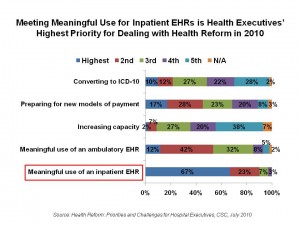
 Meeting meaningful use for inpatient EHRs is the top priority among the many challenges health executives face when considering how the Patient Protection and Affordable Care Act (PPACA) will impact their organizations. Overall, 2 in 3 health execs place MU for inpatient EHRs as the “highest priority;” among health IT executives, the proportion citing this as the highest priority is 84%.
Meeting meaningful use for inpatient EHRs is the top priority among the many challenges health executives face when considering how the Patient Protection and Affordable Care Act (PPACA) will impact their organizations. Overall, 2 in 3 health execs place MU for inpatient EHRs as the “highest priority;” among health IT executives, the proportion citing this as the highest priority is 84%.
The second-most pressing PPACA priority for health executives is preparing for new models of payment, cited by 17% of health execs overall, and 31% of non-IT executives.
CSC surveyed health executives in July to gauge their temperatures on several PPACA line-items including meeting meaningful use for both inpatient and outpatient EHRs, increasing capacity, preparing for new payment models, and converting to ICD-10 coding systems. The survey results culminated in a short report, Health Reform: Priorities and Challenges for Hospital Executives.
Most hospitals interviewed were already on the road to meeting MU, which they began before the MU regs were released on July 13, 2010. Two-thirds of respondents were implementing new capabilities to meet MU. Aside from waiting for the final rule on MU, the biggest barrier to getting ‘there,’ for 40% of executives, is insufficient IT staff, and competing priorities (cited by 32%). Limited capital is a major barrier for 28% of health execs.
The key challenges in meeting MU, execs say, are use of physician documentation (e.g., problem lists, medication lists, and documenting procedures); data exchange with other entities such as referring doctors, pharmacies and patients; and, capturing and reporting quality measures.
Health execs are also working to get their community physicians on-board for MU. 1 in 2 execs has plans to subsidize physicians’ purchase of EHRs — which means that the other half of health execs does not. 63% are already offering community physicians access to their EHR, and most plan to do just the same. 39% have teams to help physicians choose and implement EHRs — and 39% do not. 2 in 3 hospitals plan to participate in a health information exchange.
The second priority after meeting MU on an inpatient basis is dealing with new payment paradigms such as bundled payments and value-based purchasing programs. Nearly half of health executives believe accountable care organizations are both an opportunity and a threat.
Health Populi’s Hot Points: It is right that execs prioritize implementing electronic health records as fully as they can — meaningfully so — on the journey toward payment reform. That is because payment will be based on quality in the form of outcomes, reduced hospital infections, and other metrics. Since you cannot manage what you cannot measure, HIT enables value-based purchasing in health.
Dealing with PPACA will require health executives to multi-task, multi-plan, and work into their strategies a strong dose of scenario planning. That is because in PPACA, we don’t yet know what we don’t know. The Healthcare Financial Management Association (HFMA) met in Las Vegas last month, where Jason Sussman, a CPA with Kaufman, Hall and Associates, told the audience, “For every page of law, you can expect 200 pages of regulations. What we think we know today will be changed tomorrow.”
And while the words “health information technology” or its acronym “HIT” are used at least 40 times in PPACA, there’s another phrase we shouldn’t forget when living in these uncertain times that are PPACA — “The Secretary Shall.” Successfully dealing with PPACA will require hospitals and health organizations to be nimble and, in addition, very good readers of regulations and crystal balls.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...