded from late October to mid-November 2024.
Peace and Health: A Causal Relationship Explored in the AMA Journal of Ethics
“Peace and health are inextricably connected,” the Editors of the AMA Journal of Ethics introduce an issue of the journal devoted to Peace in Health Care published November 2024. In this timely journal issue, we can explore nearly one dozen essays exploring the interrelationship between peace and health in various clinical, care, and community settings — including hospice, maternal/child care, built environments, and adjacencies looking at the use of psychedelics and music for quieting one’s inner voices. You, the reader, will find your own favorite issues to explore based on your work, values, and interests.
Health Information Security – My Interview with Richard Kaufmann, CISO of Amedisys – Part 1: Origin Stories, the Security Ecosystem, and the Start Line

“If data is everywhere, how do you protect it?” This thought has been on my mind well before the Change Healthcare hacks (that’s plural) with which U.S. health care stakeholders are still dealing as this post goes live on the Health Populi blog. It’s a question posed to me in conversation with Richard Kaufmann, Chief Information Security Officer (CISO) with Amedisys. I’m grateful for the opportunity to explore in depth the many facets of cybersecurity in health care with Richard – the growing threats, the impact on providers, the state of technology and innovations to manage risks, and his evolving
AI: Patients Included

“Clinical transformation with AI is easier without patients.” When Dr. Grace Cordovano heard this statement on a panel of physicians convening to share perspectives on the future of AI in health care held in early March 2024, the board-certified patient advocate felt, in her words, “insulted on behalf of the patient communities I know that are working tirelessly to advance AI that works for them.” “The healthcare ecosystem and policy landscape must formally recognize patients as end-users and co-creators of AI,” Cordovano wrote to me in an e-mail exchange. “Patients, their care partners, caregivers, and advocates are already utilizing AI
The Economic Contours of the Change Healthcare Cyber Attack: Taking Stock So Far

On February 22, 2024, I went to a CVS Pharmacy-Inside-Target in my community to fill a prescription for benzonatate 200 mg capsules. I had caught a bad case of the flu the week before, and subsequently suffered a very long tail of a cough. That’s TMI for me to write about in the Health Populi blog, but this story has a current-events twist: the pharmacist could not electronically link with my insurance company to transact my payment. He tried a few work-flows, and ended up using a discount card which in the moment worked for us, and I paid the
Ethics for AI in Health – A View From The World Health Organization
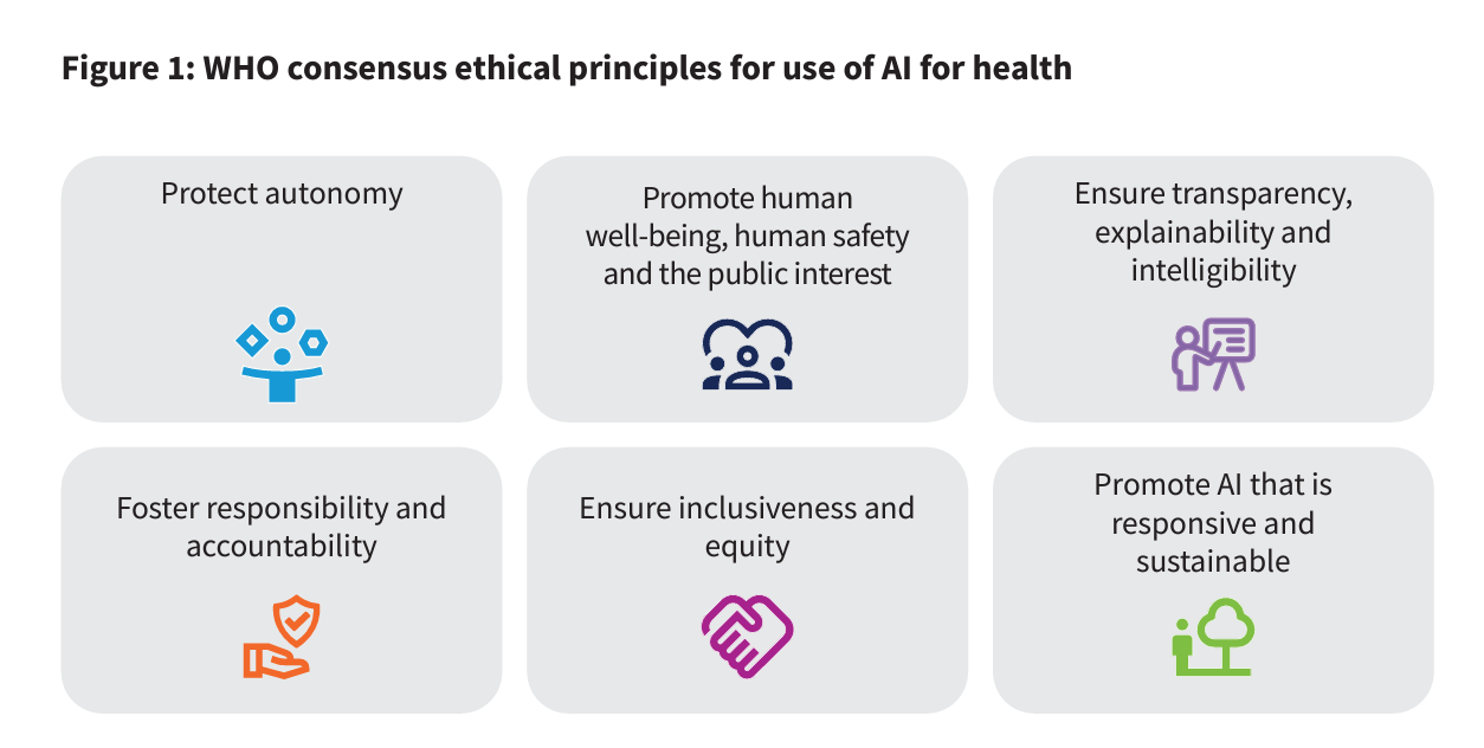
For health care, AI can benefit diagnosis and clinical care, address paperwork and bureaucratic duplication and waste, accelerate scientific research, and personalize health care direct-to-patients and -caregivers. On the downside, risks of AI in health care can involve incomplete or false diagnoses, inaccuracies and errors in cleaning up paperwork, exacerbate differential access to scientific knowledge, and exacerbate health disparities, explained in the World Health Organization’s (WHO) report, Ethics and governance of artificial intelligence for health. WHO has released guidance on the use of large multi-modal models (LMMs) in health care which detail 40+ recommendations for
#BeBurnsAware – What To Know on National Burn Awareness Day
Today 11th October is National Burn Awareness Day 2023, and I’m supporting the effort for all of us to #BeBurnsAware. I have become more bullish on Burn Awareness as I’ve come to learn more about the impact burns have on public, family, and children’s health globally. My teacher for better understanding burns and public health has been Krissie Stiles, a long-time burns nurse specialist and Ambassador to the Children’s Burns Trust in the UK. Meet Krissie. Burns are a global public health challenge, which I detailed here in Health Populi earlier this year. Today
From Managing Healthcare Providers’ Costs to “Revolutionizing” Care – Bain Looks at the Short- and Long-Term for Generative AI
“Generative AI already has the power to alleviate some of providers’ biggest woes, which include rising costs and high inflation, clinician shortages, and physician burnout,” Bain & Company observe in Beyond Hype: Getting the Most Out of Generative AI in Healthcare Today. By the end of this paper, the Bain team expects that those health care leaders who are investing in generative AI today (to start small, to win big in the report’s words) will learn key lessons that will put them “on a path to eventually revolutionize their businesses.” Bain & Company surveyed U.S. health system leaders to gauge their
The Top 10 Patient Safety Concerns for 2023 Are About Social, Mental and Behavioral Health
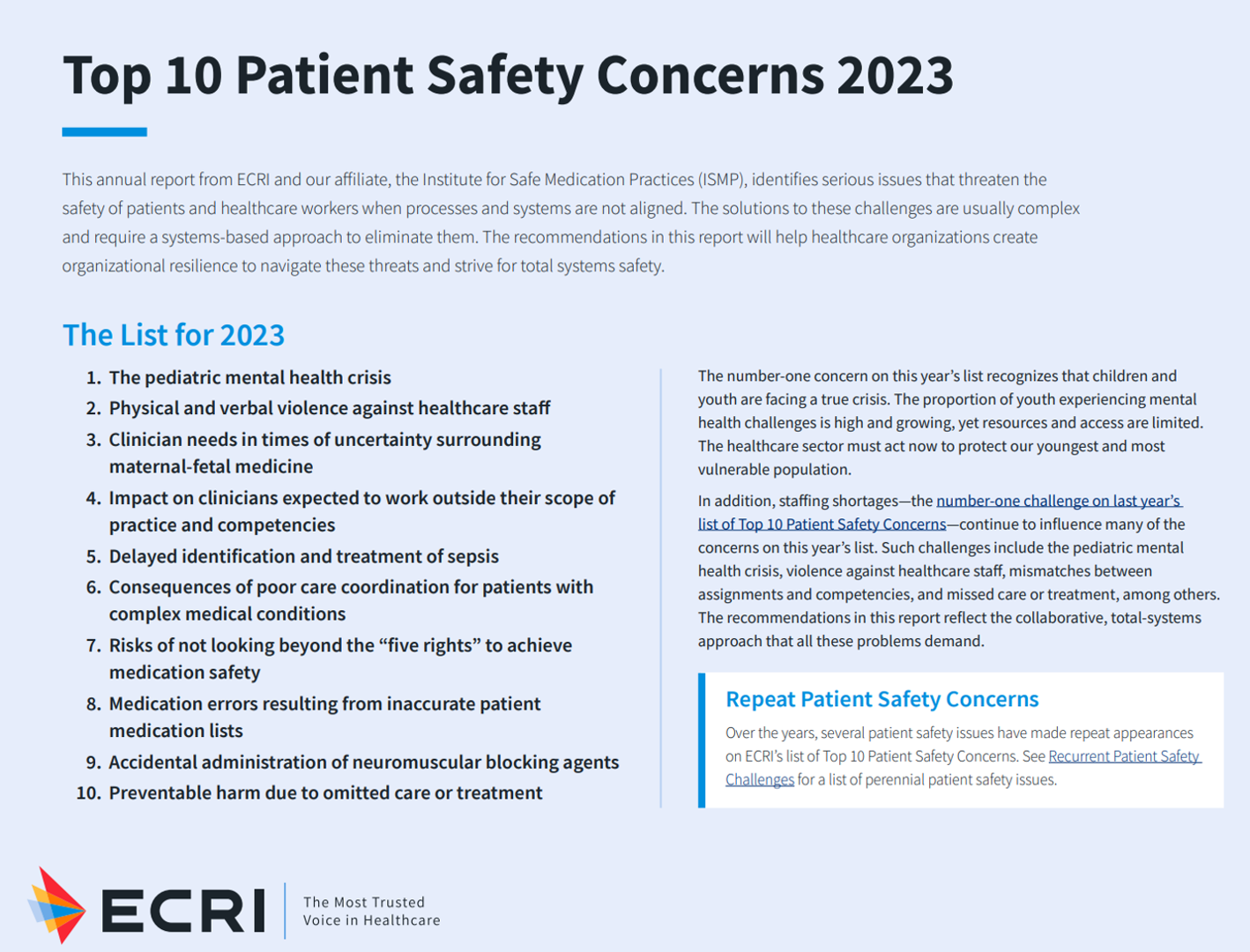
Ten years ago, ECRI named the top 10 health technology hazards for 2013: they were alarm hazards, medication administrative errors using infusion pumps, unnecessary exposure and radiation burns from diagnostic radiology procedures, patient/data mismatches in EHRs and other HIT systems, interoperability failures with medical devices and health IT systems, and five other tech-related hazards. In 2014, ECRI pivoted the title of this annual report to “patient safety concerns,” a nuance away from health technology. Fast forward to 2023 and ECRI’s latest take on the Top 10 Patient Safety Concerns 2023. While technology is embedded in this list, the headlines have more
When Household Economics Blur with Health, Technology and Trust – Health Populi’s 2023 TrendCast

People are sick of being sick, the New York Times tells us. “Which virus is it?” the title of the article updating the winter 2022-23 sick-season asked. Entering 2023, U.S. health citizens face physical, financial, and mental health challenges of a syndemic, inflation, and stress – all of which will shape peoples’ demand side for health care and digital technology, and a supply side of providers challenged by tech-enabled organizations with design and data chops. Start with pandemic ennui The universal state of well-being among us mere humans is pandemic ennui: call it languishing (as opposed to flourishing), burnout, or
Thinking Value-Based Health Care at HLTH 2022 – A Call-to-Action
The cost of health insurance for a worker who buys into a health plan at work in 2022 reached $22,463 for their family. The average monthly mortgage payment was $1,759 in mid-2022. “When housing and health both rank as basic needs in Maslow’s hierarchy, what’s a health system to do?” I ask in an essay published today on Crossover Health’s website titled Value-Based Care: Driving a Social Contract of Trust and Health. The answer: embrace value-based care. Warren Buffett wrote Berkshire Hathaway shareholders in 2008, asserting that, “Price is what you pay. Value
Patient Support Isn’t Just About the Price of Therapy: It’s About Safety, Really Rich Data and Trust
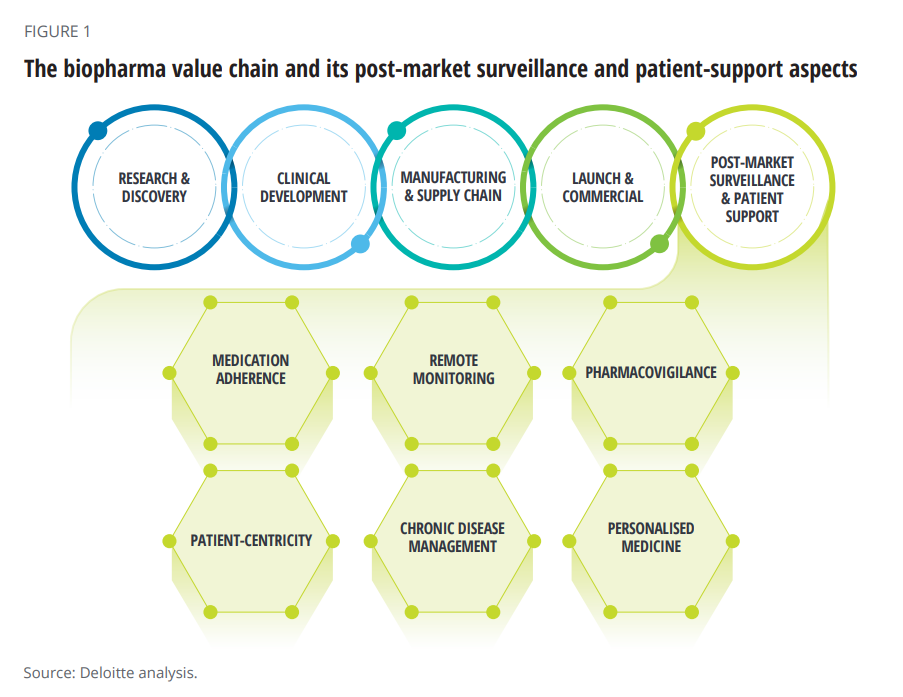
When I talk about patient support programs (PSPs), I’m most often focused on supporting peoples’ access to medicines due to costs, bolstering health literacy, and addressing health citizens’ risks of drivers of health that can be obstacles to optimal health outcomes (those challenging social determinants of health). A new report from Deloitte on Intelligent post-launch patient support speaks to another crucial definition of patient support: post-market surveillance and patient safety. The paper’s central thesis is that improving patient support is a critical step in the biopharma value chain, illustrated in the first diagram
How Trust and Geopolitics Will Impact Health and Business – Edelman 2022 Trust Barometer at the World Economic Forum in Davos

When we think about the state of Trust in in mid-2022, there is some good news: Trust is rising (at least in democratic countries, while falling in autocratic ones). The bad news: the gap in Trust has dramatically widened between higher-income people compared with those earning lower-incomes, globally. And that gap is “tinder” that can be quickly sparked into a socio-political fire in countries around the world, Richard Edelman cautioned today when introducing the latest look at the 2022 Edelman Trust Barometer, focusing on geopolitics and business. We have never seen numbers like this
McKinsey’s Six Shifts To Add Life to Years — and One More to Consider
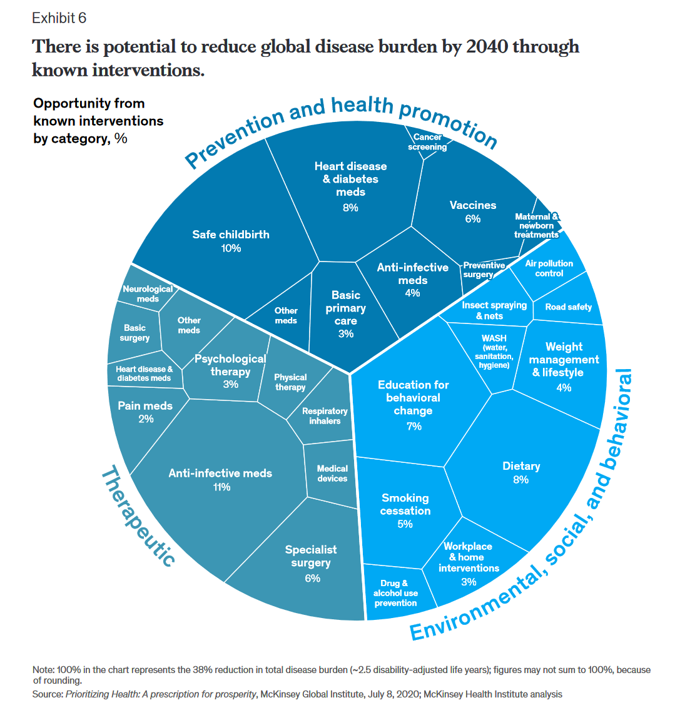
People spend one-half of their lives in “less-than-good health,” we learn early in the paper, Adding years to life and life to years from the McKinsey Health Institute. In this data-rich essay, the McKinsey team at MHI sets out an agenda that could help us add 45 billion extra years of higher-quality life equal to an average of six years per person (depending on your country and population demographics). The first graphic from the report illustrates four dimensions of health and the factors underneath each of them that can bolster or diminish our well-being: personal behaviors (such as sleep and diet),
Medical Distancing Is Bad For Your Health

“Social distancing is great. Medical distancing? Not so much,” I observe in Medical Distancing in America: A Lingering Pandemic Side Effect., my essay published this week in Medecision’s Liberate Health blog. Since we learned to spell “coronavirus,” we also learned the meaning and risk-managing importance of physical distance early in the COVID-19 pandemic. But medical distancing became a corollary life-flow of the physical version, and for our collective health and well-being, it hasn’t been good for our health in ways beyond keeping our exposure to the virus at bay. For health care providers — physicians, hospitals, ambulatory clinics, diagnostic centers —
Still Struggling with Stress in America in 2021
“Americans remain in limbo between lives once lived and whatever the post-pandemic future holds,” the American Psychological Association observes in their latest read into Stress in America 2021, with this phase of the perennial study focused on Stress and Decision-Making During the Pandemic. The top-line: people face a daily web of risk assessment, up-ended routines, and endless news about the coronavirus locally and globally. While most people in the U.S. believe that “everything will work out” after the pandemic ends, the mental, emotional, and logistical daily distance between “now” and “then” brings uncertainty and indeed, prolonged stress. More Millennials, who
The Biggest Threat to Our Health Isn’t the Next Pandemic or Cancer…It’s Climate Change
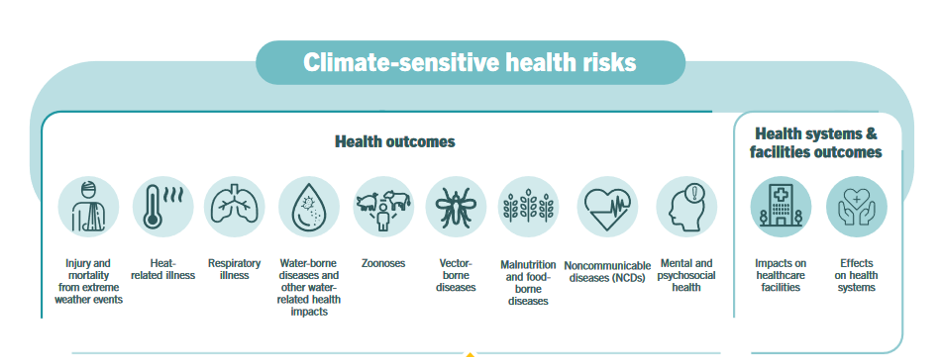
Before the coronavirus emerged, the top causes of death in developed countries were heart disease, cancers, diabetes, and accidents. Then COVID-19 joined the top-10 list of killers in the U.S. and the issue of pandemic preparedness for the next “Disease X” became part of global public health planning. But the biggest health threat to human life is climate change, according to a new report from the World Health Organization titled The Health Argument for Climate Action. It’s WHO’s special report on climate change and health, dedicated to the memory of Ella Kissi-Debrah — a child who died succumbing to impacts
Crossing the Pond by Plane in the Age of Corona – My View From the Hygienic Skies and on the Ground in Belgium
Years before we knew how to spell “coronavirus,” I gained Italian citizenship while retaining my U.S. citizenship. My family’s plan was to, soon thereafter, split time for work and life between the U.S. and the E.U. Then, COVID-19 emerged as a pandemic the world over, and the move to Brussels in January 2020 was quite short-lived. Now, the plan is in play and I’m writing this post from our home in Brussels, Belgium. Why Brussels? Among many smart reasons, the city is welcoming, our farm-to-table food style is doable, the walkability is brilliant, and the transportation options are accessible to
COVID-19 Accelerated Digital Health Investments…But It Helps to Be Bigger, Mature and Scaling
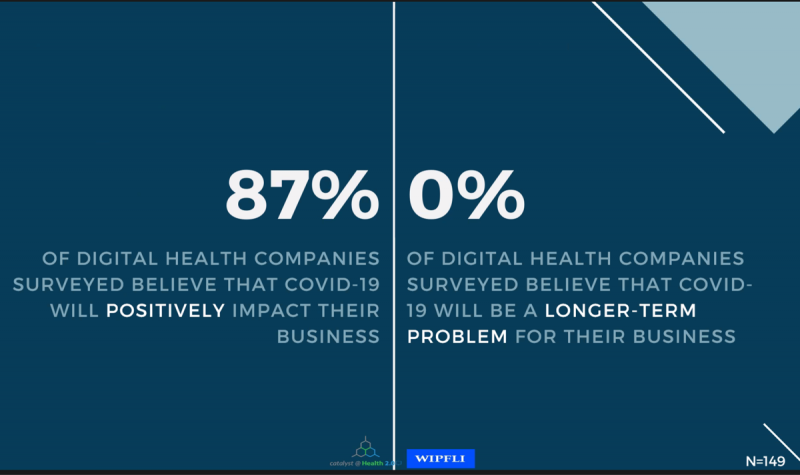
“Compare digital health to airlines, cruise lines, and other industries” and the sector looks quite privileged, opined Matthew Holt in a discussion on a study diving deeply into the State of Digital Health, conducted by Catalyst @ Health 2.0 and sponsored by WIPFLI.. The research was conducted among 335 respondents, which included 182 digital health companies polled between November 2020 and March 2021. Digital health companies represented 60% of the sample, the other 40% of which were consulting firms, subsidiaries of providers/payers/life science companies and tech corporations, and investors. As Matthew called out, the digital health sector has a relatively
Managing the Risks of Fast-Growing Digital Health
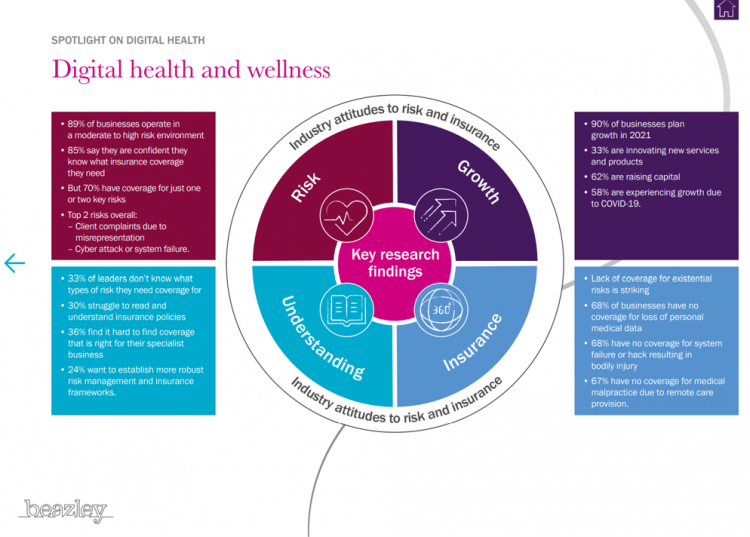
Investments in the digital health sector have fast-grown in the past decade, reaching $14bn in 2020 based on Rock Health’s latest read on the market. The COVID-19 pandemic accelerated the field across many industry segments. With such turbocharged growth on the supply side, Beazley, experts in specialty insurance, explores the risks of digital health and wellness in a new report, Digital health, telehealth and wellness: Attitudes to risk and insurance. With great potential for both innovation and reward comes great risks: Beazley points to the facts that, over two-thirds of digital health companies lack insurance coverage for medical malpractice for
A New Health Literacy Pillar: Personal Data Stewardship
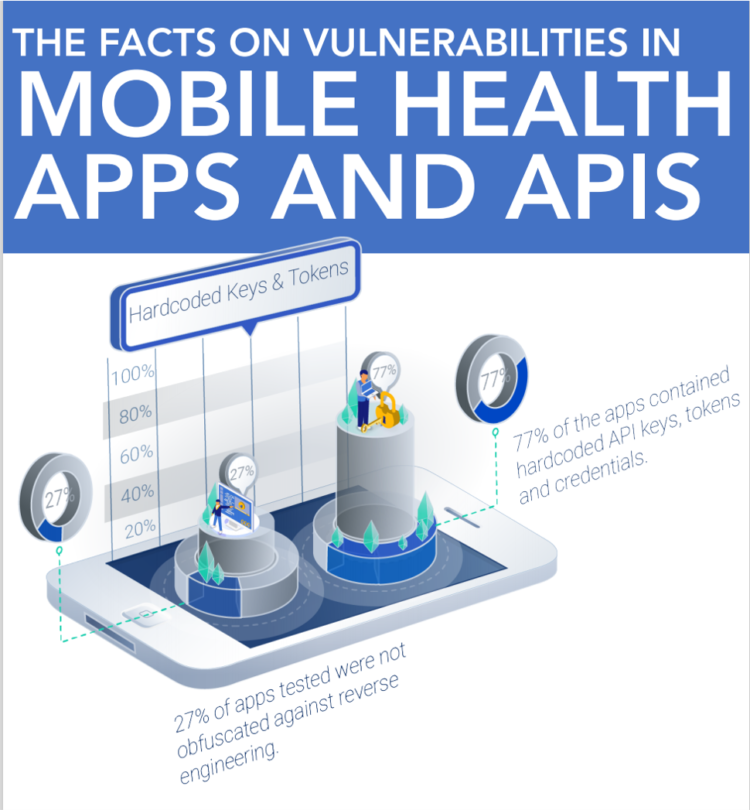
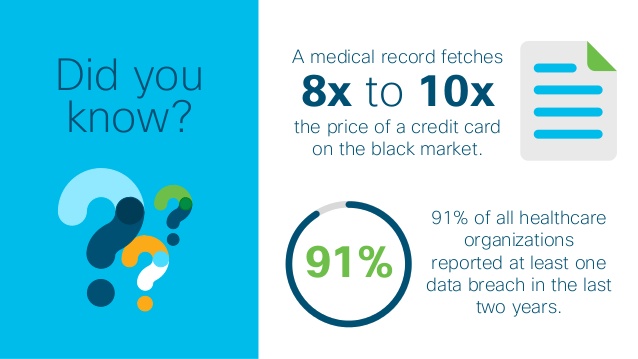
The growing use of APIs in health information technology innovation for patient care has been a boon to speeding development placed in the hands of providers and patients. Using APIs can help drive interoperability and make data “liquid” and useable. APIs can enable “Data liberación,” a concept proposed by Todd Park when he worked in the Obama administration. Without securing patients’ personal health data leveraging APIs, those intimate details are highly hackable explained in All That we Let In, a report from Knight Ink and Appr0ov. It is likely that behind growing health data hacks is the marginally greater financial
Most Americans Want a Vaccine, Dissatisfied with the Rollout
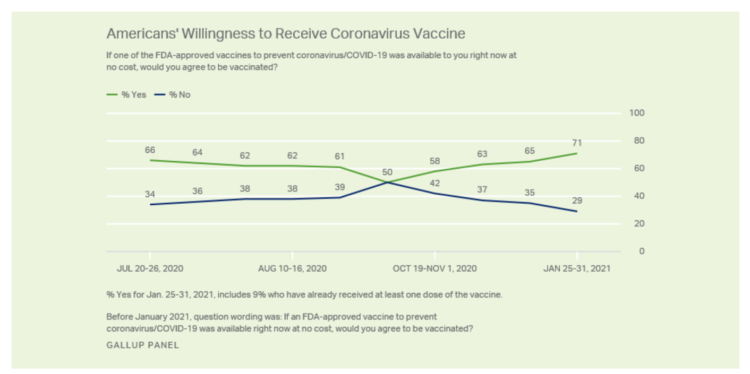
Seven in 10 U.S. adults are willing to be vaccinated, and they’re not happy about the process in getting their jab, according to Gallup’s poll taken in the last week of January 2021. The proportion of Americans willing to receive a COVID-19 vaccine has steadily grown since October 2020, which fell to a mere 50% of folks keen to get the shot. That percentage has risen to 71% as of February 1 2021, as the first line chart shows the reversal in public embrace for vaccination against the coronavirus. Now that most people in the U.S. welcome the opportunity to
The Digital Transformation of Home for Health – Brainstorming with Karsten Russell-Wood of Philips

At the start of CES 2021, I had the opportunity to catch up with Karsten Russell-Wood, Portfolio Marketing Leader, Post Acute & Home, Connected Care at Philips. We brainstormed just as CES 2021 was going to “open,” virtually, for the consumer electronics conference’s first all-virtual meeting. Philips, a longtime major exhibitor at CES, created an entirely new online experience for the CES attendees – a sort of virtual gallery of different exhibits that are accessed from a single point in a “room” with various entry points. One of the company’s key messages for CES 2021 was health care delivered outside
Trust Plummets Around the World: The 2021 Edelman Trust Barometer in #CES2021 and Microsoft Context
Citizens around the world unite around the concept that Trust is Dead. This is no truer than in the U.S., where trust in every type of organization and expert has plummeted in the wake of the COVID-19 pandemic, political and social strife, and an economic downturn. Welcome to the sobering 2021 Edelman Trust Barometer, released this week as the world’s technology innovators and analysts are convening at CES 2021, and the annual JP Morgan Healthcare meetup virtually convened. As the World Economic Forum succinctly put the situation, “2020 was the year of two equally destructive viruses: the pandemic and the
Behavioral Health Side-Effects in the COVID Era
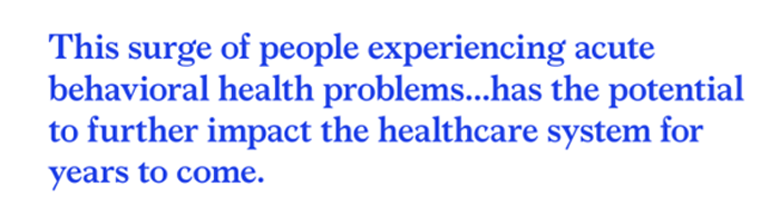
“This surge of people experiencing acute behavioral health problems…has the potential to further impact the healthcare system for years to come,” a report from McKinsey expects looking at the hidden costs of COVID-19’s impact on U.S. health care. The coronavirus pandemic has taken a toll on Americans’ mental health, with anxiety and depression growing as a side-effect to worries about the virus itself, the long Great Lockdown in much of the country, and the economic recession that has particularly impacted women and people of color. I covered depression impacts due to COVID-19 here in Health Populi yesterday, and wanted to
An Airline, A Hospital and A Disinfectant Brand Walk Into A(n Airport) Bar–the New Health/Care Collaboration in the Age of COVID

You’ve heard the one about three characters walking into a bar. A new collaboration between United Airlines, Cleveland Clinic and Clorox reminded me of that scenario, and that in the age of the coronavirus pandemic, collaboration can bolster our health. In the era of COVID-19, people — consumers. patients managing chronic conditions, and caregivers (whether for younger or older loved ones) — are concerned about contracting the virus. In U.S. states where governors mandated shelter-at-home for much of the first half of 2020, millions of people have become conditioned to physically distance, wear face coverings, and #StayHome. In particular, workers
Saving Money as a Financial Vaccine: BlackRock Finds Consumer Savings Drain and Etsy Sellers Not Saving Much
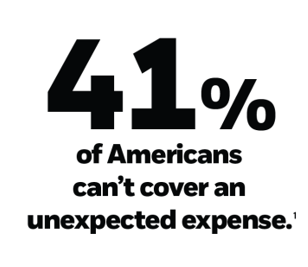
“Americans are feeling incredible financial pressure as a result of the COVID outbreak,” John Thompson, Chief Program Officer with the Financial Health Network. One in three people in the U.S. has skipped or stopped paying a bill, and over half of Americans have used emergency savings, according to a survey from the BlackRock Emergency Savings Initiative (ESI). BlackRock, the investment firm, allocated $50 million in February 2019 to form the ESI, focused on helping people with lower incomes to bolster savings and financial health. BlackRock partners in the ESI with the Financial Health Network, CommonWealth, the Center for Advanced Hindsight Common
How COVID-19 Is Driving More Deaths of Despair
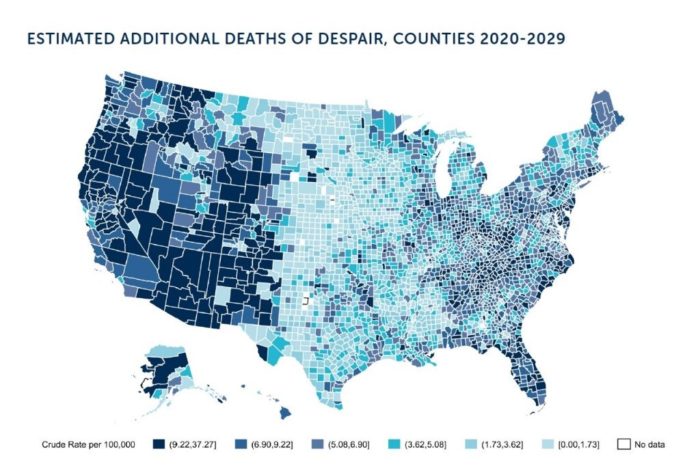
In the current state of the COVID-19 pandemic, we all feel like we are living in desperate times. If you are a person at-risk of dying a Death of Despair, you’re even more at-risk of doing so in the wake of the Coronavirus in America. Demonstrating this sad fact of U.S. life, the Well Being Trust and Robert Graham Center published Projected Deaths of Despair from COVID-19. The analysis quantifies the impact of isolation and loneliness combined with the dramatic economic downturn and mass unemployment with the worsening of mental illness and income inequity on the epidemic of Deaths of
How the Coronavirus and Technology Are Reshaping Home-Work, -Life and -Health
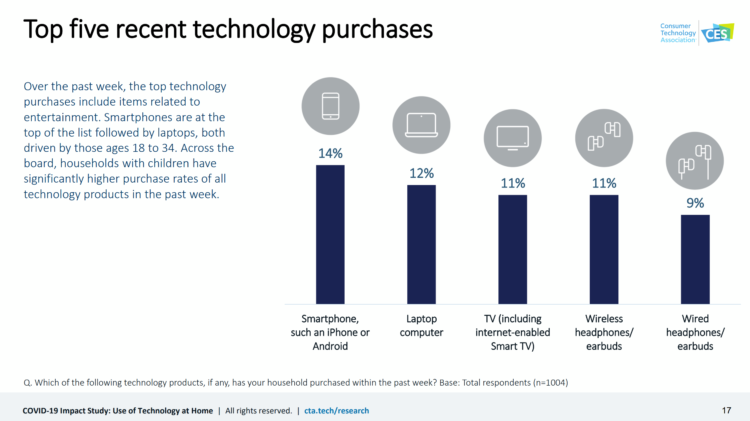
As people conform to the #StayHome lifestyle to #FlattenTheCurve of the coronavirus pandemic, technology is transforming peoples’ home lives for working, playing, and socializing. The Consumer Technology Association has conducted the COVID-19 Impact Study assessing the use of technology at home, exploring U.S. households’ changing behaviors for consuming content, stocking the pantry, engaging with social media, and using online health and fitness tools. This research surveyed 1,004 U.S. adults 18 and over in March 2020 — early in the U.S. pandemic’s national “curve.” U.S. consumers’ top five technology purchases in mid-March 2020 were for smartphones, laptop computers, TVs, and headphones/earbuds.
The COVID19 Consumer: #AloneTogether and More Health Aware
The number of diagnoses of people testing positive with the coronavirus topped 14,000 today in the U.S., Johns Hopkins COVID-19 interactive map told us this morning. As tests have begun to come on stream from California on the west coast to New York state on the east, the U.S. COVID-19 positives will continue to ratchet up for weeks to come, based on the latest perspectives shared by the most-trusted expert in America, Dr. Anthony Fauci. This report from the U.S. Department of Health and Human Services on the nation’s response to the coronavirus pandemic, published March 13, 2020, forecasts a
Making Health Care Better, from the N of 1 to the Public’s Health – Trend-Weaving Medecision Liberation 2019
Health and our health information are deeply personal. Changing health care and inspiring positive health behaviors is hard to do. But we must and we will, a group of inspiring and inspired people who work across the health/care ecosystem affirmed this week in Dallas at the conference of Medecision Liberation 2019. I was engaged at this conference to wear several hats — as a keynote speaker, a sort of “emcee,” and, finally, to trend-weave the many talks and discussions happening throughout the meeting. This post is my synthesis of the summary I delivered live at the end of the conference,
A Matter of Trust, Perception, Risk, and Uncertainty – The Big Issues Raised by the Acquisition of PatientsLikeMe and Other Patient Data Transactions

By Susannah Fox, Jane Sarasohn-Kahn and Lisa Suennen I’ve lived long enough to have learned The closer you get to the fire the more you get burned But that won’t happen to us Cause it’s always been a matter of trust A Matter of Trust, by Billy Joel If you’re in health care and don’t live under a rock, you have probably heard that United Health Group (UHG) has acquired PatientsLikeMe (PLM). After the announcement, there was a lot of sound and fury, some of which signified nothing, as the saying goes, and some which signified a lot.
A Concerning Gap in Cybersecurity for Connected Medical Technology

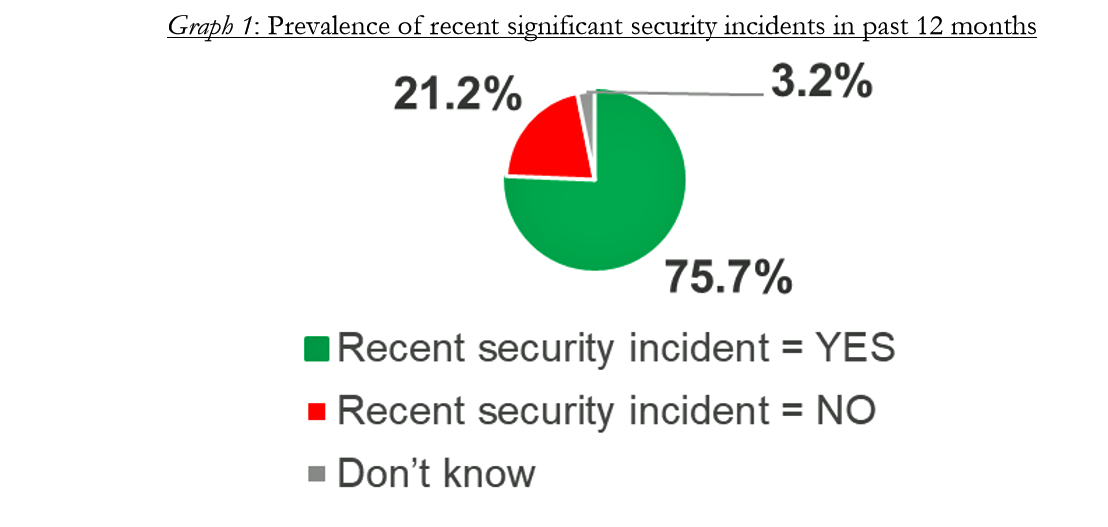
Notwithstanding mass adoption of antivirus protection and firewalls among healthcare providers, there remains a security gap for biomedical technologies, according to a report from Zingbox. This concerning finding was confirmed in recent observations from Gartner, which wrote in a market trends report that, “generally, medical devices are not replaced for at least ten years, with many running old software that has not been updated or patched.” Zingbox learned that most healthcare executives say they’re confident in their ability to protect connected medical devices: 79% of health IT professionals say they have real-time information about which connected devices are vulnerable to
Best Buy Bets on AgingTech in the Expanding Retail Health Ecosystem

With the acquisition of GreatCall, a mature player in the aging-tech space, Best Buy is doubling down on consumer health technology@retail. This week at Best Buy. the electronics retailer, it’s out with CDs and in with technology for aging at home. The company announced that it would buy GreatCall for $800 million. A snippet from the announcement from Best Buy’s press release is shown in the first diagram, noting that GreatCall’s membership is approaching 1 million subscribers who use mobile phones and connected devices, “providing peace of mind to their loved ones.” Beyond the obvious “falling and I can’t get
Healthcare Information In-Security Is the New Normal

Three-fourths of healthcare providers experienced a data breach in 2017, according to the HIMSS 2018 Cybersecurity Survey. Health data insecurity is the new normal. A big piece of addressing the cybersecurity healthcare challenge is educating people who work in healthcare settings, and that has been under-funded. Only 41% of healthcare workers say they receive security training, a Forrester study learned in January 2018. Forrester also found that while healthcare organizations have experienced some of the most egregious cyberattacks, the industry allocates a smaller proportion of IT budgets to security compared with than other organizational types at a rate of 22%
Consumer Trust, Privacy and Healthcare – Considering #HIMSS18 in the Stark Light of Facebook and Cambridge Analytica
What a difference a couple of weeks make…. On 1st March 2018, two over-arching issues remained with me leaving Las Vegas and #HIMSS18: the central, recognized role of cybersecurity threats in healthcare, and the growing use of consumer-facing technologies for self- and virtual care. Eighteen days later, we all learned about Cambridge Analytica’s misuse of 50 million Americans’ social network data posted on Facebook. We who work in healthcare must pose the questions: going forward, how trusting will patients, consumers and caregivers be sharing their personal health information (PHI)? Will people connect dots between their Facebook lives – and their
Patient Privacy And Cyber In-Security at HIMSS 2018
Nearly one-half of Americans experienced a personal data breach in the past three years, the third annual national cybersecurity survey found. Ensuring privacy and cybersecurity should become integrated into the healthcare industry’s consideration of a patient’s consumer experience. This makes sense, given that privacy and cybersecurity ranked the second highest priority to hospitals and healthcare providers polled in HIMSS 2018 Healthcare Leadership Survey. Providers put patient safety as #1. Appropriately, privacy and security were hot topics at HIMSS Annual Conference this year, in respond to providers’ demands for more education and concerns around the challenges. Let’s put these concerns in
Hug Your Physician: S/He Needs It – Listening to the 2018 Medscape National Physician Burnout & Depression Report

Two in five U.S. physicians feels burned out, according to the Medscape National Physician Burnout & Depression Report for 2018. This year, Medscape explicitly adds the condition of “depression” to its important study, and its title. In 2017, the Medscape report was about bias and burnout. Physicians involved in primary care specialties and critical care are especially at-risk for burnout, the study found. One in five OBGYNs experience both burnout and depression. Furthermore, there’s a big gender disparity when it comes to feeling burned out: nearly one-half of female physicians feel burnout compared with 38% of male doctors. Being employed by
Health Care Is 2.5 More Expensive Than Food for the Average U.S. Family
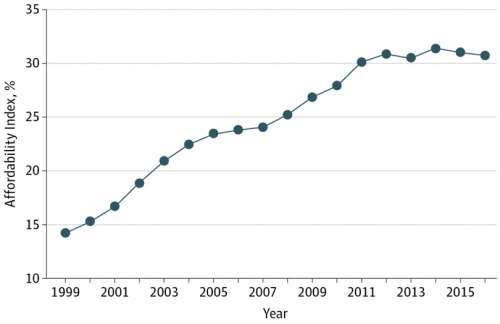
The math is straightforward. Assume “A” equals $59.039, the median household income in 2016. Assume “B” is $18,142, the mean employer-sponsored family insurance premium last year. B divided by A equals 30.7%, which is the percent of the average U.S. family’s income represented by the premium cost of health insurance. Compare that to what American households spent on food: just over $7,000, including groceries and eating out (which is garnering a larger share of U.S. eating opportunities, a topic for another post). Thus, health care represents, via the home’s health insurance premium, represents 2.5 times more than food for the
Patients’ Healthcare Payment Problems Are Providers’, Too
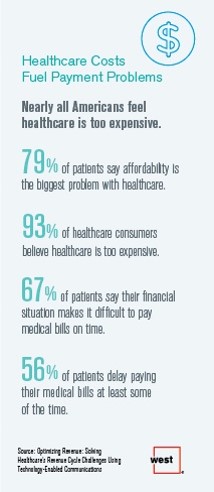
Three-quarters of patients’ decisions on whether to seek services from healthcare providers are impacted by high deductible health plans. This impacts the finances of both patients and providers: 56% of patients’ payments to healthcare providers are delayed some of the time, noted in Optimizing Revenue: Solving Healthcare’s Revenue Cycle Challenges Using Technology Enabled Communications, published today by West. Underneath that 56% of patients delaying payments, 12% say they “always delay” payment, and 16% say they “frequently delay” payment. West engaged Kelton Global to survey 1,010 U.S. adults 18 and over along with 236 healthcare providers to gauge their experiences with
Loneliness and Isolation Kill: Health Depends on Purpose
In the U.S., one-third of people age 65 and over have difficulty walking 3 city blocks. Hold that thought, and consider the role of purpose in life: purpose drives well-being, inoculating one’s life with meaning, direction, and goals, as the On Purpose guru Victor Strecher explains in his amazing graphic manifesto. Having a higher sense of purpose in life is associated with higher probability of people engaging in healthier behaviors, such as greater physical activity and seeking preventive healthcare; better biological functioning; and, lower risk of disease. Four researchers from the Harvard School of Public Health connected the dots between
Strengthening Chronic Care Is Both Personal and Financial for the Patient
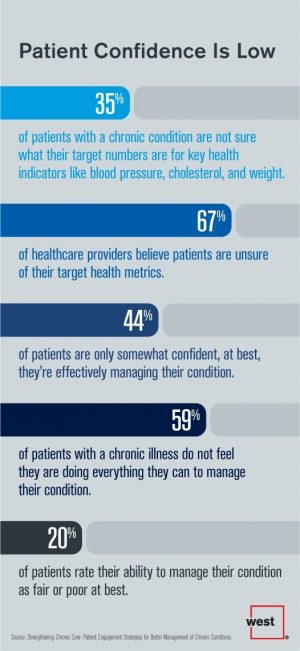
6 in 10 people diagnosed with a chronic condition do not feel they’re doing everything they can to manage their condition. At the same time, 67% of healthcare providers believe patients aren’t certain about their target health metrics. Three-quarters of physicians are only somewhat confident their patients are truly informed about their present state of health. Most people and their doctors are on the same page recognizing that patients lack confidence in managing their condition, but how to remedy this recognized challenge? The survey and report, Strengthening Chronic Care, offers some practical advice. This research was conducted by West
A New Health Risk: Hacked Personal Medical Devices
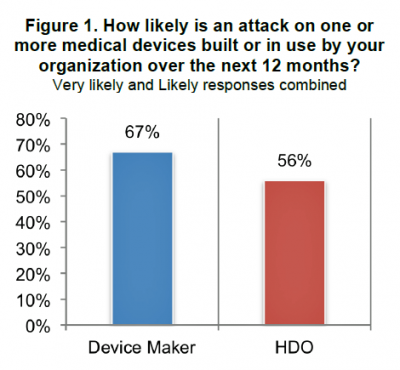
We have entered an era of insecurity in healthcare in America. While major attention is being paid to healthcare insurance and service insecurity, food insecurity and financial insecurity, there’s another one to add to this list: medical device security. As more medical devices have moved into the digital internet-connected mode, the risk for malware, ransomware, and overall hack-ability grows. This increasing and challenging risk is covered in the report, Medical Device Security: An Industry Under Attack and Unprepared to Defend from Ponemon Institute. Ponemon Institute has been tracking information security across industries, including healthcare, for several years. In this survey, sponsored
Building Digital Trust Is Now Part of Serving Up Healthcare

The most trusted stewards for protecting consumers’ health data are “my providers:” “my” physician (88%), “my” pharmacy (85%), and “my” hospital” (84%). according to the Accenture 2017 Consumer Survey on Healthcare Cybersecurity and Digital Trust. Who’s least-trusted? Government (56%) and tech companies (57%). Note, though, that most Americans (over 50%) trust these health data holders — it’s just that fewer people trust them than healthcare providers, who are top health information protectors in health consumers’ trust rosters. Accenture commissioned Nielsen to conduct this survey in November 2016 in seven countries. The results discussed here in Health Populi focus on the
The Growth of Digital Health @Retail

This post was written to support the upcoming meeting of the PCHA, the Personal Connected Health Alliance, to be held 11-14 December 2016 at the Gaylord Hotel in greater Washington, DC. You can follow the events and social content via Twitter using the hashtag #Connect2Health. Have you visited your local Big Box, discount or consumer electronics store lately? You’ll find expanding shelf space for digital health technologies aimed squarely at consumers. 2017 promises even more of them, aimed at helping people accomplish health tasks once performed in hospitals and by healthcare providers, or tasks not yet delivered in today’s healthcare
Building the Primary Care Dream Team
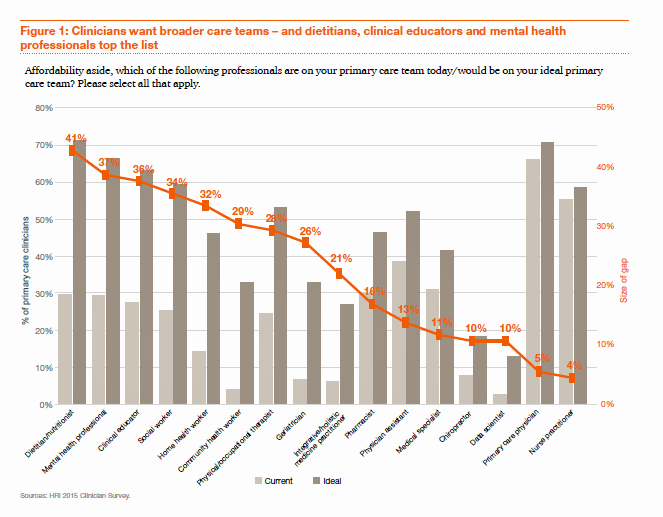
“Today’s primary care won’t work tomorrow,” given the shortage of primary care providers (PCPs) and the need to do more in healthcare with fewer resources in the emerging value-based economy. So let’s re-imagine primary care models, PwC asserts, and makes the case in their report, ROI for primary care: Building the dream team. What’s the financial impact of this dream team on healthcare providers? It’s potentially $1.2 million in savings for every 10,000 patients served, PwC calculates. Historically, physicians have been loath to share their work with non-physicians because of how doctors have been paid — on the basis of fee-for-service,
Doctors Are Growing to Like Digital Health Tools, Says the AMA
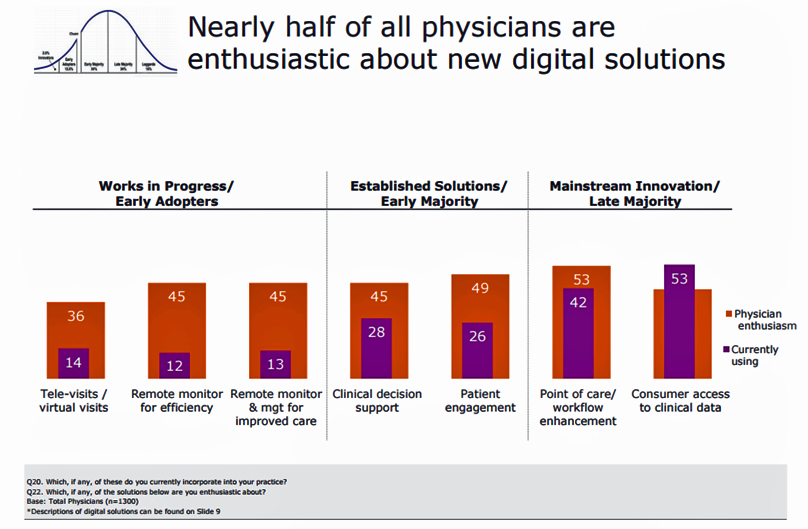
Notwithstanding the head of the AMA recently referring to digital health technologies as “snake oil,” it appears that one-half of physicians is keen on digital health. And scale, not age, matters when it comes to doctors using digital health tools. The American Medical Association (AMA) surveyed physicians on their use of digital health tools, finding that primary care physicians (PCPs) and doctors working in larger and more complex practices tend to be more digital. In Physicians’ motivations and requirements for adopting digital clinical tools, the AMA’s digital health study, “Physicians are optimistic about digital health innovation and its game-changing potential
More Patients Morph Into Financially Burdened Health Consumers
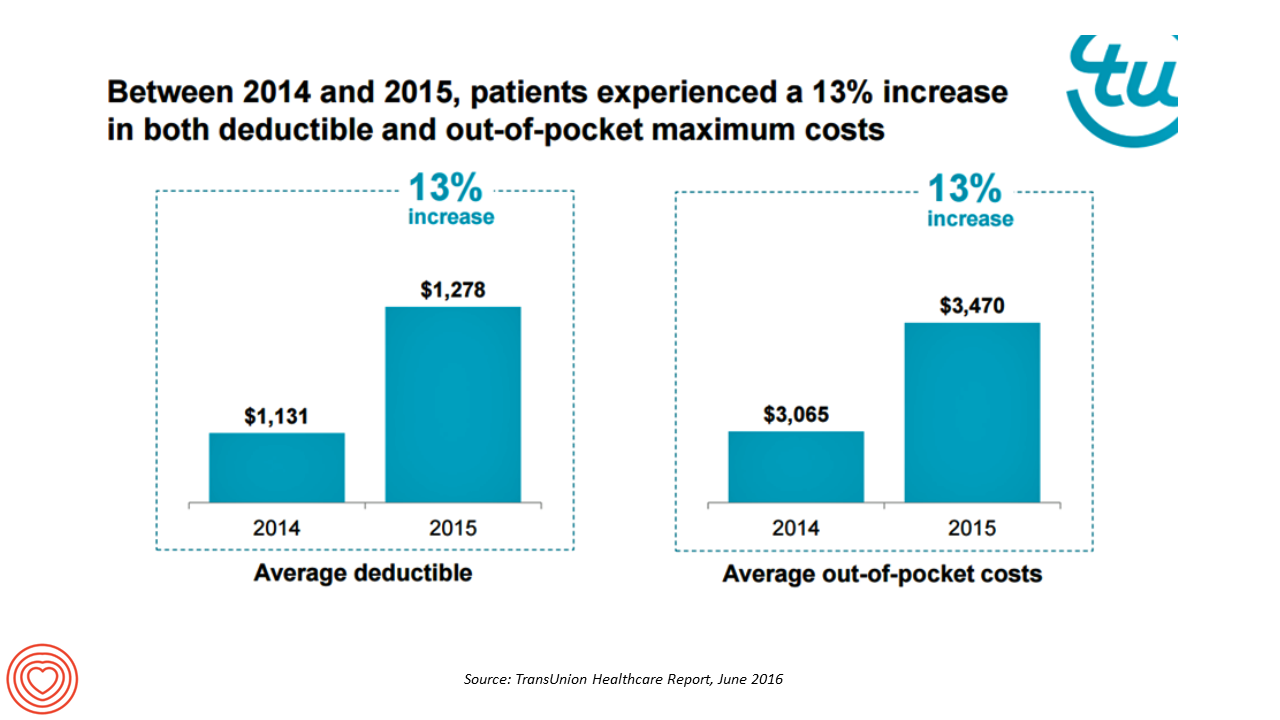
Health care payment responsibility continues to shift from employers to employee-patients, More of those patients are morphing into financially burdened health consumers, according to TransUnion, the credit agency and financial risk information company, in the TransUnion Healthcare Report published in June 2016. Patients saw a 13% increase in their health insurance deductible and out-of-pocket (OOP) maximum costs between 2014 and 2015. At the same time, the average base salary in the U.S. grew 3% in 2015, SHRM estimated. Thus, deductibles and OOP costs grew for consumers more than 4 times faster than the average base salary from 2014 to 2015. In
Better Aging Through Technology
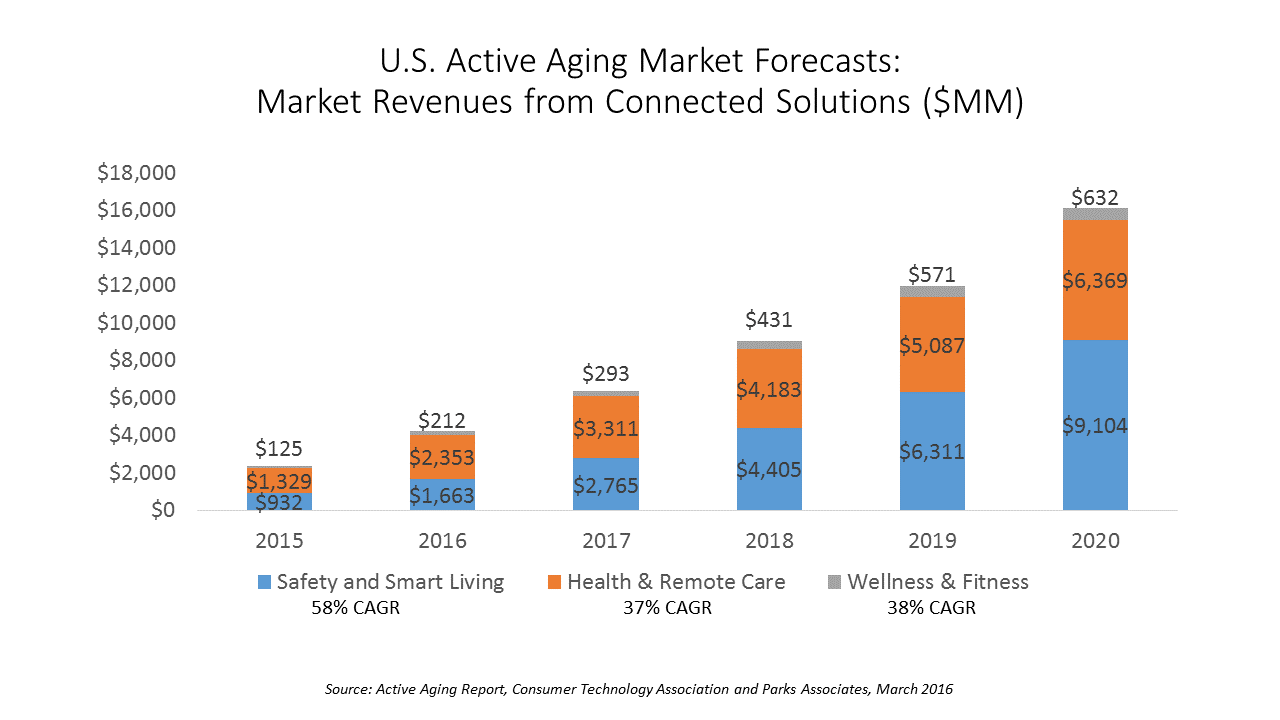
There are 85 million people getting older in America, all mindfully working to not go gentle into their good nights — that is, working hard to stay young and well for as long as they can. This is the market for “active aging” technology products, which will be worth nearly $43 billion in 2020, according to a report from the Consumer Technology Association (CTA), the Active Aging Study. CTA and Parks Associates define the active aging technology market in three segments with several categories under each: Safety and smart living, which includes safety monitoring, emergency response (PERS), smart living, and home
What Retail Financial Services Can Teach Healthcare
“Banks and insurance companies that cannot keep pace will find their customers, busy pursuing flawless service models and smart solutions, have moved on without them and they are stranded on the wrong side of the digital divide — from which there will be no return,” according to a report on The Future of Retail Financial Services from Cognizant, Marketforce, and Pegasystems. You could substitute “healthcare providers” for “banks and insurance companies,” because traditional health industry stakeholders are equally behind the consumer demand for digital convenience. This report has important insights relevant to health providers, health plans and suppliers (especially for
Tying Health IT to Consumers’ Financial Health and Wellness

As HIMSS 2016, the annual conference of health information technology community, convenes in Vegas, an underlying market driver is fast-reshaping consumers’ needs that go beyond personal health records: that’s personal health-financial information and tools to help people manage their growing burden of healthcare financial management. There’s a financial risk-shift happening in American health care, from payers and health insurance plan sponsors (namely, employers and government agencies) to patients – pushing them further into their role as health care consumers. The burden of health care costs weighs heavier on younger U.S. health citizens, based on a survey from the Xerox Healthcare
IoT in Healthcare, Take 3 – Accenture & the Internet of Me in Health
We’re entering the era of personalized healthcare promising convenient and meaningful health experiences, according to Accenture’s 2015 Healthcare IT Vision articulated in their report, Top 5 eHealth Trends. This post is third in three published here on Health Populi this week, exploring the growing role of the Internet of Things in health/care. On 8th July, we dug into McKinsey Global Institute’s research on IoT’s influence over nine industries, including human health; and on the 9th, we reviewed Goldman Sachs’ report on digital health’s potential impact on the U.S. healthcare system. Accenture’s five eHealth trends include: The Internet of Me; the Outcome Economy, with
John Hancock flips the life insurance policy with wellness and data
When you think about life insurance, images of actuaries churning numbers to construct mortality tables may come to mind. Mortality tables show peoples’ life expectancy based on various demographic characteristics. John Hancock is flipping the idea life insurance to shift it a bit in favor of “life” itself. The company is teaming with Vitality, a long-time provider of wellness tools programs, to create insurance products that incorporate discounts for healthy living. The programs also require people to share their data with the companies to quality for the discounts, which the project’s press release says could amount to $25,000 over the
The Affordable Care Act As New-Business Creator
While there’s little evidence that the short-term impact of the Affordable Care Act has limited job growth or driven most employers to drop health insurance plans, the ACA has spawned a “cottage industry” of health companies since 2010, according to PwC. As the ACA turned five years of age, the PwC Health Research Institute led by Ceci Connolly identified at least 90 newcos addressing opportunities inspired by the ACA: Supporting telehealth platforms between patients and providers, such as Vivre Health Educating consumers, such as the transparency provider HealthSparq does Streamlining operations to enhance efficiency, the business of Cureate among others
Value is in the eye of the shopper for health insurance
While shopping is a life sport, and even therapeutic for some, there’s one product that’s not universally attracting shoppers: health insurance. McKinsey’s Center for U.S. Health System Reform studied people who were qualified to go health insurance shopping for plans in 2015, covered by the Affordable Care Act. McKinsey’s consumer research identified six segments of health insurance plan shoppers — and non-shoppers — including 4 cohorts of insured and 2 of uninsured people. The insureds include: Newly-insured people, who didn’t enroll in health plans in 2014 but did so in 2015 Renewers, who purchased health insurance in both 2014 and
Privacy and the Internet of Your Healthy Things – the FTC says less (data) is more
The FTC has weighed in on privacy and security and the Internet of Things (IoT) in a report published on 27th January 2015. When it comes to IoT and devices that connect to the internet, the FTC will focus on Enforcing privacy laws Educating consumers and business on privacy and security for connected devices Participate in multi-stakeholder groups such as the NTIA’s team considering guidelines for facial recognition, and Advocate with other agencies, at the state level, and with courts. The report summarizes input received in a FTC workshop conducted in November 2013 with IoT industry experts, and offers recommendations
Health care costs, access and Ebola – what’s on health care consumers’ minds
The top 3 urgent health problems facing the U.S. are closely tied for first place: affordable health care/health costs, access to health care, and the Ebola virus. While the first two issues ranked #1 and #2 one year ago, Ebola didn’t even register on the list of healthcare stresses in November 2013. Gallup polled U.S. adults on the biggest health issues facing Americans in early November 2014, and 1 in 6 people named Ebola as the nation’s top health problem, ahead of obesity, cancer, as well as health costs and insurance coverage. Gallup points out that at the time of
Health-wear – at Health 2.0, health met fashion, function and care
Wearables met health and medicine at the 8th annual Health 2.0 Conference in Santa Clara, CA, last week. I had the real pleasure of shepherding a wearables panel of five innovators during the conference, in a well-attended session followed by an energetic Q&A. The organizations who demonstrated their tools and brainstormed the wearables market included, in alphabetical order, Atlas Wearables, Heartmath, MySugr, SunSprite and Withings. I hasten to add that among the five presenters, two were women: that 2 in 5 = 40% gender representation is, happily to my way of thinking about women’s roles in health-making, a very good
Joan Rivers lessons for health and wellness: think like a Bee and Laugh
If laughter is the best medicine, Joan Rivers earned an MD in my personal health ecosystem. My parents loved and laughed with her comedy when pioneered stand-up comedy on TV, and I became increasingly intrigued in and impressed by her vitality, her tenacity, and her survival strategies. I also shared a love of her bee pins with my mother-in-law; the pins were created by Joan and her team for QVC, the electronic retailer, with whom Joan forged a profitable and popular line of fashion, jewelry and home decor. The bee, Joan explained, is anatomically and aerodynamically unfit to fly. Yet,
Hyperconnected Healthcare – The Need for Cyber-Resilience
The growth of data, small and Big, in health care motivates the industry’s stakeholders to adopt technologies that help store, manage and analyze data to drive knowledge and, ultimately, individual and public health. Healthcare is embracing cloud technology, mobile platforms, social networks, e-commerce, robotics, and the Internet of Things (IoT), among a growing list of tech innovations. Each of these innovations, which enable productivity and economic growth, also present cybersecurity risks. The value of these risks is estimated to be as much as $3 trillion to the global economy, according to McKinsey’s calculations in the report Risk and Responsibility in





 Thanks to Jennifer Castenson for
Thanks to Jennifer Castenson for  yeva, digital storyteller, for engaging in
yeva, digital storyteller, for engaging in  Jane joined host Dr. Geeta "Dr. G" Nayyar and colleagues to brainstorm the value of vaccines for public and individual health in this challenging environment for health literacy, health politics, and health citizen grievance.
Jane joined host Dr. Geeta "Dr. G" Nayyar and colleagues to brainstorm the value of vaccines for public and individual health in this challenging environment for health literacy, health politics, and health citizen grievance.