Question: “What is the opposite of ‘patient-centered care?'” asked a panelist on Day 1 of the 11th Annual Health 2.0 Conference.
Answer: “‘Physician-centered care.'”
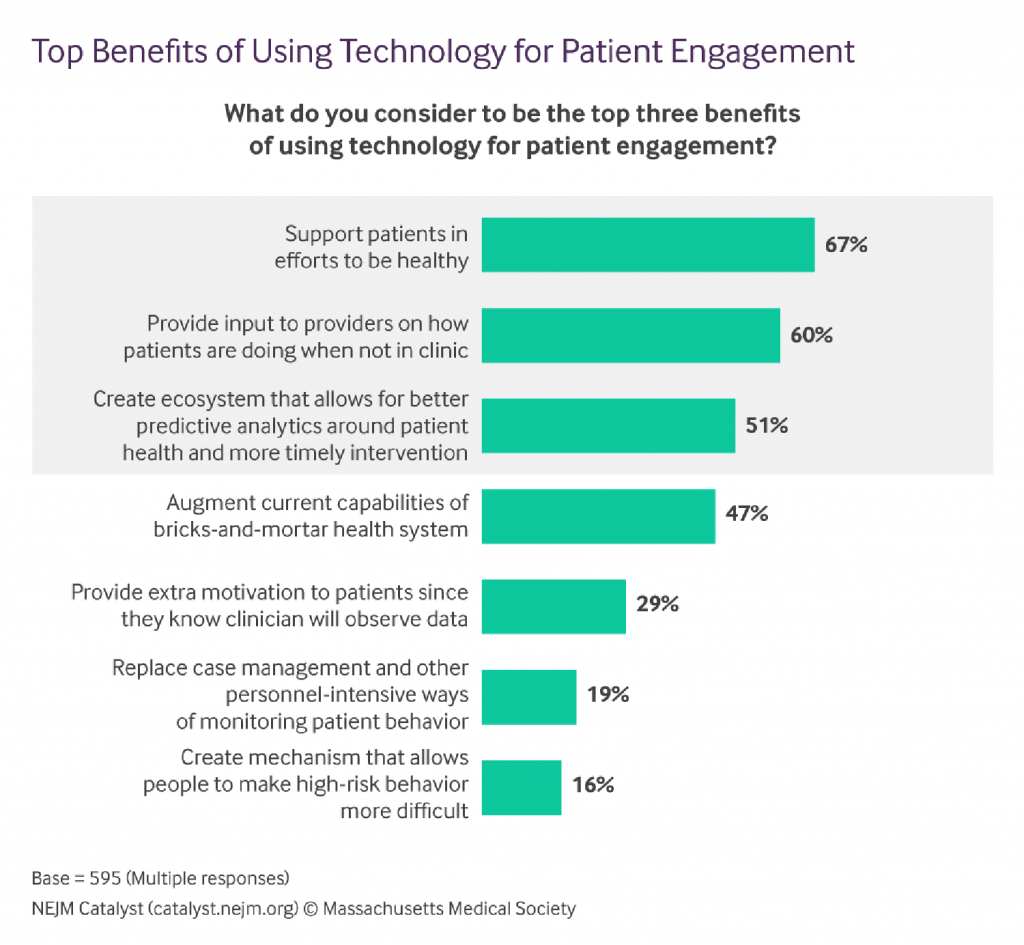
Even physicians today see the merits of patient engagement, as this survey from New England Journal of Medicine found earlier this year.
Since the launch of the first Health 2.0 Conference in 2007, the patient has played a growing role in session content and, increasingly, on the big stage and panel breakout sessions. A panel I attended on Day 2 convened five developers of patient engagement platforms and digital tools to help healthcare look and feel more like Amazon’s ecommerce, Apple iTunes, Facebook groups, and pleasantly-designed consumer-facing (non-healthcare) apps. They included CareCloud, MyLinks (part of PatientLink), Orbita, TickiT, and Wellopp.
CareCloud demonstrated a multi-feature portal that enables patients to book appointments, pay medical bills, check medication lists, and manage personal information to streamline peoples’ interactions with their doctors’ practices.
MyLinks, developed by a caregiver based on personal experience, engages patients across three pillars: patient-to-provider, patient-to-researcher, and patient-to-patient. The patient-to-researcher link is long overlooked, and an opportunity and on-ramp for patients to link up with clinical researchers focused on peoples’ conditions. This sort of link can fast-track clinical trials and peoples’ accessibility to them.
Orbita is a voice-first developer that lays over digital personal assistants like the Amazon ECHO, Google Home, and other popular consumer tech in this fast-growing space. I’ve written about the Orbita story previously in Health Populi here. Orbita demonstrated their Breather tool to support patients managing respiratory conditions at home, such as COPD. The program supports people across their daily workflows for managing a disease, such as medication reminders, checking clinical metrics, getting sleep, nutrition, and other tasks.
TickiT serves up a mobile questionnaire platform that allows consumers to input their personal data which can mash up with doctor’s observations and notes and enable more robust clinician-patient conversations and shared decision-making.
Wellopp’s application focuses on social determinants of health, and facilitates peoples’ data entry of a broad range of life issues, including but not limited to food security, financial health, employment, education, social isolation/connectedness, and other facets of daily living outside of the doctor’s office and knowledge. These data taken together and analyzed through algorithms generate personalized patient dashboards that suggest areas of risk that can be mitigated through “prescribing” (recommending) various social and health services.
Health Populi’s Hot Points: In my one:one session on the “3 CEOs” fireside chat, I spent quality time interviewing David Vivero, founder of Amino.
I introduced our conversation describing the challenge of being a health care shopper: the case in point was Dr. Ateev Mehrotra, professor at Harvard and father of a daughter who needed services from an ophthalmologist. Dr. Mehrotra wrote up his experience in STAT News in September. Now that the Family Mehrotra was managing healthcare under a high-deductible health plan, Dr. Mehrotra had a “terrible” experience, in his word, trying to find a doctor and a price.
Vivero and his co-founders started up Amino four years ago, the first two in stealth mode, to develop a consumer portal that helps patients actually behave as consumers. This week, Amino launched an information source that will help people compare costs between one hospital and another in their communities.
On Day 1, entrepreneur Iya Khalil of GNS Healthcare talked about the promise of machine learning for drug discovery. She discussed the specific case of PCSK9 to address high cholesterol. This new drug therapy shows great promise for patients managing the risk of the onset of heart disease. PCSK9 falls into the medicines segment known as “specialty drugs,” which are high-cost therapies which segment into a special pricing tier in prescription drug benefit programs.
The consumer-facing price for a Medicare patient prescribed PCSK9 therapy is $300 a month, compared with $4 for a generic statin.
In JAMA Cardiology last week, a study found that only 30.9% of patients prescribed a PCSK9 therapy actually received the drug due to cost: either their health insurance plan didn’t cover the therapy, or the patient faced out-of-pocket copay or coinsurance that they were not willing to pay or couldn’t afford to.
As we continue to work to transform our health care systems, we must be mindful that “patient engagement” has many layers: there are those physical ones, managing clinical aspects of care; and there are fiscal issues, where especially in America, the patient is the payor.
Remember that even the most educated of patient-consumers, such as Dr. Mehrotra, can feel like a rookie (in the words of Vivero) in the process of shopping for healthcare.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...