 Some one in three physicians is burned out, according to the Medscape’s National Physician Burnout & Suicide Report. The subtitle, “The Generational Divide,” tells a bit part of the subtext of this annual report that’s always jarring and impactful for both its raw numbers and implications for both patient care and the larger health care system in America.
Some one in three physicians is burned out, according to the Medscape’s National Physician Burnout & Suicide Report. The subtitle, “The Generational Divide,” tells a bit part of the subtext of this annual report that’s always jarring and impactful for both its raw numbers and implications for both patient care and the larger health care system in America.
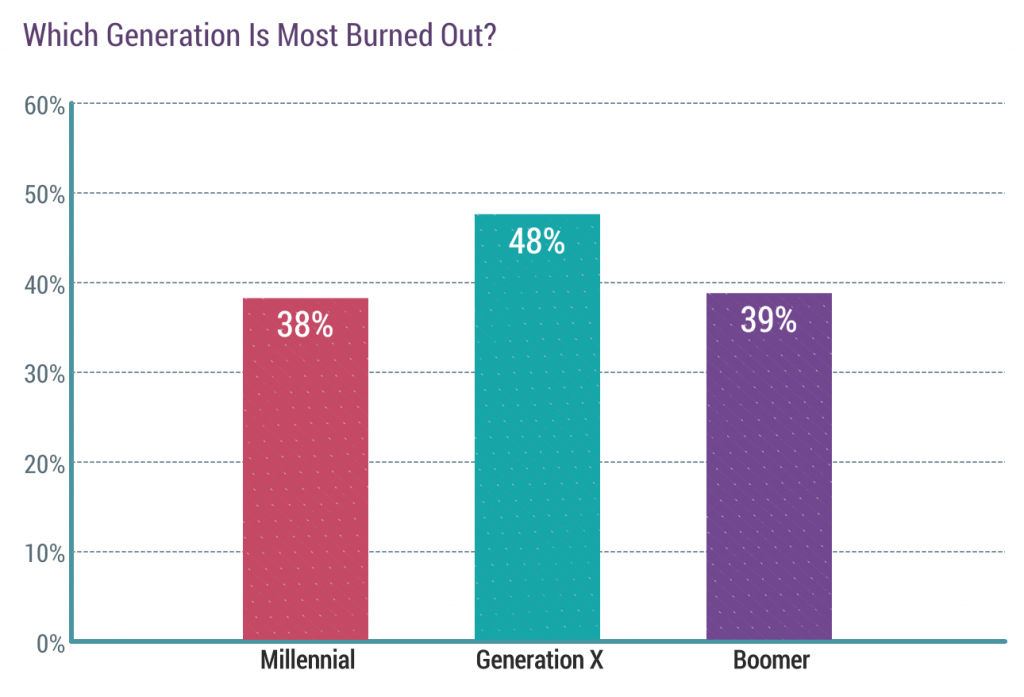
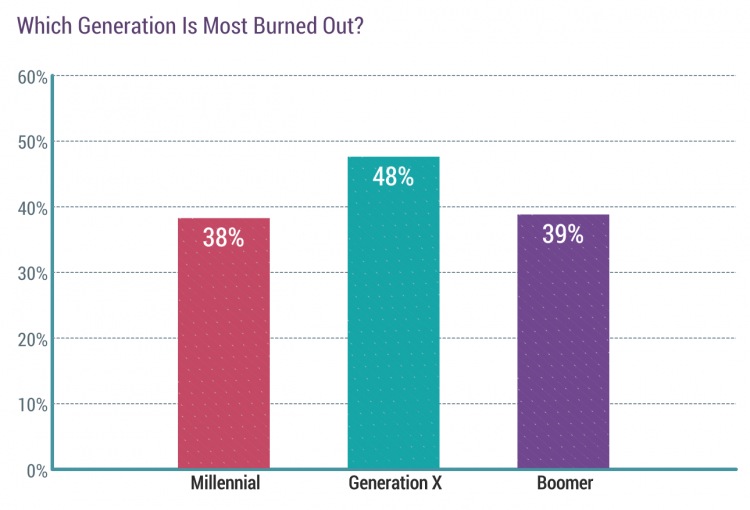
Nearly 1 in 2 physicians in Generation X, those people born between 1965 and 1979, feel burned out compared with roughly 4 in 10 doctors who are Millennials or Boomers.
Furthermore, many more women than men physicians feel burned out: 48% of female doctors versus 37% of male.
Beyond generational differences shown in the first bar chart, feeling burned out also varies by specialty. This year, the greatest levels of burn-out are felt by the urologists, neurologists, nephrologists, endocrinologists, family doctors, radiologists, OBGYNs, rheumatologists, and infectious disease specialists.
Least likely to feel burned out are public health and preventive medicine doctors, ophthalmologists, orthopedists, psychiatrists, ENTs, and general surgeons.
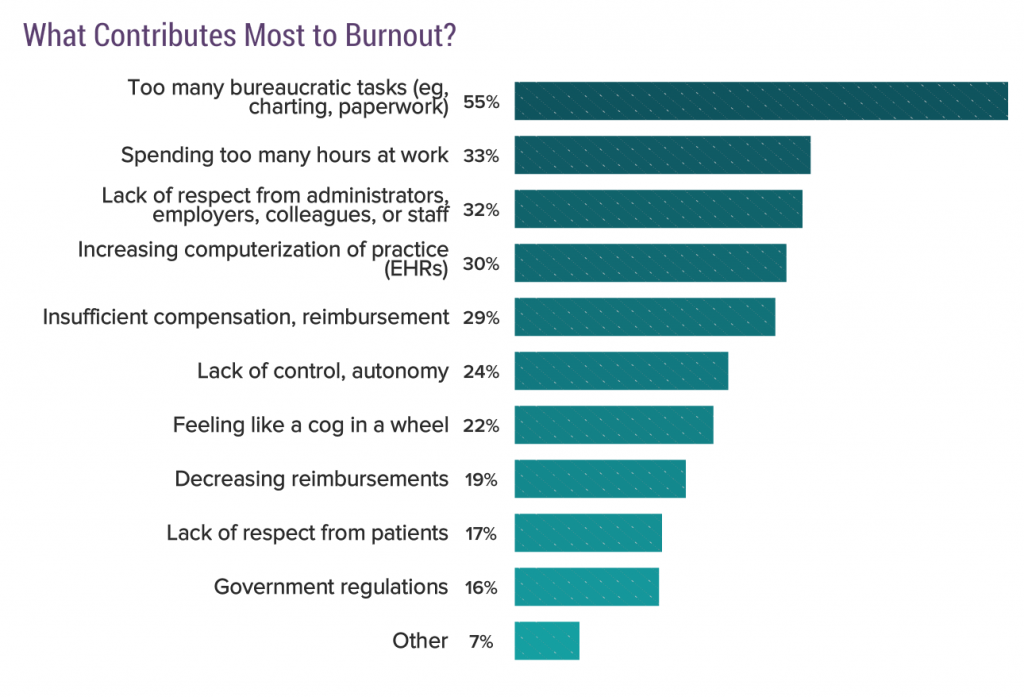 What contributes most to burnout, doctors told Medscape, was by far onerous bureaucratic tasks — paperwork, charting, and lack of time for hands-on patient care.
What contributes most to burnout, doctors told Medscape, was by far onerous bureaucratic tasks — paperwork, charting, and lack of time for hands-on patient care.
Bureaucracy is followed by too much time at work, lack of respect at the workplace, increasing computerization of practice (read: EHR impacts), and insufficient compensation or reimbursement.
Lack of control or autonomy, and “feeling like a cog in a wheel,” are burnout risks for over 1 in 5 doctors.
Bureaucracy contributes to burnout fairly equally across the generations, but the second key risk factors for burnout vary by generation: for Millennials, it’s too much time at work; for Gen X, it’s lack of respect from colleagues at work; and, for Boomers, guess what? It’s EHR implementation and the computerization of practice.
 For the majority of doctors who feel burnout, it’s had a negative impact on relationships for over two-thirds of Boomers, and 3 in 4 Millennials and Gen X doctors.
For the majority of doctors who feel burnout, it’s had a negative impact on relationships for over two-thirds of Boomers, and 3 in 4 Millennials and Gen X doctors.
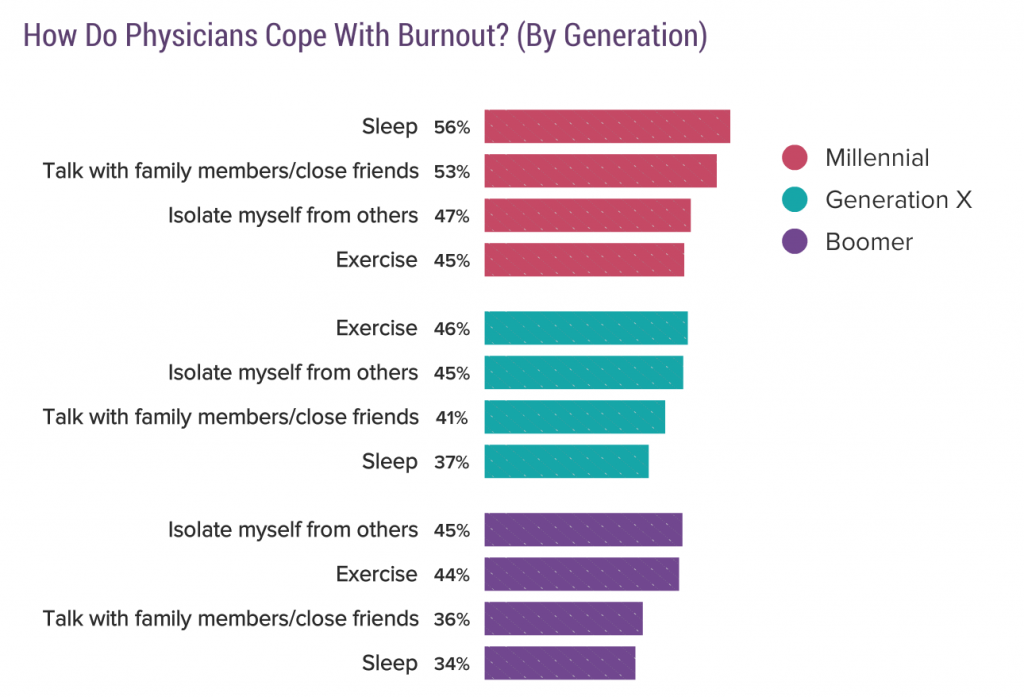
Doctors cope with burnout differently by generation, too: more Millennials look to sleep more and talk with family and friends; more Gen X doctors exercise and isolate themselves from others to deal with burnout; and, among Boomers, isolation and exercise are the go-to strategies for burnout management.
Fully one-third of doctors overall are unhappy with their work life, roughly the same proportion across generations.
And, roughly the same proportion, between 15% and 18%, of doctors say they are depressed. Two-thirds of physicians have not felt suicidal, but one in five doctors has thought of suicide — but not attempted it.
Medscape surveyed 15,181 physicians across 28 specialists in June through September 2019 to gauge clinicians’ perspectives on burnout and depression for this study.
 Health Populi’s Hot Points: Clearly, there are differences across generations regarding physicians recognizing their level of burnout and depression, as well as variations in those clinicians seeking support for their state of mental health. It’s the gender chasm in this year’s Medscape study that needs further explication.
Health Populi’s Hot Points: Clearly, there are differences across generations regarding physicians recognizing their level of burnout and depression, as well as variations in those clinicians seeking support for their state of mental health. It’s the gender chasm in this year’s Medscape study that needs further explication.
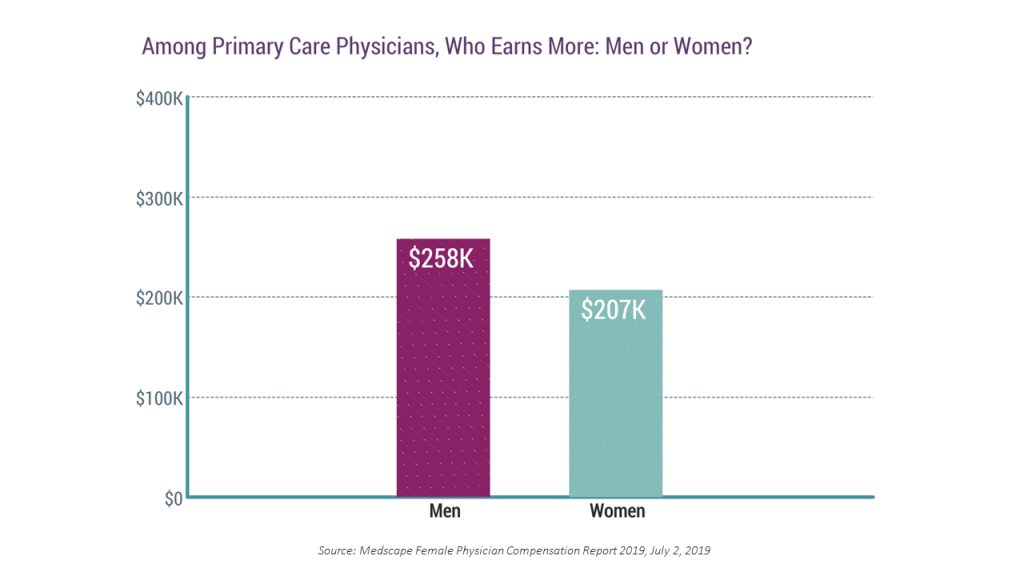
Women in the U.S. earn less than men do in the same occupations, and that includes physician salaries as well as other jobs in America. Medscape’s 2019 Female Physician Compensation Report calculated that female primary care physicians (PCPs) earned roughly 20% less than their male colleagues in 2019 — that is, $207,000 for women compared with $258,000 for men in primary care.
 Note that more women than men would take a salary reduction to achieve better work-life balance, Medscape found. Taking this trade-off in real life would put women at an even greater financial disadvantage than men, where women would give up income to find more time and energy for other aspects of their life.
Note that more women than men would take a salary reduction to achieve better work-life balance, Medscape found. Taking this trade-off in real life would put women at an even greater financial disadvantage than men, where women would give up income to find more time and energy for other aspects of their life.
Doing so could help address the work/life balance issue in itself. But trading off salary for time could then compromise another aspect of life that contributes to stress — financial wellness, where Nationwide’s Women and Retirement research learned that women over the long-term have worse fiscal health as they (1) outlive men and (2) have saved less money than men have due to the wage differential they faced through their lifetime of work and/or home-keeping.
Physician burnout and depression compromise health care delivery in America. We must recognize that physicians are also patients, stressed as so many people are — at work, at home, in society, in personal finances. Reducing the taboo around mental health for all people helps everyone in the health/care ecosystem. So will expanding services at the workplace, and giving people greater flexibility in doing our jobs, both for men and women at work. This is particularly, heart-breakingly crucial for health care systems in confronting, eyes wide open, the challenge of the Quadruple Aim.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...