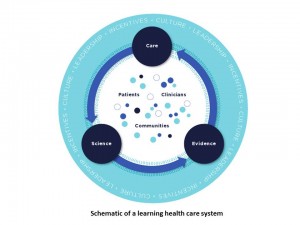
Among factors that contribute to patients’ positive experiences with health care providers, the doctor’s ability to access ‘my’ overall medical history is nearly as important to consumers as the doctor’s overall knowledge, training and expertise. This enlightening data point comes to us from a Harris Interactive poll conducted in July 2012 and published this week.
This news is important because it’s National Health IT Week. I attended the kickoff meeting for #NHITWeek yesterday in Washington, DC, held in the Department of Health and Human Services headquarters building named for Hubert Humphrey – an early public health proponent (and trained pharmacist, BTW). This first day’s meeting was billed as the Consumer Health IT Summit, with the hashtag #HealthIT4U. The day covered ONC’s strategy for engaging consumers, the growth of and plans for the Blue Button initiative, and Federal projects liberating health data (and with that topic, could Todd Park be kept off the stage? Think not).
Dr. Farzad Mostashari, National Coordinator for Health IT at ONC, was the “Emcee” for the day. He called to the stage the individual he referred to as the “Consumerista” of ONC, Lygeia Ricciardi, Acting Director, Office of Consumer eHealth. Ricciardi headed up a project to take the positive benefits of health IT to the public via an educational video that looks and sounds different than most public service announcements launched by the Federal government. The 3-minute video, called Health IT For You, was introduced by Alexandra Drane, Founder and Chief Visionary Officer of Eliza, and screened for the audience. Drane was an advisor to this project, as were I and several other patient-engagement proponents. It was exciting to view the video on “the big screen,” and gratifying that folks seemed to like it. [Of course, I realize that this was a form of preaching to the converted, but allow me my professional pride in the work our group accomplished with the virtuoso production company, Aperture Films).
Finally, a panel convened featuring private sector initiatives making health care data available to patients — an important growing trend that the public sector’s passion and resources allocated for health IT has inspired.
This last group is what most impressed me — that the likes of UnitedHealth, Cerner, Catholic Health Partners, LIVESTRONG, and other for-profit and entrepreneurial organizations are recognizing the power of patient engagement in health — and putting resources to the efforts to get consumers more involved in self-care and in embracing their personal health information.
These private sector representatives told personal stories about their own health challenges and how access to data made a difference in their lives. Cerner’s Clay Patterson talked about the company working in the community, partnering with churches on health issues. This prompted a panelist to talk about neighborhoods as a locus for health care — something Health Populi often talks about in the mantra that health is where people “live, work, play and pray.”
These private sector players, who are in the business of making money while also doing good work in health care, have learned a lot on their journeys toward greater patient engagement. Some of the lessons learned were shared on the panel, including:
- Don’t assume every one has a smartphone nor, if they do, that they want to use health apps and tools.
- People need help beyond automated tools: they often want “someone” at the other end of the line, who might be a provider like a nurse or diabetes educator or pharmacist, or perhaps an educated soothing voice to deal with a consumer issue for an OTC product.
- Patient engagement in health care, while focusing on the person at the center of care, involves multi-stakeholder engagement.
For more on consumers and health IT, read my iHealthBeat column launched today called, Health IT Promotion Goes Direct-to-Consumer.
 Health Populi’s Hot Points: Evidence supporting patient and consumer health engagement for (1) bolstering health outcomes and (2) conserving costs for an episode of illness is growing. A new report on patient-centered medical homes (PCMH), Benefits of Implementing the PCMH: A Review of Cost & Quality Results, was published last week by the Patient-Centered Primary Care Collaborative which calls out the central role of patient and family engagement in the redesign of health care. A critical aspect cited by the paper, demonstrated in AHRQ research into the PCMH, is that partnering with patients in decision making and giving patients access to their own medical records improves care and outcomes.
Health Populi’s Hot Points: Evidence supporting patient and consumer health engagement for (1) bolstering health outcomes and (2) conserving costs for an episode of illness is growing. A new report on patient-centered medical homes (PCMH), Benefits of Implementing the PCMH: A Review of Cost & Quality Results, was published last week by the Patient-Centered Primary Care Collaborative which calls out the central role of patient and family engagement in the redesign of health care. A critical aspect cited by the paper, demonstrated in AHRQ research into the PCMH, is that partnering with patients in decision making and giving patients access to their own medical records improves care and outcomes.
The IOM pre-published a seminal paper this month, Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. A foundational element the consensus found is that the digital health infrastructure is a crucial building block for that better health care system. Within this infrastructure, “patients should participate in the development of a robust data utility; use new clinical communication tools, such as personal portals, for self-management and care activities; and be involved in building new knowledge, such as through patient-reported outcomes and other knowledge processes.”
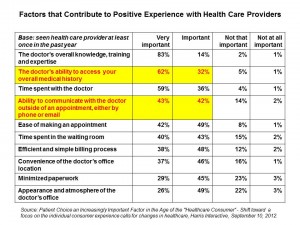
Imagine my delight in reading page S-12 of the pre-publication copy to find the schematic drawing shown in the second chart. If you click the diagram to full size, you’ll find that the inner circle of the dynamic includes patients, clinicians and communities, the outer cycle flows care, science and evidence ongoing, and the outer circle is the environment of incentives, leadership, and culture.
This is the multi-stakeholder imperative for patient engagement, too: where incentives align patients and providers; where care is bolstered through evidence-based processes and therapies; and where communities come together to crowdsource both knowledge and caring.
I’ll be writing more on this IOM report, which is must-reading for people who care about bending the cost curve and getting the U.S. to a patient-centered high-performing health system.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.