“Digital technologies offer tremendous potential for shifting from traditional medical routines to remote medicine,” with the role of wearables playing a growing role in the new home care for healthy aging.
But what are the challenges of deploying this promising tech with older people keen to be independent at home? We learn a lot about prospects and challenges in Digital health for aging populations, a Perspective report in Nature Medicine‘s July 2023 issue.

An experienced team affiliated with the University of California San Diego shares their insights in this essay, which first lays out the portfolio of technologies and devices for health monitoring in older adults.
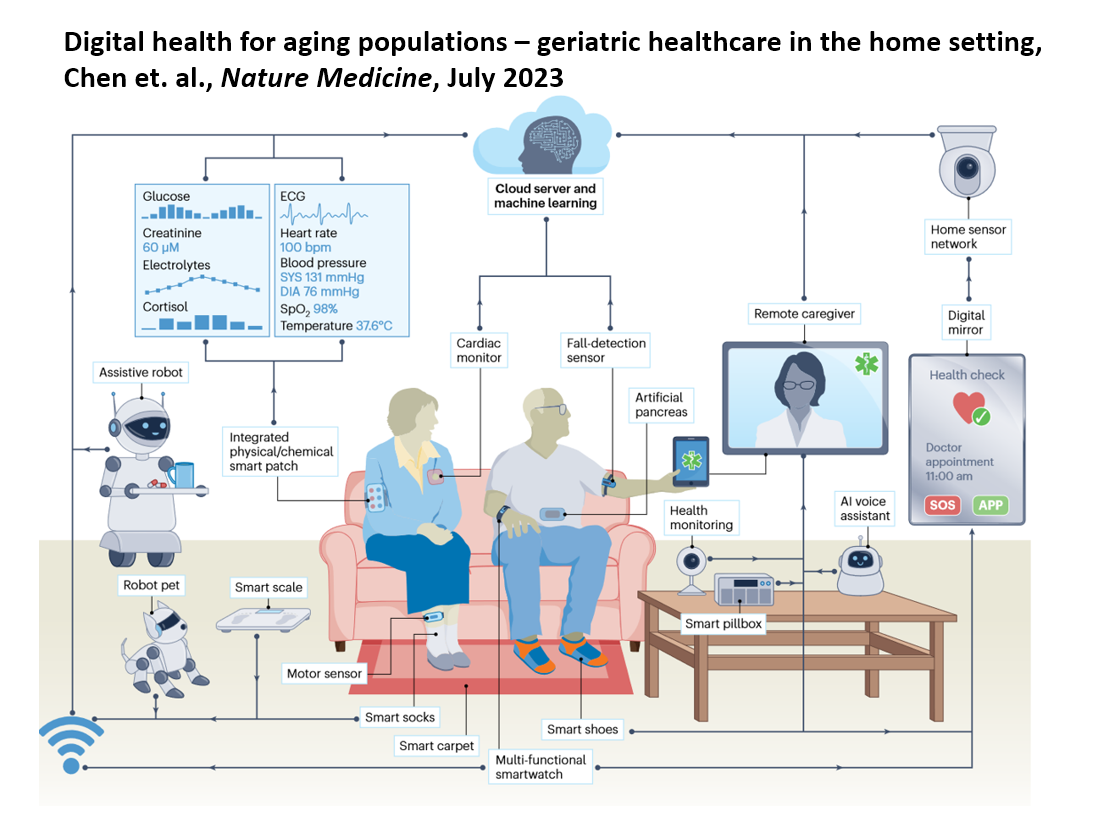
These are illustrated in the first graphic here snapped from the article, noting that wearable sensors have rapidly evolved since the emergence of the Internet of Things (IoT) and mobile devices — think Fitbit’s early days to smart socks and shoe-soles, the Oura ring and blood pressure reading from the wrist.
In addition to vital signs, these devices can monitor mobility and activity-related signals, assess gait disorders for patients with Parkinson’s disease, and anticipate early onset of cardiovascular disease.
The essay discusses sensors by category, covering wearable physical sensors, wearable chemical sensors, hybrid and multi-parameter sensing platforms, and non-wearable sensors (think: smart home digital systems that can sense behavior, posture, and movement of people at home.
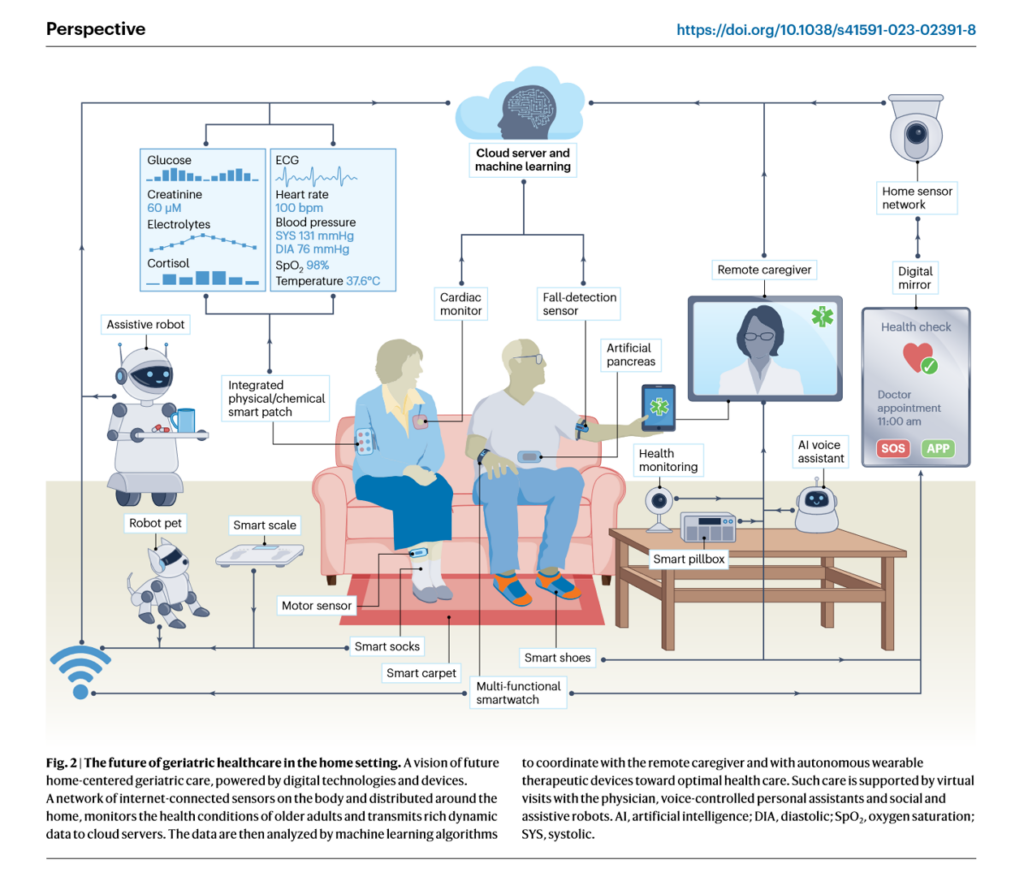
Figure 2 shown here from the report illustrates one scenario of a smart home for older people, with an infrastructure of a wireless communication network and cloud analytics platform over which various sensors (wearable and non-) and Internet of Things connected devices generate data based on residents’ behaviors and clinical signals.
Note the assistive robot, a remote caregiver screen for telehealth support, a digital mirror, and even a robot pet for social interaction and well-being/
The researchers identify a range of “challenges to clinical translation,” such as digital literacy skills, data privacy and security threats, and limited device performance in the current generation of these things.
How to overcome the challenges? Here are some of the team’s thoughts:
- Design with older adults in mind – “engaging with older adults and seeking their input on design and operation of these digital devices would be the best way to understand user needs and achieve this goal”
- The migration from active to passive sensors can help in this translation and migration
- Address data processing and security, acknowledging that the current systems cannot cope with the exponential growth of data and volumes generated by all of these sensors and devices. Attend, to, to peoples’ concerns about privacy and security such as the risk of remote hacking and control of the devices; data processing and security pose a greater challenge for older people due to digital literacy and/or cognitive aging issues
- Solve for performance gaps and challenges in the technologies: for example, the current state of wearable chemical sensors that still have limited stability, accuracy, and too-narrow scope, the authors note. Continuous improvements for the devices should fill the performance gaps to be able to transform geriatric care, they believe.
- Finally, accessibility and cost of devices and services cannot be assumed away: the economic burden poses financial challenges for older people who tend to live on fixed incomes, and in lower-income countries an even larger financial burden.
The authors are bullish on the role of digital tech for aging at home–with the provisos that user-centered design, filling in technology gaps, and assuring financial access to the promises of these devices and smart home environments are part of the planning.
Health Populi’s Hot Points: From the American Medical Association to 7Wire Ventures, influential voices in the health/care ecosystem are firmly focused on the growing role of peoples’ homes for healthy and safe aging.
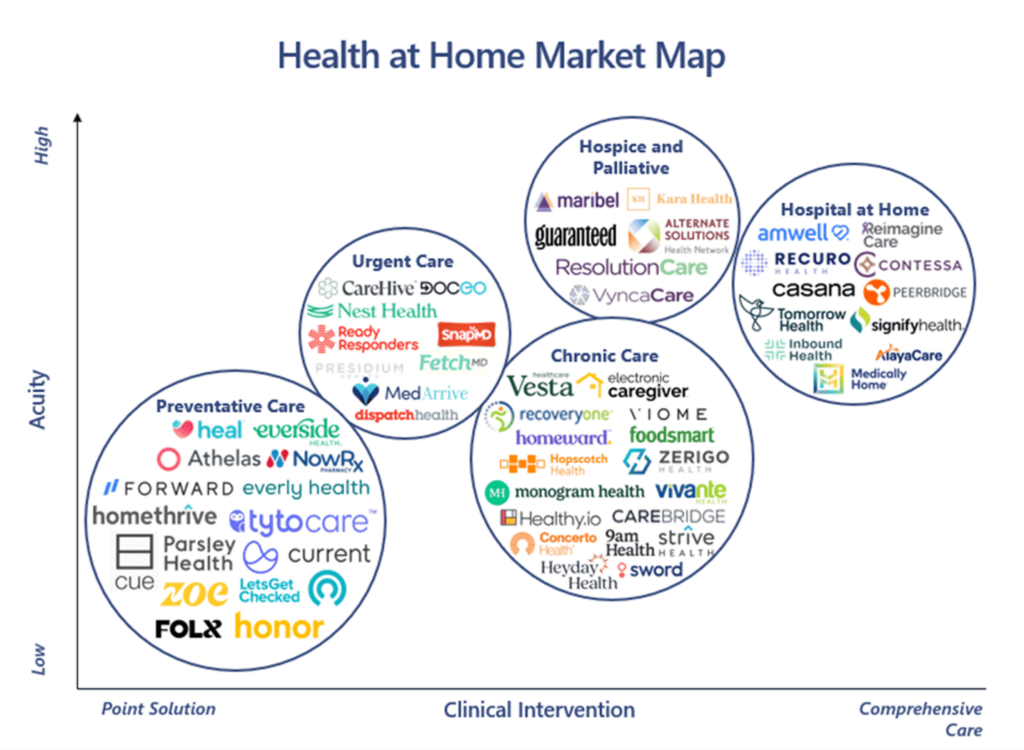
The Health at Home Market Map here was featured in 7Wire Ventures’ write-up on our homes as our medical homes, and inventories some of the key categories of digital technologies for care in consumers’ residences.
In considering the scenario above of people aging, living and loving at home over time, it occurs to me that we are all “aging at home,” every day…..every health citizen wants to be well, and stay well, for as long as possible, to thrive at whatever age they’re in.
At any point in time, each of us could need hospital-at-home services, after dealing with a sports/athletic accident or injury, an acute episode, or confronting and managing end-stage illness.
The lessons the UCSD authors raise in the challenges for digital health at home are as relevant to younger people below AARP age (that is, 50) as they are to people 51 years of age and older. Health happens at home for all of us. And even the most digitally-native consumers may not know how to navigate the healthcare system as nimbly as their grandparent does.
Thanks to Chuanrui Chen, Shichao Ding and Joseph Wang for shedding bright light on the topic of digital health for aging — for all of us.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...