 In 2017, Americans’ relationship with prescription drugs can be characterized in three ways: cost-rationing, misuse, and abuse.
In 2017, Americans’ relationship with prescription drugs can be characterized in three ways: cost-rationing, misuse, and abuse.
Three new studies about medicines in America paint this picture, brought to light by the AARP, Truven Analytics, and Quest Diagnostics.
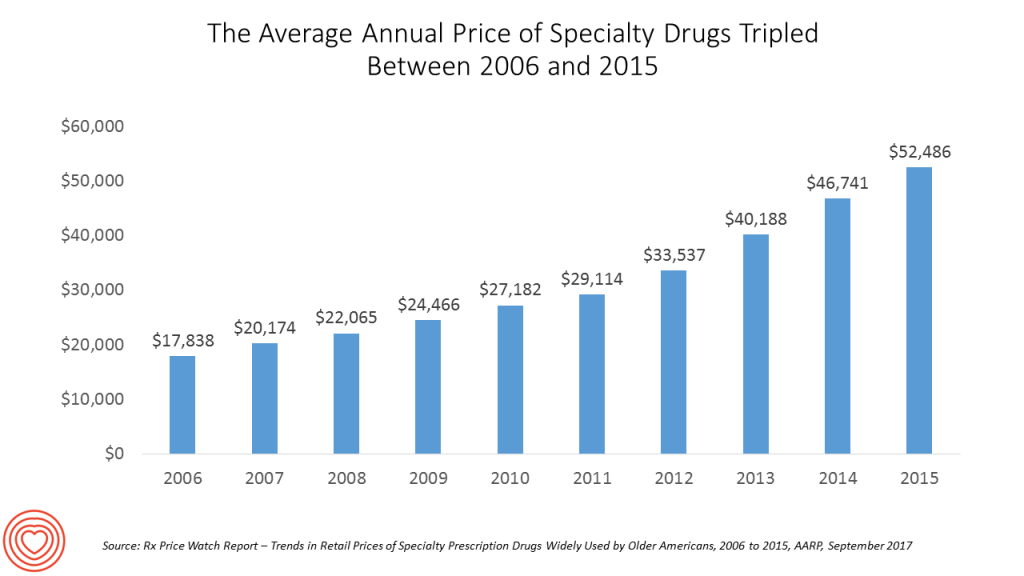
First, let’s look at the cost issue covered by AARP. AARP tracks the cost of prescription drugs among its constituents, namely people 50 years of age and over. The data were published in AARP’s Rx Price Watch Report, Trends in Retail Prices of Specialty Prescription Drugs Widely Used by Older Americans, 2006-2015. The average annual cost for one specialty medication used for a chronic condition was over $52,000 in 2015. That year, retail prices for 101 widely used specialty prescription drugs rose by 9.6%. This was 80 times faster than the rate of general inflation in the U.S. (which was 0.1%). Even older drugs’ prices, which had been on the market since 2006, increased cumulatively by an average of 177% over 10 years, when inflation increased 19.4%. Therapeutic drug categories with the highest price increases were for endocrine drugs (25%), DMARD (17%), Multiple Sclerosis (11%), Pulmonary Hypertension (11%), and Antipsoriatics (10%), all of which grew at least 10% between 2014-2015.
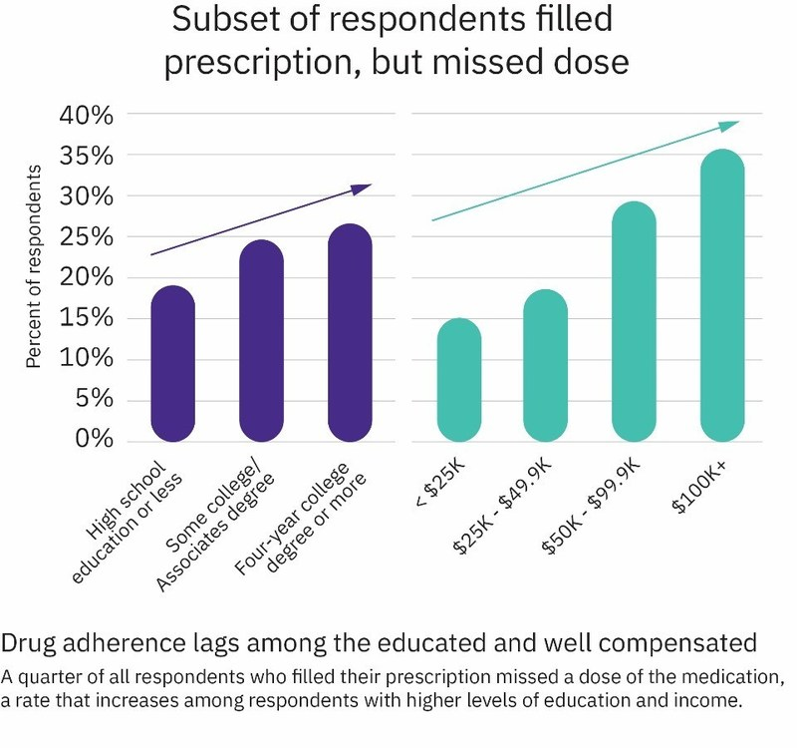
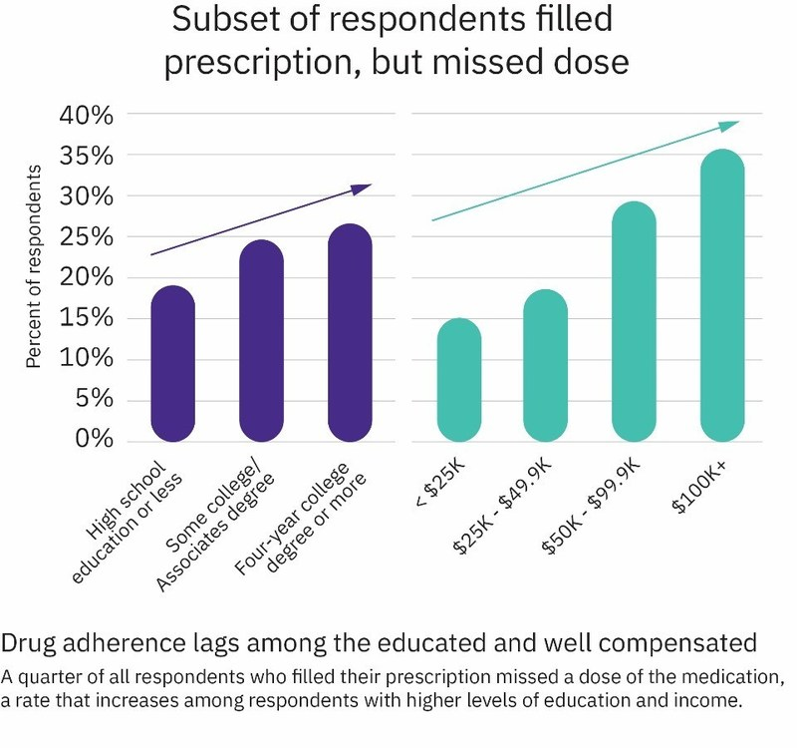 Truven Health Analytics, a unit of IBM Watson Health, published its Health Poll on Prescription Drugs last week in collaboration with NPR (National Public Radio). The top-line of the survey is that 1 in 3 Americans check the cost of a prescription drug before filling it. The surprise is that people with higher education and income are less-adherent to prescription drug regimens. This is illustrated in the second chart.
Truven Health Analytics, a unit of IBM Watson Health, published its Health Poll on Prescription Drugs last week in collaboration with NPR (National Public Radio). The top-line of the survey is that 1 in 3 Americans check the cost of a prescription drug before filling it. The surprise is that people with higher education and income are less-adherent to prescription drug regimens. This is illustrated in the second chart.
43% of people with income $100,000 and over check the cost of a medication before filling it, in contrast with 30% of people under $25K checking the cost and 29% of people earning $25-$49.9K a year checking the price.
While cost is the first reason a person won’t initially fill a prescription, patients’ drop-off from continuing a course of treatment happens due to side effects (29%), “didn’t need” it (17%), “felt better” (16%), “not working” (15%), and then cost (10%).
Cost as a factor for lack of adherence to a prescription drugs decreases with age: the older we are, the more likely we are to adhere to a drug regimen. Specifically, 64% of Millennials look for the cost of a medication before filling a prescription. Only 19% of people 65 and over check the price of a medication before filling it.
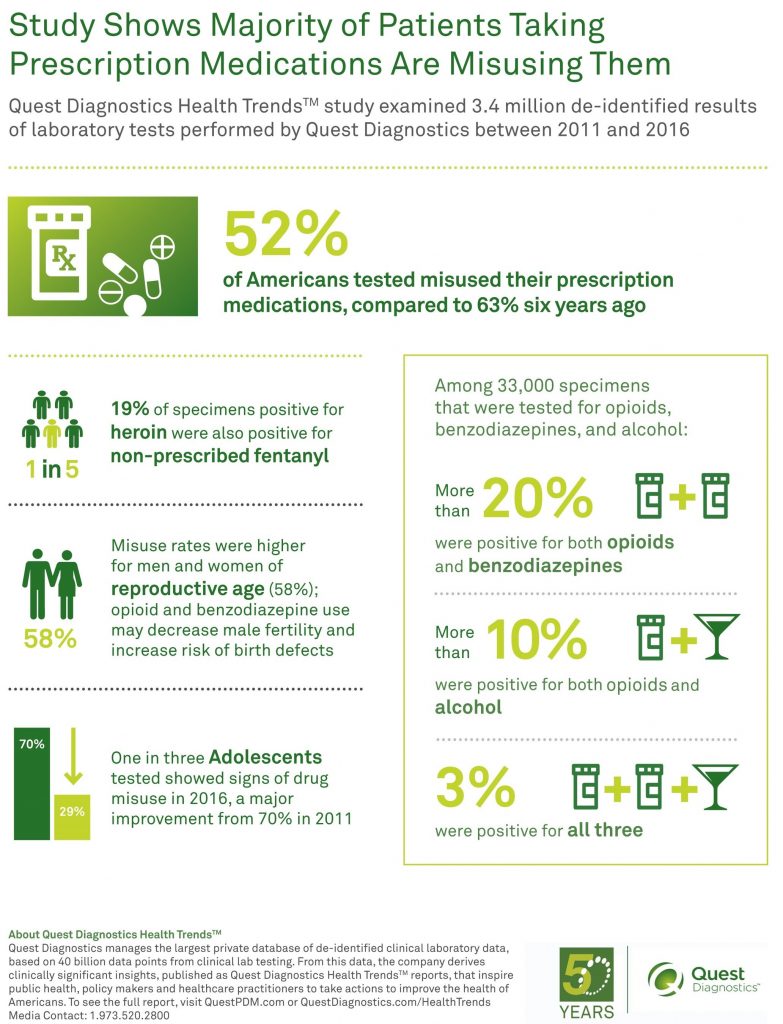
1 in 2 Americans misused prescription medications, based on Quest Diagnostics’ lab tests conducted among 3.4 million results between 2001 and 2016. On the upside, 1 in 3 adolescents tested showed signs of drugs misuse in 2016, down from 70% in 2011. Quest Diagnostics featured these findings in Prescription Drug Misuse in America: Diagnostic Insights in the Growing Drug Epidemic from Quest Diagnostics. The paper was published in concert with the PAINWeek 2017 meeting held last week in Las Vegas.
Quest learned that:
- 52% of patient lab tests showed signs of prescription drug misuse, down from 2011 when 63% of specimens tested for abuse. Quest points out that despite public health campaigns from both public and private sector messengers, misuse of prescription drugs continues to be prevalent.
- Drug misuse happens across age groups, genders, and people covered by all types of health plans — Medicare, Medicaid, and private plans alike.
- Dangerous drug combinations are common, crossing opioids, benzodiazepines, and alcohol. This implies that many people abusing prescription drugs are receiving prescriptions from at least one healthcare provider.
For historical context, I covered Quest Diagnostics’ study on prescription drug misuse last year here in Health Populi.
Health Populi’s Hot Points: Traditionally, the segment called “retail health” is long thought to include the front of the pharmacy where over-the-counter drugs are physically located. But increasingly, as patients take on more first-dollar costs for medicines that live behind-the-counter where the pharmacist stands, consumers confront sticker-shock. This becomes a retail moment-of-truth for the patient, now a consumer, who often makes a decision whether to fill, refill, or stick to a prescribed medicine based on its cost.
On the drug misuse/abuse part of the story, note that Quest Diagnostics found that prescription drug abuse happens across-the-board across men and women, all age cohorts (with adolescents misuse improving, thankfully), and across health plan types. This is evidence against the notion that the Affordable Care Act’s expansion of Medicaid has contributed to the opioid epidemic.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...