Most consumers would be willing to try an FDA-approved app or online to treat a medical condition, as well as receiving hospital care at home if would be less costly.
We’ve reached an inflection point on the demand side among consumers for digital health options, PwC suggests in their report on the New Health Economy coming of age. The report outlines health/care industry issues for 2019, with a strong focus on digital health.
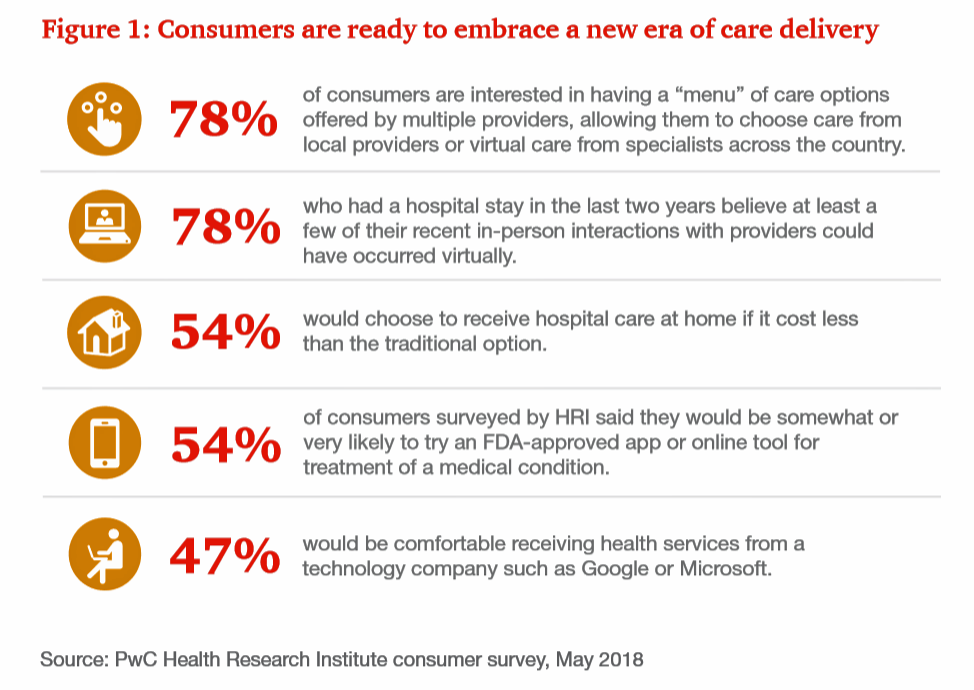
Whether a menu of care options including virtual health to access specialists across the U.S., post-hospital virtual visits, or hospital care at-home, a majority of Americans supports a new era of care delivery, as PwC coins the broad landscape of telehealth.
Nearly one-half of consumers also said they’d be comfortable receiving health services from a technology company like Google or Microsoft.
This is consistent with a previous survey by PwC’s firm Strategy& conducted several years ago which asked consumers what industries they would trust to help them manage their health. Equal proportions (39-40%) of people said, “large retailers,” “digitally-enabled companies,” and “healthcare providers.”
Comfort with tech companies getting involved in health care services is now a viable scenario in health consumers’ minds, for nearly 50% of people.
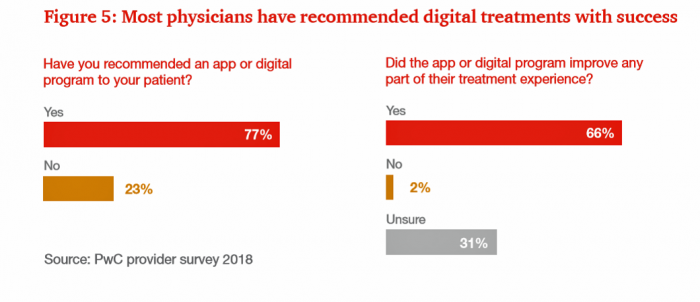
PwC also notes that most physicians (3 in 4) have recommended an app or digital tool to patients. Two-thirds of these digital tool “prescriptions” (small “p”) have been met with success, the prescribers say.
This statistic also demonstrates a new tipping point and convergence between health consumers and their doctors, which has been a chasm for a while. I discussed this digital health supply/demand gap here in Health Populi.
Note that 31% of physicians were unsure about the results of their digital tool prescribing. We need better metrics to quantify this kind of encounter that will provide evidence for tools that work in consumers’ self-help hands, and those that don’t.
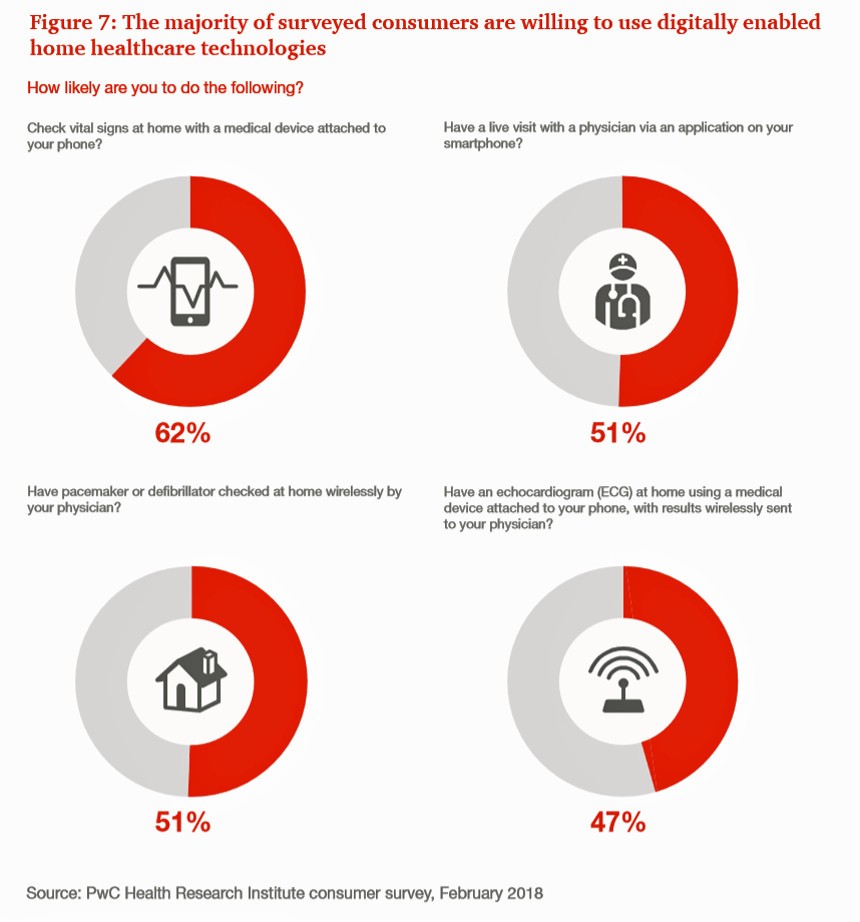
As patients-as-consumers grow more comfortable with telehealth, remote health monitoring and using consumer-facing digital health tools, they’re also envisioning the possibility and viability of more medical area at home.
Most people would be willing to use a medical care tool at home, such as those that check vital signs with a device attached to a phone; having a live visit with a physician via an app; checking their implanted medical device, like a pacemaker or cardiac defibrillator “long-distance” wirelessly by a physician; or, having an ECG at home using a device attached to their phone, communicating results to their physician.
These statistics from PwC’s health consumer surveys are underpinned by a key finding: most consumers are interested in an FDA-approved digital app or tool to treat a medical condition.
One-half of consumers would be likely to try such an FDA-cleared device. And again, most doctors told PwC they’ve brought up the subject of such digital therapies to patients, and 26% of patients have raised up the topic with their doctors.
Health Populi’s Hot Points: A column in JAMA published January 11, 2019 discusses Personal Health Records: More Promising in the Smartphone Era?
Dr. Christian Dameff and colleagues from UC-San Diego answer the question by saying, yes, PHRs are indeed more promising in this smartphone era with the advancement and adoption of FHIR standards that help make electronic health records more inter-operable. These standards are complemented by advances in internet-connected consumer devices that allow patients to collect personal biometric and other clinical data from well-designed wearable tech and remote health monitors. Technology companies beyond traditional health IT, such as Apple, Google, and Samsung among others, are advancing some of these applications.
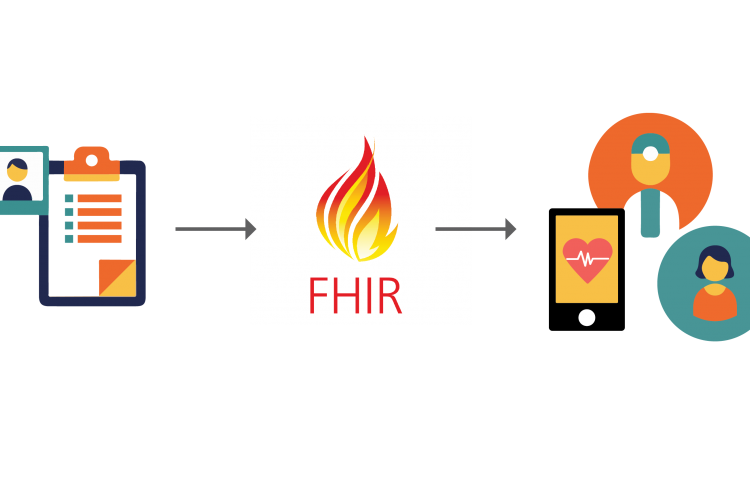 Fostering the adoption of FHIR standards in healthcare beyond academic medical centers will be really important to bring virtual and technology-enabled self-care to mainstream patients dealing with the chronic conditions that are amenable to lifestyle and behavior changes — say diabetes, heart disease, and respiratory diseases like asthma and COPD, all of which have a growing assortment of better-and-better designed digital health tools that can be used by consumers.
Fostering the adoption of FHIR standards in healthcare beyond academic medical centers will be really important to bring virtual and technology-enabled self-care to mainstream patients dealing with the chronic conditions that are amenable to lifestyle and behavior changes — say diabetes, heart disease, and respiratory diseases like asthma and COPD, all of which have a growing assortment of better-and-better designed digital health tools that can be used by consumers.
The authors conclude, “whether these technological advances ultimately improve patient outcomes, lower costs, and improve quality remain the most important unanswered questions.”
As clinicians and consumers join forces to take healthcare home, it’s incumbent on everyone to assess to measure these experiences in this early adoption phase. We’ll need to crowdsource and share findings from these studies to gauge what works. This will help pay-it-forward for future patients and doctors in helping forge more efficient and cost-effective health care, as well as high consumer-grade experiences.
We’ll be discussing the consumerization of digital health technologies on Valentine’s Day at HIMSS, 14th February 2019, during an all-day session hosted by Dr. Joe Kvedar and the Personal Connected Health Alliance. At 10:15 am that day, I’ll be on a panel with Greg Orr, VP of Digital Health with Walgreens; Nick Desai, President of Heal; and, Peter Rasmussen, Medical Director of Digital health at the Cleveland Clinic, focusing on digital traction in the consumerization of healthcare.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.