 Overtreatment is a major contributor to waste and patient risk in America. Most U.S. physicians say it’s a common fact of life in American healthcare, gleaned through physician survey detailed in Overtreatment in the United States, published in PLOS One on September 6, 2017.
Overtreatment is a major contributor to waste and patient risk in America. Most U.S. physicians say it’s a common fact of life in American healthcare, gleaned through physician survey detailed in Overtreatment in the United States, published in PLOS One on September 6, 2017.
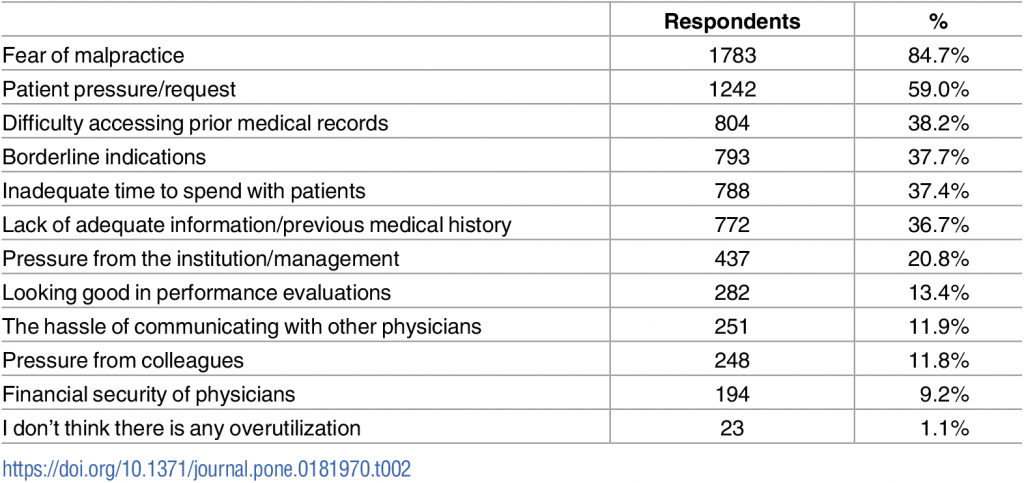
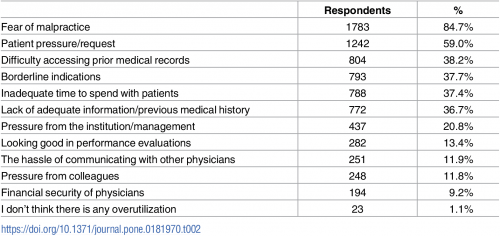
The overwhelming majority (8 in 10 physicians) identified malpractice as the reason for overtreatment, followed by patient pressure/request (59%). Other reasons cited for overtreatment included:
- Difficulty accessing prior medical records
- Borderline indications
- Inadequate time to spend with patients, and
- Lack of adequate information or previous medical history.
Overall, physicians judged 20% of healthcare to fall into the category of overtreatment. Doctors pointed to several key line items of overtreatment: 22% for prescription medications, 25% for medical tests, and 11% for procedures.
27% of physicians perceive that at least 30 to 45% of overall medical care is unnecessary.
Doctors offered several recommendations to stem overtreatment, including:
- Training medical residents on appropriateness criteria
- Providing easy access to outside health records
- Offering more practice guideline
- De-emphasizing fee-for-service bonus pay (while increasing base salaries).
While malpractice was cited, by far, as the #1 driver of overtreatment, the study’s authors note that the prevalence of malpractice lawsuits “may be greater than the reality of the problem.” Only two to 3% of patients harmed by negligence pursue litigation, the researches point out, of whom about one-half have received compensation. Furthermore, paid claims have fallen by nearly 50% in the last decade, with the growth of honest disclosure and physician apologies helping to mitigate litigation.
Health Populi’s Hot Points: In the nation where popular culture has valued supersizing, most patients still can’t distinguish between overtreatment, under-treatment, and that Goldilocks optimal ground of right-sized healthcare. I’ve covered this in Health Populi from its beginning ten years ago, as the issue is central to U.S. healthcare economics.
Here’s a recent post covering the consumer misperception challenge on overtreatment. That’s on the scale of an N=1 patient/consumer.
Now aggregate that, and you have a public health problem in 2 ways:
- More treatment means more risk for healthcare harm
- More treatment means wasted spending on care that could be otherwise allocated to another person who truly needs, but cannot access, the care.
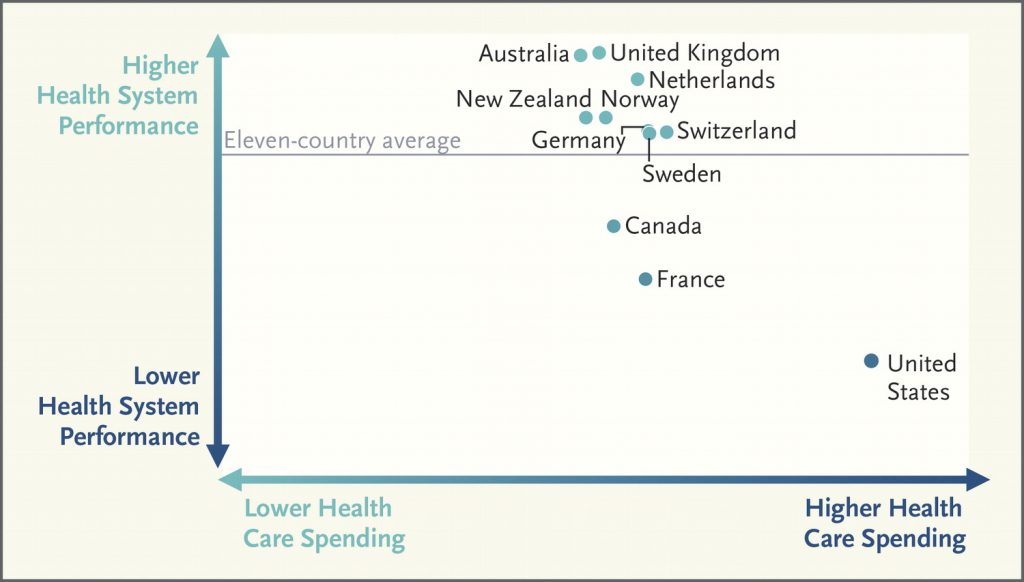 A perspective published last week in The New England Journal of Medicine begs the question, From Last to First — Could the U.S. Health Care System Become the Best in the World? The “Last” in the article’s title refers to reports from The Commonwealth Fund comparing Americans’ health outcomes and national spending to other wealthy countries’ health citizens and systems, where the U.S. fails to achieve their level of results. This low-ranking is shown in the second chart based on OECD data for 2014.
A perspective published last week in The New England Journal of Medicine begs the question, From Last to First — Could the U.S. Health Care System Become the Best in the World? The “Last” in the article’s title refers to reports from The Commonwealth Fund comparing Americans’ health outcomes and national spending to other wealthy countries’ health citizens and systems, where the U.S. fails to achieve their level of results. This low-ranking is shown in the second chart based on OECD data for 2014.
There are many reasons for the low-yield of high health spending in the U.S., among them lower investment in primary care (and front-end prevention) relative to specialty care, and lower per capita rate of social care spending, both of which you can explore here on Health Populi in previous posts.
But don’t underestimate the cost-increasing role that overtreatment plays in U.S. health over-spending. It’s a drag on the nation’s health system ROI, and a public health risk for patients.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...