As patients continue to grow health consumer muscles, their ability to vote with their feet for health care services and products grows. That’s why it’s crucial for health care providers to understand how patients perceive their quality and service levels, explained in Patient Experience: It’s Time to Rethink the Consumer Healthcare Journey, a survey report from GE Healthcare Camden Group and Prophet, a brand and marketing consultancy.
3 in 4 frequent healthcare consumers say they are frustrated with their services. One-half of less-frequent patients are frustrated.
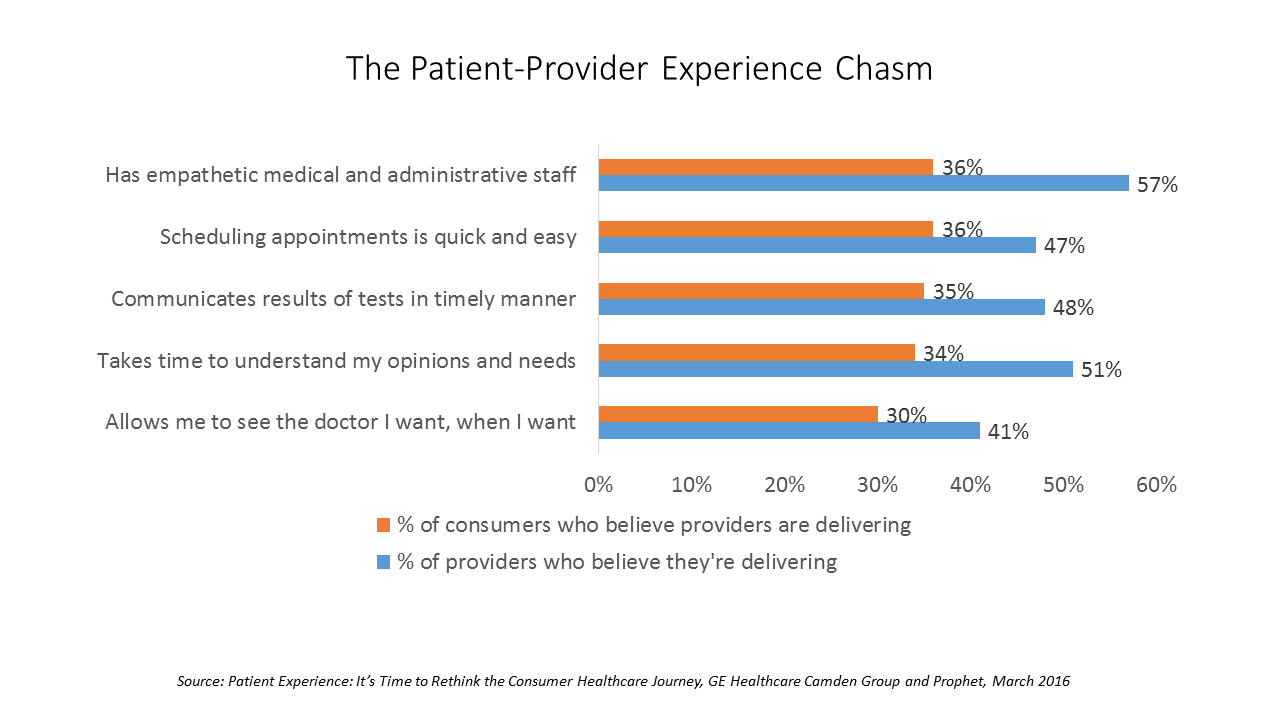
Patients and physicians are on different pages when it comes to evaluating the health care experience: note that the chart’s blue bars representing physicians’ perspectives are much longer than the orange ones, those of patients/consumers. Physicians are much more likely to positive assess patients’ views of their health services; about one-third of patients across various service measures believe physicians are delivering timely, empathetic, efficient services.
As a result, most patients are willing to use new formats of health services: 73% are willing to use on-demand medical centers, 64% retail clinics, and 52% telemedicine, according to this consumer survey.
While most consumers see these clear alternatives to their current (traditional) doctor visits, 85% of providers say they don’t have a clear picture how to improve the patient experience, GE/Prophet assert in their report.
Health Populi’s Hot Points: “Progress is slow. But the smartest healthcare systems are realizing that happy patients are essential to their survival,” GE/Prophet conclude.
According to a hospital CEO survey conducted by The American College of Healthcare Executives (ACHE), 75% said patient experience was important — but among the ACHE leaders polled, “patient experience” didn’t rank in their top five priorities.
At the annual conference of the American Medical Group Association‘s (AMGA) held in Orlando, patient experience was a well-covered topic, with leaders from the Cleveland Clinic calling this “the burning platform.” Lori Kondas, senior director at the Clinic for the office of patient experience told the conference, “The risk for not giving patients a good experience financially now becomes very high, so hospitals or practices that don’t stand behind the fact that we need to take care of our patients both behaviorally and clinically stand to lose a significant amount of money,” she said. The Clinic now holds annual Patient Experience Empathy & Innovation Summits, eight years and going.
The March 2016 issue of Health Affairs offered a perspective on the challenge for The Medical Profession’s Future: A Struggle Between Caring For Patients And Bottom-Line Pressures by Phillip Miller of Merritt Hawkins, the physician recruitment firm. Their physician poll found that only 56% of physicians planned to continue “as they are” for the next three years. 18% of doctors planned to cut back on hours, 10% would seek nonclinical jobs in health care, 9% would retire, and 8% would cut back on the number of patients seen.
For those doctors who become highly engaged with promoting the positive patient experience, GE and Prophet estimate that their efforts translate to about $460,000 more in average additional patient revenue per physician per year.
Thus, the ROI on patient experience can be seen by those who choose a glass-half-full approach to be a lucrative strategy, based on GE and Prophet’s calculations.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...