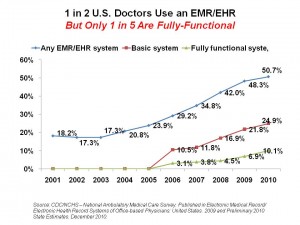
 1 in 2 office-based physicians in the U.S. use any sort of electronic medical record (EMR) or electronic health record (EHR). However, only 10% of doctors have a fully functional EMR or EHR system. This means that the great majority of doctors currently using electronic records are not yet meeting meaningful use criteria as defined by the U.S. Department of Health and Human Services (DHHS).
1 in 2 office-based physicians in the U.S. use any sort of electronic medical record (EMR) or electronic health record (EHR). However, only 10% of doctors have a fully functional EMR or EHR system. This means that the great majority of doctors currently using electronic records are not yet meeting meaningful use criteria as defined by the U.S. Department of Health and Human Services (DHHS).
Physicians reported the computerized functions of their electronic records systems as part of the annual Centers for Disease Control‘s (CDC) National Ambulatory Medical Care Survey (NAMCS). The chart illustrates the good news: that every year since 2003, U.S. physicians are increasingly adopting EMRs/EHRs. However, the green line on the bottom shows that a small minority report using these systems as fully as they are capable of doing.
Both basic and “fully functional” systems include: patient history and demographics, patient problem lists, physician clinical notes, list of patient medications, prescription orders, lab results, and viewing imaging results. Fully functional systems also incorporate medical history and follow-up notes, drug interaction/contraindication warnings, e-prescribing, computer orders for lab tests, out-of-range values highlighted, computerized radiology ordering, and guideline-based interventions or screening tests.
The survey polled 10,301 U.S. office-based physicians in April-July 2010 via mail, with follow up phone calls to nonrespondents. The response rate was 2 in 3 physicians.
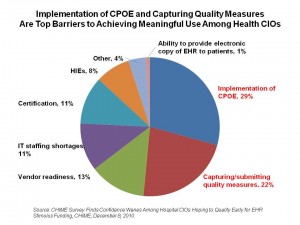 Health Populi’s Hot Points: There is dwindling confidence among hospital Chief Information Officers on their ability to qualify for economic stimulus funding for EHR implementation, according to a survey conducted by the College of Healthcare Information Management Executives (CHIME). CHIME’s 1,400 members are CIOs and other senior health IT leaders.
Health Populi’s Hot Points: There is dwindling confidence among hospital Chief Information Officers on their ability to qualify for economic stimulus funding for EHR implementation, according to a survey conducted by the College of Healthcare Information Management Executives (CHIME). CHIME’s 1,400 members are CIOs and other senior health IT leaders.
The top barriers to achieving meaningful use are computerized order entry, cited as the #1 obstacle to MU by 29% of CIOs, and capturing/submitting quality measures, noted as the prime barrier by 22% of CIOs, shown in the pie chart based on CHIME’s survey data.
These findings demonstrate a more sobering perspective on health CIOs and meaningful use since CHIME’s August 2010 survey, which found “cautious optimism” according to the organization. At that point, 28% of respondents expected to quality for stimulus funding in the first half of 2011; in the December 2010 survey, only 15% of CIOs said they expect to qualify for stimulus early.
The reasons for concerns have changed in the past 3 months: there are fewer concerns about certification in the most recent survey, which probably relates to more vendors’ systems receiving certification by approved bodies. However, CPOE and quality reporting have risen to the top, with these two challenges embodying 50% of the CIOs reporting concerns about reaching MU.
CPOE involves clinicians entering orders into EMRs/EHRs, which means doctors are changing their regular workflows. CHIME points out that history has shown once a doctor begins to use CPOE, she demonstrates its value and influences other physicians.
Adopting EMRs/EHRs may be job 1 for health providers’ HIT and administrative departments. However, with pressing business concerns such as Medicare payment cuts and continued Medicaid financial stresses, the road to achieving meaningful use could be longer and more winding than health CIOs believed earlier this year.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.