 Of the $2.4 trillion spent on health in the U.S., 75% goes to Americans with chronic conditions like diabetes, heart disease, and asthma. One reason so much resource flows toward chronic disease is that too many patients aren’t engaged with their own health. For example, more than 20% of first-time prescriptions that treat chronic conditions have never been filled, according to a study in the April 2010 Journal of General Internal Medicine, Primary Medication Non-Adherence. Non-adherence was found to be particularly high for patients diagnosed with diabetes, high blood pressure, and high cholesterol.
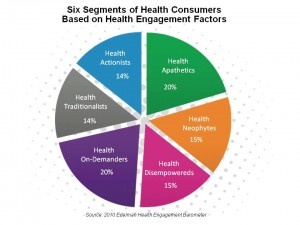
The 2010 Edelman Health Engagement Barometer surveyed 5,000 Americans and thousands of other health citizens throughout the world, who clustered into six group based on similar attitudes, behaviors, and demographics. The six segments are:
Health Actionists, the most highly health-engaged group who not only pay attention to their own health, but are health-influencers over other people in their lives
Health Traditionalists, who engage with the health system in Old School ways
Health On-Demanders, who quickly engage with health care when they’re diagnosed
Health Disempowereds, who have chronic conditions but are confused by much of the health information they confront and generally stressed
Health Neophytes, who tend to be younger and uninvolved with the health system
Health Apathetics, who are the least likely to take care of themselves and share opinions about health with others.
Edelman’s poll found that for each of these segments, information alone doesn’t motivate people even the most engaged Health Actionists to take on healthy behaviors. It’s a combination of information plus a connection to a loved one plus a life moment (from becoming a parent to losing one, getting married or learning about a personal health risk).
Of the $2.4 trillion spent on health in the U.S., 75% goes to Americans with chronic conditions like diabetes, heart disease, and asthma. One reason so much resource flows toward chronic disease is that too many patients aren’t engaged with their own health. For example, more than 20% of first-time prescriptions that treat chronic conditions have never been filled, according to a study in the April 2010 Journal of General Internal Medicine, Primary Medication Non-Adherence. Non-adherence was found to be particularly high for patients diagnosed with diabetes, high blood pressure, and high cholesterol.
The 2010 Edelman Health Engagement Barometer surveyed 5,000 Americans and thousands of other health citizens throughout the world, who clustered into six group based on similar attitudes, behaviors, and demographics. The six segments are:
Health Actionists, the most highly health-engaged group who not only pay attention to their own health, but are health-influencers over other people in their lives
Health Traditionalists, who engage with the health system in Old School ways
Health On-Demanders, who quickly engage with health care when they’re diagnosed
Health Disempowereds, who have chronic conditions but are confused by much of the health information they confront and generally stressed
Health Neophytes, who tend to be younger and uninvolved with the health system
Health Apathetics, who are the least likely to take care of themselves and share opinions about health with others.
Edelman’s poll found that for each of these segments, information alone doesn’t motivate people even the most engaged Health Actionists to take on healthy behaviors. It’s a combination of information plus a connection to a loved one plus a life moment (from becoming a parent to losing one, getting married or learning about a personal health risk).
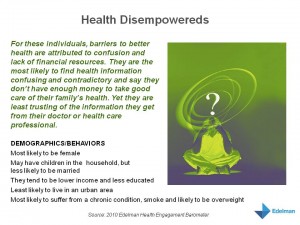 Health Populi’s Hot Points: Health engagement underpins healthy outcomes. Take the Health Disempowereds: were organizations who provide health care, market health services and products, and sell health insurance to crack the code on engaging this segment, outcomes would improve, costs could be tamed (across the overall system), and we’d be singing Kumbayah.
Not so fast: the Health Disempowereds, representing about 1 in 6 health citizens, tend to be diagnosed with chronic conditions, overweight, and smoke more than average. So they need health care and counsel. But they also don’t generally trust doctors or the health establishment. They’re also somewhat befuddled by available health information. What to do?
A key finding from the Barometer provides some creative food for thought when it comes to reaching the Health Disempowereds. Think about the fact that, while this cohort generally isn’t too keen to receive health information from doctors in whom they lack trust, they’re still living lives 24×7 outside of the doctor’s office. They work, they shop, they tend to live outside of urban centers. I bet they tend to shop in Big Box stores. Many of them are also self-described as overweight, so they may also frequent fast food restaurants and grocery stores. These retail and food destinations become important channels for health communication and decision-making at the point-of-purchase.
Beyond food choices and filling prescriptions, the other micro-decisions people make 24×7 contribute mightily to their health status. Jen McCabe, a particularly bright light on the Health 2.0 scene, has started up Get Up and Move, a “microfitness revolution” as she and her partner call it. Get Up and Move is a technology platform, via Twitter and Facebook, that provides social support for people who sign onto the group. Jen has said that behavior change over time can take from 18 to 260 days or longer, depending on ‘who’ you are: your personality, your state of mental and physical fitness, and the other personal baggage we all carry around.
So Edelman found that information isn’t enough. And Jen McCabe has learned and is teaching us that socializing physical movement can be a crucial part of health behavior change. For Health Disempowereds, this can be one piece of the complex, long and winding journey toward health empowerment.]]>
Health Populi’s Hot Points: Health engagement underpins healthy outcomes. Take the Health Disempowereds: were organizations who provide health care, market health services and products, and sell health insurance to crack the code on engaging this segment, outcomes would improve, costs could be tamed (across the overall system), and we’d be singing Kumbayah.
Not so fast: the Health Disempowereds, representing about 1 in 6 health citizens, tend to be diagnosed with chronic conditions, overweight, and smoke more than average. So they need health care and counsel. But they also don’t generally trust doctors or the health establishment. They’re also somewhat befuddled by available health information. What to do?
A key finding from the Barometer provides some creative food for thought when it comes to reaching the Health Disempowereds. Think about the fact that, while this cohort generally isn’t too keen to receive health information from doctors in whom they lack trust, they’re still living lives 24×7 outside of the doctor’s office. They work, they shop, they tend to live outside of urban centers. I bet they tend to shop in Big Box stores. Many of them are also self-described as overweight, so they may also frequent fast food restaurants and grocery stores. These retail and food destinations become important channels for health communication and decision-making at the point-of-purchase.
Beyond food choices and filling prescriptions, the other micro-decisions people make 24×7 contribute mightily to their health status. Jen McCabe, a particularly bright light on the Health 2.0 scene, has started up Get Up and Move, a “microfitness revolution” as she and her partner call it. Get Up and Move is a technology platform, via Twitter and Facebook, that provides social support for people who sign onto the group. Jen has said that behavior change over time can take from 18 to 260 days or longer, depending on ‘who’ you are: your personality, your state of mental and physical fitness, and the other personal baggage we all carry around.
So Edelman found that information isn’t enough. And Jen McCabe has learned and is teaching us that socializing physical movement can be a crucial part of health behavior change. For Health Disempowereds, this can be one piece of the complex, long and winding journey toward health empowerment.]]>
Empowering disempowered people in health care: information isn't enough
By Jane Sarasohn-Kahn on 25 May 2010 in Demographics and health, Health Consumers, Health engagement, Public health




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.