Technology alone won’t improve health care in America, especially in people with chronic health problems don’t want to use it. Furthermore, too many clinicians who have invested in digital health technologies (namely, electronic health records systems), aren’t fully taking advantage of what they have.
This and other health care realities are explored in Better Together: Patient Expectations and the Accountability Gap, based on a consumer survey conducted by Nielsen Strategic Health Perspectives for the Council of Accountable Physician Practices, an affiliate of the American Medical Group Foundation.
The survey polled 30,007 consumers in March 2016, and combined physician data culled from Nielsen’s 2015 survey of 626 U.S. physicians.
The Patient Experience Report Card summarizes the consumer survey findings across the five pillars for accountable care (as CAPP defines them):
- Care/team coordination, encouraging but only for half of patients
- 24/7 access to care needs work, with only one-third of patients having full-time care access
- Evidence-based treatment, with most doctors reporting using guidelines — but note that most patients say they’ve not had conversations with their physicians about these
- Robust health information technology, with more clinicians using digital health tools but truly “meaningful” use still rare
- Preventive primary care, “too low for comfort” CAPP says. The bottom line: most patients do not “hear” PCPs’ messaging around weight management and healthy living.
 More detailed takeaways from the study are that:
More detailed takeaways from the study are that:
- Care coordination is improving, with many patients benefit from it, but
- Coordination for patients managing multiple conditions is not better than for healthier patients. Half of the time, patients’ information is not being shared across health care providers.
- Most patients can’t access health care 24/7
- There is a gap between physician follow-up and patients’ ongoing experience
- Most patients can’t access digital care alternatives. While 48% of patients reported having access to a portal to log on and see their lab tests, imaging results, or other personal health information, only 35% used the portal.
- Patient-physician engagement around mobile health apps remains low: only 5% of patients said their primary care doctor recommended them using a mobile app to track physical activity levels.
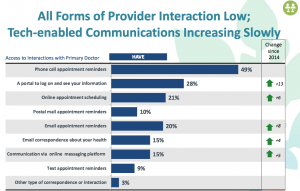
Physicians are slowly moving toward technology-based patient engagement, illustrated in the second chart. About one-half of patients say they have received phone call appointment reminders form their doctors, followed by access to a portal online for personal health information (for 28% of consumers, the fastest-growing communications platform), online appointment scheduling (for 21%), email appointment reminders (20%), email correspondence about one’s health (15%) tied with communication via an online messaging platform (secure messaging) for 15%.
For more on accountable care from the CAPP, see this engaging, informative video.
Health Populi’s Hot Points: “Accountable care” has a formal definition in the physician community when it comes to payment, organization of labor, and the needed technology to underpin this newer approach to health care delivery.
But what is “accountability” to a patient/consumer?
This survey revealed that older people, who tend to bear the burden of most chronic disease, are dis-engaged with many digital health tools, neither using nor wanting to use them. Other patients have a disconnect when it comes to “hearing” their physicians’ recommendations for healthy living — whereas 9 in 10 physicians have recommended patients increasing activity levels, adopting better eating habits, and getting preventive screenings.
The question then is “what will it take for patients to move their own personal needles on health engagement?”
My answer: it takes a village, and the key is in this initiative’s over-arching theme: “Better Together.” Most people aren’t that keen to be healthcare consumers, but they certainly want to be healthy people.
People can Make Health in everyday life – at work, at play, in the grocery store, in their communities, at school, in faith-based institutions. Health can and must be baked into all of these places for health engagement to be sustainable and personally meaningful. As a recent JAMA article was titled, “Value-Based Payments Require Valuing What Matters to Patients.” Accountable care must translate to patients in ways that matter to them.
Kudos for this important work to Ian Morrison, co-founder of Strategic Health Perspectives and a personal long-time mentor; Humphrey Taylor, fellow co-founder and Chairman Emeritus of The Harris Poll; and, Jennifer Colamonico, VP at Nielsen’s Strategic Health Perspectives.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...