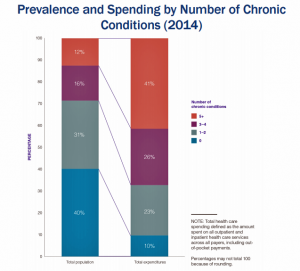
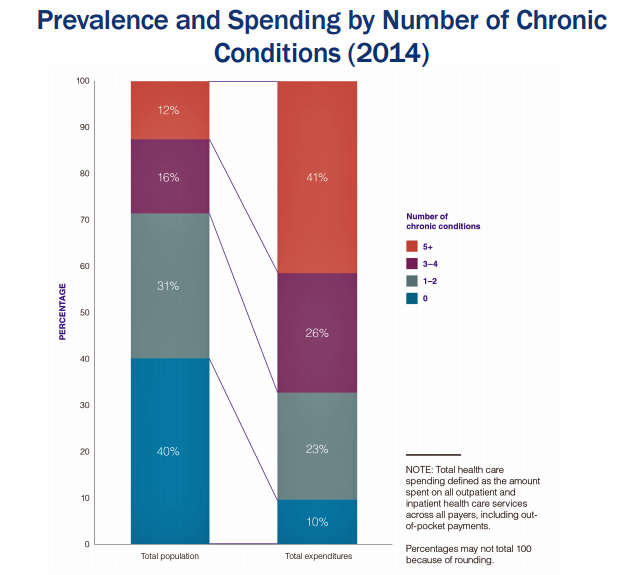
 Forget about the 80/20 Rule. Welcome to the 41/12 Metric: 12% of U.S. adults account for 41% of healthcare spending in America, calculated by RAND Corporation in their new report, Multiple Chronic Conditions in the United States.
Forget about the 80/20 Rule. Welcome to the 41/12 Metric: 12% of U.S. adults account for 41% of healthcare spending in America, calculated by RAND Corporation in their new report, Multiple Chronic Conditions in the United States.
RAND’s report quantifies the growing chronic care landscape in America that will be a burdensome legacy for younger Americans in terms of financial and social costs.
First, a definition: RAND defines a chronic condition as a physical or mental health issue that lasts more than one year and causes functional restrictions or requires ongoing monitoring or treatment.
Older adults are more likely to have two or more chronic conditions at the same time, and women more likely than men due to their relatively longer life spans. People dealing with more chronic conditions also have more functional, social, and cognitive limitations, along with higher health care expenses, RAND recognizes.
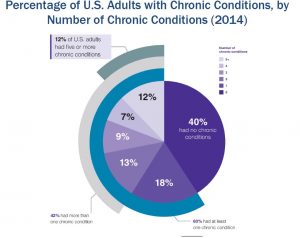
6 in 10 people in the U.S. had at least one chronic condition in 2014, and 42% had more. 28% had 3 Americans had or more chronic conditions, the second graph shows.
The prevalence of multiple chronic conditions increases with age, with women more likely to be diagnosed with them: Non-Hispanic whites record a higher rate of multiple conditions than people in other racial or ethnic groups. This may be attributable to the fact that Non-Hispanic white people have better access to health care services than people in other groups.
The most common chronic ailments have to do with heart disease: 1 in 4 U.S. adults has hypertension and 1 in 5 has been diagnosed with high cholesterol. Mental health issues such as depression and bipolar disorder, and anxiety, rank third and fifth in chronic condition prevalence, with diabetes falling between the two, shown in the third graph.
The fastest-growing prevalence for a chronic condition among women was for anxiety, increasing 4 percentage points from 8.4% in 2008 to 12.8% in 2014.
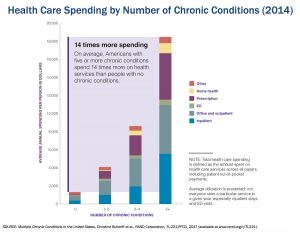
People with five or more chronic conditions spend twice as much on healthcare than people with three or four conditions. On average, Americans with at least five chronic conditions spend 14 times more on health care services than people with no chronic conditions.
For the study, the RAND researchers analyzed data from the Medical Expenditure Panel Survey (MEPS), the most complete source of data on the cost and use of health care and health insurance, based in the U.S. Department of Health and Human Services.
Health Populi’s Hot Points: The last chart clearly illustrates the cost impact of the chronic disease burden in America: dealing with multiple chronic conditions dramatically increases a person’s risk for being admitted to the hospital, going to doctor’s appointments, and taking prescription drugs, all of which compromise physical function (think about the activities of daily living), cognitive function and social connections. Then, there is the economics of chronic disease: people with more conditions spend significantly more money out-of-pocket and payors spend more in the healthcare system: Medicare, other public healthcare programs, and private sector payors (especially employers) alike.
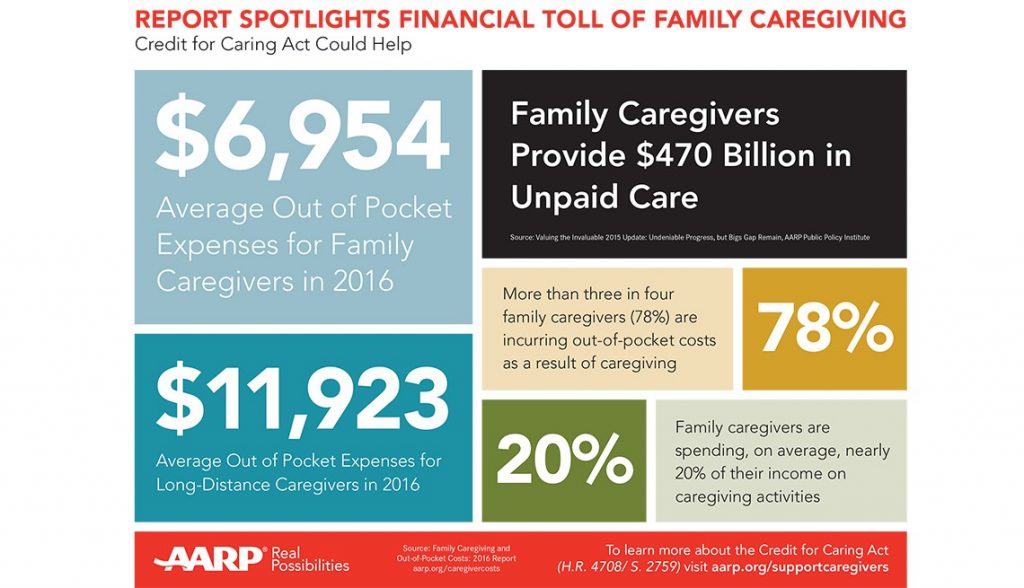 There’s another cost not quantified in this analysis to be called out: the costs of caregiving, which are largely uncompensated for the family or friend who provides assistance to people compromised for those activities of daily living: preparing food and eating, bathing, toileting, and getting to those many doctor’s and clinic appointments.
There’s another cost not quantified in this analysis to be called out: the costs of caregiving, which are largely uncompensated for the family or friend who provides assistance to people compromised for those activities of daily living: preparing food and eating, bathing, toileting, and getting to those many doctor’s and clinic appointments.
There’s an opportunity to design health care workflows and payment to inspire (and nudge) for greater health engagement and shared decision making between patients, providers and caregivers.
“Considering the family as a whole in clinical decisions and treatment plans can provide direct benefits to the patient, and family members deserve are — medical and psychological — as well,” a recent perspective in The New England Journal of Medicine observed (aptly called, “Health as a Family Affair.”
Value-based payment regimes that align clinical outcomes with patient values is moving this scenario along the adoption curve of better-designed healthcare. The more care that can be done in the home and community settings, such as community pharmacy, grocery stores, senior centers, and schools, the more patients can take on effective self-care roles and caregivers can be rewarded and recognized for providing the valuable services they undertake. Managing the burden of chronic care really does take a village approach.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...