While the prescription drug bill makes up about 10% of U.S. national health spending, the fastest-growing component of pharmacy spending is specialty medications. These are categorized as “specialty” drugs because they rarely have generic equivalents, and treat serious or life-threatening diseases (such as cancer, MS, and rheumatoid arthritis).
They are also “special” because specialty pharmaceuticals average $3,000 per patient per month and can surpass $100,000 a year for certain products.
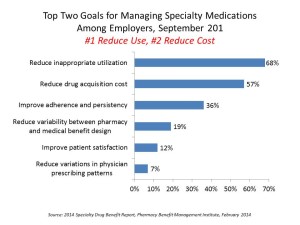
 As a result, the top two goals for managing specialty medications among employers are #1, to reduce inappropriate utilization, and #2, to reduce drug acquisition costs, based on a survey conducted for the Pharmacy Benefit Management Institute. The PBMI’s 2014 Specialty Drug Benefit Report, sponsored by Walgreens, found that the top problems employers see related to specialty meds are the cost of new specialty drug benefits, changes in manufacturer prices for the meds, and accurate measurement of specialty med expenditures under the medical benefit.
As a result, the top two goals for managing specialty medications among employers are #1, to reduce inappropriate utilization, and #2, to reduce drug acquisition costs, based on a survey conducted for the Pharmacy Benefit Management Institute. The PBMI’s 2014 Specialty Drug Benefit Report, sponsored by Walgreens, found that the top problems employers see related to specialty meds are the cost of new specialty drug benefits, changes in manufacturer prices for the meds, and accurate measurement of specialty med expenditures under the medical benefit.
This third problem – the inability to accurately measure the cost trends of specialty meds – is especially acute for smaller employers, who have an opportunity to impact what they can’t effectively measure.
One of the surprising findings in this study was that the opportunity to improve adherence and persistency for specialty meds was ranked by 1 in 2 employers as a top goal in 2011, but this fell to 36% in 2013. The opportunity to reduce inappropriate utilization grew in importance among employers as the role of adherence slipped between 2011 and 2013.
The key strategies being used to manage pharmacy and medical benefits include:
- Prior authorization, used by 90% of employers for the pharmacy benefit and 68% for the medical benefit
- Preferred products and formulary, used by 85% for pharmacy and 44% for medical
- Clinical care management programs, used by 82% for pharmacy and 55% for medical
- Step therapy, used by 74% for pharmacy and 43% for medical
- Limit specialty products to 30-day supply, used by 65% for pharmacy and 41% for medical.
Prior authorization, preferred products/formulary, and step therapy have significantly grown in use between 2011 and 2013.
The study also found that cost-sharing by plan beneficiaries substantially varies: for example, copayment amounts ranged from $10 to $250, and coinsurance percentages also vary widely, between 10% and 80% for the pharmacy benefit.
Trends to watch, PBMI expects, are changes in cost-sharing policies, use of utilization and care management tools, and network/.site-of-care management to nudge people to more appropriate access channels.
The survey was conducted among 337 employers in September 2013.
Health Populi’s Hot Points: The good news for people who are sick is that biopharmaceutical pipelines are getting richer with possible treatments and cures for hard-to-tread conditions such as Alzheimer’s, a range of cancers, and diseases once-considered as “orphans” by general pharma companies.
As these therapies come onto the market, their marketers will face buyers armed with increasingly sophisticated tools to aggressively management utilization and the cost of acquiring these products. Once prescribed and adopter, these products will then be closely monitored for outcomes and site-of-use.
From the patient-consumer standpoint, as cost-sharing responsibility grows with out-of-pocket and coinsurance cost increases, more people will seek transparency in both clinical trial information, outcomes and pricing information. Patient social networks will be go-to places for some patients and caregivers to both access this information as well as learn from best-practices among fellow peer-patients. Check out SmartPatients for a model of how this is already working today.
Bio-pharma companies will also need to expand and streamline pharma access programs to make them accessible, helpful, easy-to-use destinations.
The opportunity for site-of-use is a positive development for patients-people as more convenient locations outside of “Pill Hill” and far-afield hospitals would benefit end-users and caregivers. PBMI found that lowest-cost sites of care were physician’s offices via specialty pharmacy, closely followed by the patient’s home. About one-third of health benefit designs currently incorporate incentives to encourage lower-cost sites of care to deliver specialty meds; this tactic will grow over time as patients and caregivers take on greater roles in self-care as their homes become the next medical home. As this role of the doctor’s office and home grow for site-of-specialty-pharma-care, so will shared-decision making between clinicians and patients.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...