 A health system that’s built to last: this is the latest sound-bite echoing through health policy circles. The theme of sustainability is permeating all matters of policy, from education and business to health care.
A health system that’s built to last: this is the latest sound-bite echoing through health policy circles. The theme of sustainability is permeating all matters of policy, from education and business to health care.
Enter IBM, with a rigorous approach to Redefining Value and Success in Healthcare: Charting the path to the future, from the group’s Healthcare and Life Sciences thinkers.
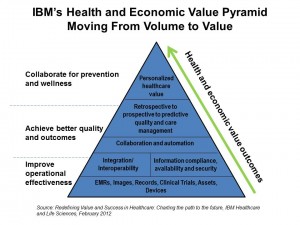
What’s inspiring about this report is the team’s integrative thinking, bridging the relationship between operational effectiveness built on a robust information infrastructure that enables team-based care (the “collaboration” aspect in the middle of the pyramid), which then drive personalized healthcare value that is bolstered through preventive and wellness-focused care.
IBM points out that “the science of medicine has never been more advanced or capable than it is right now.” We are blessed on the technological supply-side of the healthcare equation. However, the challenges remain on the basic health services side of access — intervention for (some) individuals has been the result of a fragmented system-less health structure, “devaluing” (in IBM’s word) primary care and population health. Compared to all other industry sectors, economists rank health care as the least efficient industry in the world, according to an IBM survey of 480 economists conducted in 2010. Other inefficient industries cited were education and government, but healthcare wins the Inefficiency Contest. (Most efficient, BTW, were noted as communications and leisure/recreation/clothing segments).
IBM says we can’t blame inefficiency on the fact that health care is complicated — other sectors are, as well, and run quite smoothly. It’s that, as my friend J.D. Kleinke observed many years ago in his book, Oxymorons, the health care “system” isn’t a “system” at all.
Thus, IBM argues that a move that realigns incentives from volume to value will motivate system-ness in nations lacking streamlined care and rational payment regimes.
One disruption to expect is that “the boundaries between payers and providers are beginning to blur” the world over. The new environment brings with it transparency and accountability in payment and measuring quality and outcomes. The underlying drivers for this aren’t only regulation and Federal law — they’re market-based factors, especially costs borne by payers which include employers and individual health citizen-consumers.
Health Populi’s Hot Points: While the supply side of payers, suppliers and providers will be morphing toward alignment for value, so, too, must those (we) health citizen-consumers. Patients and caregivers have a central role in this new choreography of healthcare: IBM notes that, “empowering patients means developing multi-channel approaches, convenient locations, and varied settings to expand access to healthcare services.” I addressed this necessity in Primary Care Everywhere, written for the California HealthCare Foundation in November 2011.
Extreme personalization in healthcare means that people need and demand services where they live, work, play and pray, my mantra adopted from Surgeon General Regina Benjamin. This means providers, payers, and suppliers need to put on the hat of a P&G, an Apple, a Disney — to understand how people-patients feel about their health, want to be reached and served, as partners in their own health. This will be a new competency in health care. Those stakeholders who ‘get’ this will be well-positioned to serve the growing cadre of patients looking for greater health and personalized services.
IBM’s CEO Study found they are in search of staff with “people skills.” This cannot be overstated.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.