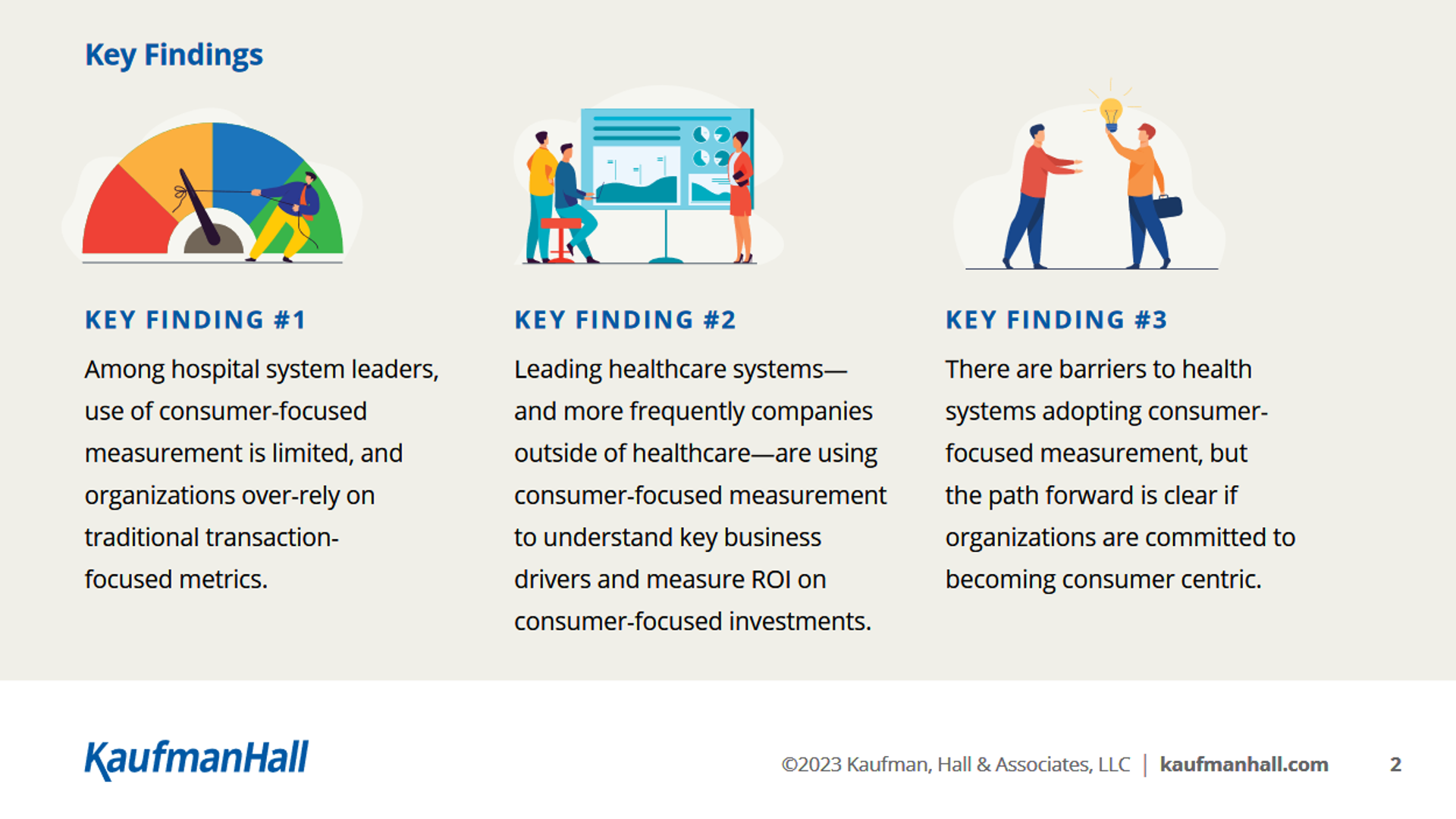
While there are barriers preventing health systems and care providers from adopting consumer-focused measures for patient experience, those who have deployed these metrics can provide solid role models for advancing consumer-centered care.
Welcome to Kaufman Hall’s eighth annual study culminating in the 2023 State of the Healthcare Consumer Report. This year, the report’s subtitle “Measuring What Matters” speaks to the importance of achieving an ROI on consumer-facing investments while facing real, pragmatic headwinds such as cost and margin management and staffing pressures, among other forces that can stifle investments in new-new things.
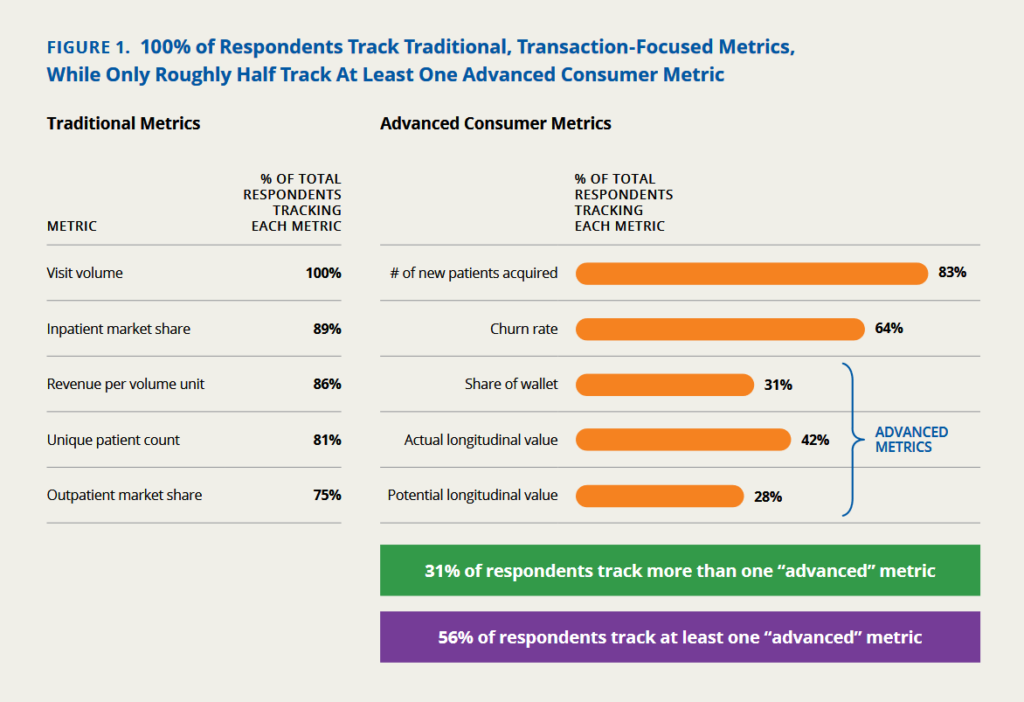
Over the years of conducting this research and working with clients in the field, Kaufman Hall has developed a portfolio of advanced consumer metrics that have evolved out of the more traditional metrics like visit volume, market shares, and revenue per volume unit.
Clearly, the traditional metrics are married to volume-based payment.
The advanced consumer metrics have more to do with relationship value — number of new patients acquired to start, then share of wallet over time and longitudinal value of the patient relationship.
One in three health system respondents have begun to track more than one of these advanced metrics.
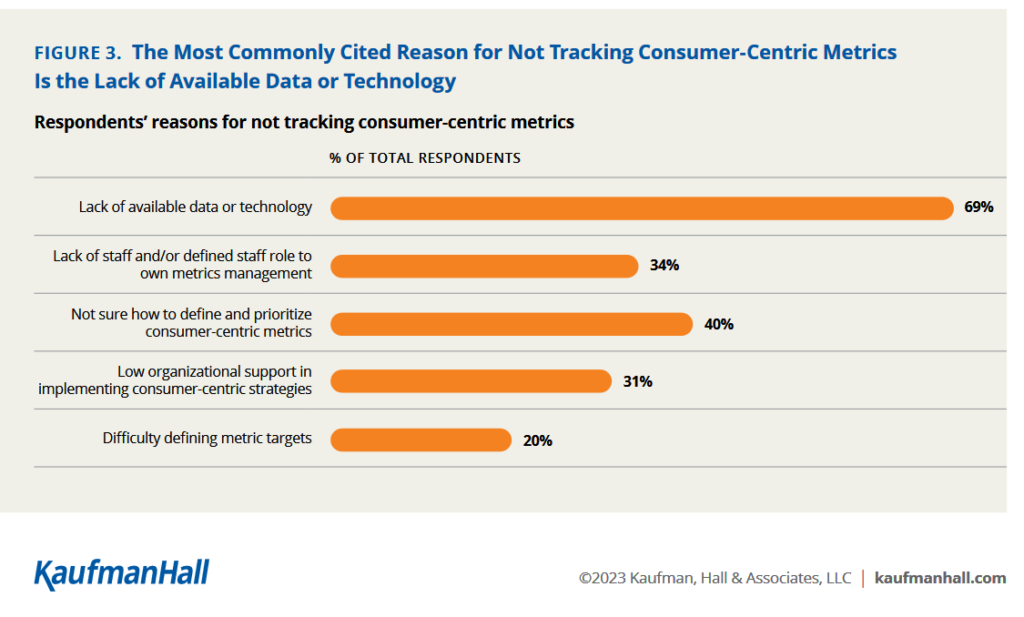
So why don’t more health systems track the consumer-centric metrics? By far the leading obstacle is lack of available data or technology, followed by uncertainty in how to define the consumer-oriented measures and lack of staff/roles to do so.
“Consumers vote with their feet and their smartphones. Health systems that track consumer-centric, relationship-focused metrics and use the resulting insights to transform their businesses will be in the best position to capture their loyalty and the high
lifetime healthcare spend of each individual consumer.
That led Kaufman Hall to conclude the 2023 report with 5 benefits of a consumer-centric, relationship-driven model — the fifth of which is, “Improved ability to compete with potential disrupters.” This point should be well-taken seriously by health care providers and plans, and other touchpoints in the larger health/care ecosystem. We can’t blink in 2023, and beyond, in trying to keep track of those “disrupters” partnering with health system incumbents: note announcements from the past few weeks such as…
- Best Buy Health collaborating with Mass General Brigham
- Amazon Prime discounting subscriptions to One Medical for hybrid primary care as well as a new partnership with CommonSpirit Health’s Virginia Mason Franciscan Health for specialty care in greater Seattle
- Walmart collaborating with Orlando Health for care coordination, and,
- Instacart growing its food-as-medicine program in alignment with providers and advocacy groups, among many others.
Health Populi’s Hot Points: Change in health care is always hard, so starting with a clear True North objective can help align different internal organization stakeholders on the same page. Here, I’ve circled the #3 task of Kaufman Hall’s recommendations on “Where to Begin.”
If we focus, together, on an “operating model shift” mindset firmly set on the consumer experience of access, that could be a useful cognitive therapy tool for a team looking to evolve toward consumer-centricity.
This feels like a powerful, empowering choice to me because “Access” has many facets when we’re speaking about patient/consumer centricity. Access can relate to…
- An on-ramp into a health system or provider organization through a “real” or digital front door, portal, or app
- Cultural-literacy accessibility, from language to cultural mores and social norms for a particular group of patients
- Financial access for, say, a specialty prescription drug or ability to pay for a procedure under a high-deductible health plan
- Trust as a precursor to health engagement,
and so on.
With that in mind, I’ll revisit one of the most important publications that continues to inform and nudge me when brainstorming consumer-centered design in health care across the health care ecosystem — whether in conversations with health plans, payers, technology innovators, life science companies and providers…
Value-based payments require valuing what matters to patients.
Check this out in JAMA and don’t fret about the publication date being well over 8 years ago….it’s a classic and prescient when it was published.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...