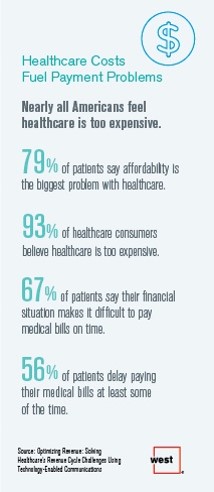
Three-quarters of patients’ decisions on whether to seek services from healthcare providers are impacted by high deductible health plans. This impacts the finances of both patients and providers: 56% of patients’ payments to healthcare providers are delayed some of the time, noted in Optimizing Revenue: Solving Healthcare’s Revenue Cycle Challenges Using Technology Enabled Communications, published today by West.
Underneath that 56% of patients delaying payments, 12% say they “always delay” payment, and 16% say they “frequently delay” payment.
West engaged Kelton Global to survey 1,010 U.S. adults 18 and over along with 236 healthcare providers to gauge their experiences with healthcare costs and patient payments. More Millennials and younger people delay payments than older patients (70% versus 50%).
8 in 10 patients say affordability is the biggest problem with U.S. healthcare, shown in the first chart. 93% of U.S. adults say healthcare in America is too expensive, and two-thirds say it’s difficult to pay medical bills on time.
Other key findings impacting healthcare providers’ bottom lines are that:
- Managing overdue payments is a top challenge confronting healthcare organizations
- Patients struggle to make medical bills; 1 in 2 delays payments
- High deductibles and confusion about insurance coverage cause patients to delay healthcare payments (30% of people are confused about what’s covered).
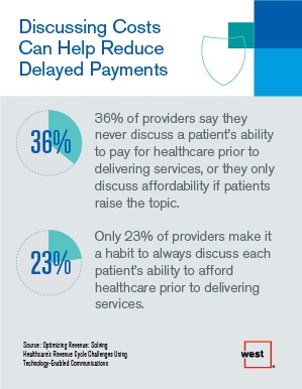
Discussing healthcare costs can help reduce delayed payments. West, which is in the technology-based communications business, offers advice on how to improve this challenge. Healthcare providers have found various communications tactics to be useful to stem late or non-payments, such as sending reminder notifications via automated voice messaging, email or text message appointment reminders. Currently, only 15% of providers send messages using any of these methods. Furthermore, only 31% of providers make phone calls to patients who have missed payments, and fewer use automated communications (such as voice messages, texts and emails) to do so.
West concludes that providers can better manage their risk by prioritizing chronic disease management. Two-thirds of patients dealing with chronic conditions say they want support and are willing to pay for services that help them manage chronic conditions — up to $10 per month out-of-pocket for between-visit support from their medical team. This is an important finding because nearly one-half of chronically ill patients say high deductibles impact how often they go to see their healthcare provider, West found.
 Health Populi’s Hot Points: Health literacy in American in 2017 goes beyond clinical instructions; in the current healthcare environment, patients are consumers, taking on both clinical and financial roles. When we’re sick, dealing with an acute onset of, say, cancer, or learning to manage a chronic condition, we can face the issue of financial toxicity — for an oncology therapy that may require an out-of-pocket cost in the six-figures, or for ongoing testing and maintaining a healthy lifestyle for managing diabetes.
Health Populi’s Hot Points: Health literacy in American in 2017 goes beyond clinical instructions; in the current healthcare environment, patients are consumers, taking on both clinical and financial roles. When we’re sick, dealing with an acute onset of, say, cancer, or learning to manage a chronic condition, we can face the issue of financial toxicity — for an oncology therapy that may require an out-of-pocket cost in the six-figures, or for ongoing testing and maintaining a healthy lifestyle for managing diabetes.
The conversation between provider and patient that enables shared decision making is also the one that boosts health literacy, clinical and financial. The traditional bedside manner gives way here to more digital approaches that can scale, and also reinforce, learnings and advice between doctors, other clinicians, and patients and caregivers.
One approach was discussed in the New York Times last week: the use of recording interactions between patients and doctors. While there are some legal issues, state by state, which may impede or be a barrier to this happening, more research and evidence is building making the case for taping or otherwise digitally recording (via smartphones) encounters in real time. This allows patients and those that care for them to re-listen to instructions, diagnostic and prognostic information, and share it in a team-based way.
Lest you call me a techno-optimist in health care, let’s not forget the importance of trust and empathy in our healthcare, as well. Without these, health engagement won’t happen much. There’s evidence for this, too.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...