“This surge of people experiencing acute behavioral health problems…has the potential to further impact the healthcare system for years to come,” a report from McKinsey expects looking at the hidden costs of COVID-19’s impact on U.S. health care.
 The coronavirus pandemic has taken a toll on Americans’ mental health, with anxiety and depression growing as a side-effect to worries about the virus itself, the long Great Lockdown in much of the country, and the economic recession that has particularly impacted women and people of color.
The coronavirus pandemic has taken a toll on Americans’ mental health, with anxiety and depression growing as a side-effect to worries about the virus itself, the long Great Lockdown in much of the country, and the economic recession that has particularly impacted women and people of color.
I covered depression impacts due to COVID-19 here in Health Populi yesterday, and wanted to follow that up with this McKinsey study to connect some dots.
In one section of the report, McKinsey focuses on the behavioral health impacts of the pandemic, noting the costs of these are additive to the physical an acute care effects of COVID-19.
Data indicate greater rates of binge drinking and insomnia, for example.
The first chart illustrates data on the impact of COVID-19 on behavioral health across different population groups. Overall, 1 in 3 people in the U.S. could have a behavioral health need in 2021.
To the right, note that 46% of frontline health care workers would need behavioral health support in 2921, and nearly 40% of the newly unemployed due to the economic impact of the pandemic.
 Consider the frontline health care workers data point: behavioral health addresses peoples’ negative or dangerous “behaviors,” like the aforementioned binge drinking which may lead to alcohol use disorder or result from post-traumatic stress as a reaction to the daily grind working in the hospital ICU.
Consider the frontline health care workers data point: behavioral health addresses peoples’ negative or dangerous “behaviors,” like the aforementioned binge drinking which may lead to alcohol use disorder or result from post-traumatic stress as a reaction to the daily grind working in the hospital ICU.
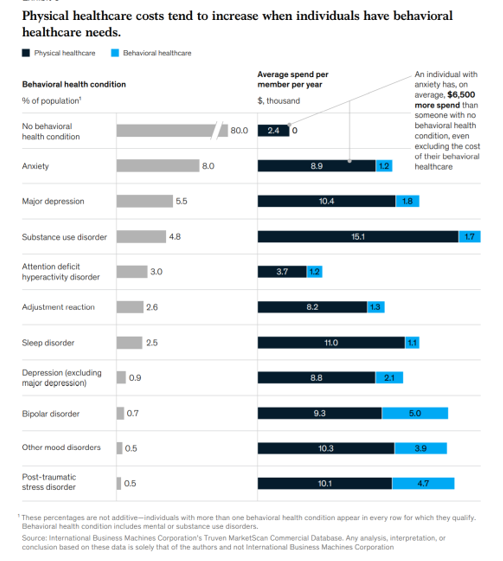
The bar chart here inventories the comorbidity of behavioral health with physical health care costs. Patients with behavioral health conditions generally have greater spending for physical health care than people without behavioral health conditions.
Start at the top of the graphic: a patient with no behavioral health condition would have, on average, $2,400 spend per member per year on just their physical health care costs.
A patient with anxiety would spend $6,500 more on their physical health care compared with someone with no behavioral health condition — not including the cost of their behavioral health care.
Further down the chart, check out PTSD, which adds nearly 50% on top of the physical health care costs to treat the behavioral health condition ($10,100 for the physical component, and $4,700 for the BH cost).\
McKinsey concludes that the behavioral health impact of the pandemic will undoubtedly last beyond 2020, with certain conditions like PTSD not appearing until 2021 and lasting years beyond the onset.
Health Populi’s Hot Points: What Senator Paul Wellstone advocated for and knew way back in 2000 was that mental health is just part of health, and needed to be embedded into primary care and the U.S. health care system in terms of workflow and payment parity.
Paul died in a plane crash in 2002. In 2007, former First Lady Rosalynn Carter allied with David Wellstone, Paul’s son, to lobby Congress to pass mental health insurance legislation.
 While physical health conditions can resolve in weeks or a few months, the impact of mental health on behavior can persist for months into years if undiagnosed or not addressed. Some of McKinsey’s recommendations are for health systems and employers to:
While physical health conditions can resolve in weeks or a few months, the impact of mental health on behavior can persist for months into years if undiagnosed or not addressed. Some of McKinsey’s recommendations are for health systems and employers to:
- Develop virtual health offerings beyond “tele-urgent” care that care for whole patients, physical and mental health care together
- Increase remote and home health care channels for people dealing with chronic or episodic conditions
- Develop an approach to prioritize high-risk consumers built on collaborations between payors and providers
- Strengthen community prevention of behavioral health conditions with crisis-counseling and outreach to promote resilience in the community.
Finally, McKinsey suggests integrating behavioral and physical health services, especially bolstering primary care providers’ competency in mental health. This could include the use of peer-to-peer counselors, universal screening for mental and substance use disorders, and de-stigmatizing mental health in society and in the medical practice.
I recommend that you read this essay on Paul Wellstone’s important legacy for mental health, written by Al Franken in The Atlantic in October 2012.
From the article:
One of Paul’s most famous quotes is this: “Politics is not about power. Politics is not about money. Politics is not about winning for the sake of winning. Politics is about the improvement of people’s lives.”
As we work to re-build a strong health community and system for U.S. health citizens beyond the pandemic moment, we would be wise to keep Paul Wellstone’s integrity and community-wide focus in mind.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.