
While more U.S. patients are use digital health tools and take on more clinical and financial decision making for their health care, people also have gaps in health engagement and health literacy.
Three studies published in early October 2017 provide insights into the state of healthcare consumerism in America. The 2017 UnitedHealthcare Consumer Sentiment Survey found that a plurality of Americans (45%) turn first to primary care providers (doctors or nurses) as their source for the first source of information about specific health symptoms, conditions or diseases. 28% of people also use the internet or mobile health apps as their first source for information about health symptoms, conditions or diseases, up 3 percentage points from 2016.
In addition to seeking information about health conditions via tech, consumers also do health care shopping using the internet or mobile apps. 32% of Americans do so, increasing 230% from 2012. Millennials lead this trend, 44% of whom health care shop online. 80% of people who used technology to shop for health care said this was helpful (“very” or “somewhat”).
That one-third of Americans shopping for health care treatments, procedures and services online follows more popular goods and services, such as media content (books, CDs, etc.), comparison-shopped by 53% of U.S. adults; airline tickets, among 48% of people; and, electronics (computers, cameras) for 44% of people. But that 32% of adults who shop for health care is nearly the same proportion of people who also comparison-shop for cars online (31%).
4 in 10 people said they be likely to use telemedicine to access health care, with 46% saying they’d be unlikely to do so. Within that are 29% of Americans would be “very unlikely” to access telehealth. There was a 5 percentage point increase of people moving from “unlikely” to “likely” users of telehealth.
The growing use of and interest in using digital health tools for health information and care is moving in a positive direction. On the less sanguine side, peoples’ understanding of four basic health terms is low. Only 9% of U.S. adults understand the meanings of the phrases, “health plan premiums,” “health plan deductibles,” “out-of-pocket maximum,” and, “co-insurance.” That 9% is only a 2 percentage point increase from 2016.
[ORC International conducted UHC’s survey among 1,006 U.S. adults age 18 and older in August 2017].
 While the concept of consumer engagement is a priority for payors and providers surveyed by Change Healthcare, there is a difference in activation among older patients, described in The Engagement Gap: Healthcare Consumer Engagement in 2017. As people are taking on more financial responsibility for their health, Change Healthcare found that consumers want more and better information about the cost and nature of their care.
While the concept of consumer engagement is a priority for payors and providers surveyed by Change Healthcare, there is a difference in activation among older patients, described in The Engagement Gap: Healthcare Consumer Engagement in 2017. As people are taking on more financial responsibility for their health, Change Healthcare found that consumers want more and better information about the cost and nature of their care.
Most consumers have seen little improvement in engagement experiences with payors and providers, and one-fifth believes engagement has worsened in the past few years, the second chart illustrates.
While improving member (consumer) satisfaction and increasing market share are the top two consumer engagement objectives on payors’ and providers’ wish-lists, Change Healthcare’s survey results show a failure in meeting members’/patients’ expectations.
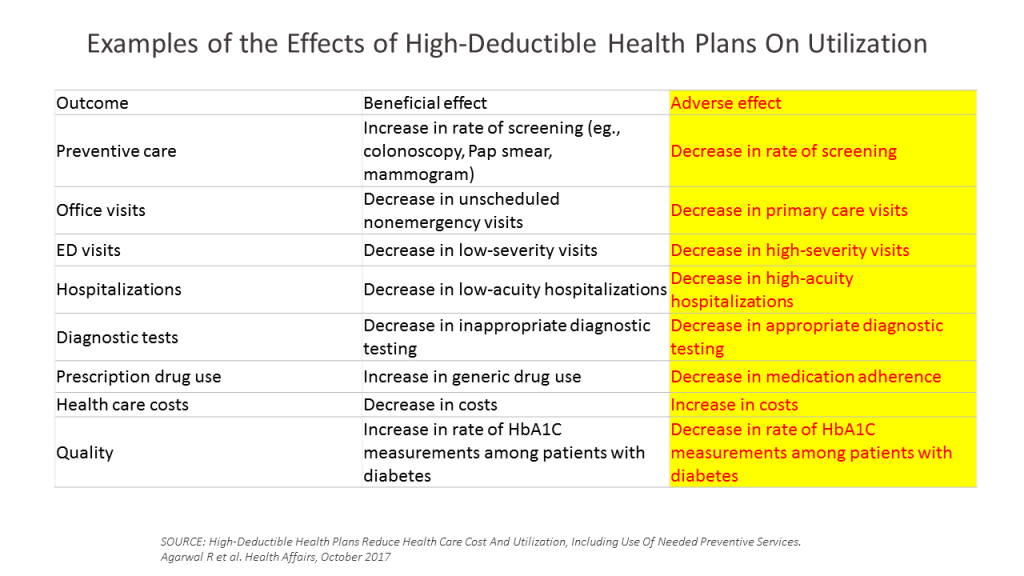 Finally, a third study that provides paint for the consumer healthcare picture was published in Health Affairs‘ October 2017 issue, finding that High deductible health plans reduce health care cost and utilization, including preventive services.
Finally, a third study that provides paint for the consumer healthcare picture was published in Health Affairs‘ October 2017 issue, finding that High deductible health plans reduce health care cost and utilization, including preventive services.
This study speaks to the landmark RAND research on consumers’ cost-sharing for health care, learning that cost-sharing reduces health care costs by lowering utilization for both appropriate and inappropriate (unnecessary, duplicate) services.
Among those “appropriate” services that consumers self-rationed was preventive care, for which this meta-analysis found significant reductions for screening, as well as needed primary care, diagnostic testing, and reductions in medication adherence.
 Health Populi’s Hot Points: Health literacy has many layers in 2017: there’s the traditional definition, encompassing patients’ understanding of medication instructions and post-surgical follow-up for physical therapy and exercise or sticking to prescribed nutritional intake once home from hospital to avoid wasting away. There’s also the challenge of digital literacy, where some patients may lack the knowledge or wherewithal to go online to participate in signing up for health insurance, booking appointments, or following a prescription health app to track nutrition, exercise, or blood glucose levels, for example.
Health Populi’s Hot Points: Health literacy has many layers in 2017: there’s the traditional definition, encompassing patients’ understanding of medication instructions and post-surgical follow-up for physical therapy and exercise or sticking to prescribed nutritional intake once home from hospital to avoid wasting away. There’s also the challenge of digital literacy, where some patients may lack the knowledge or wherewithal to go online to participate in signing up for health insurance, booking appointments, or following a prescription health app to track nutrition, exercise, or blood glucose levels, for example.
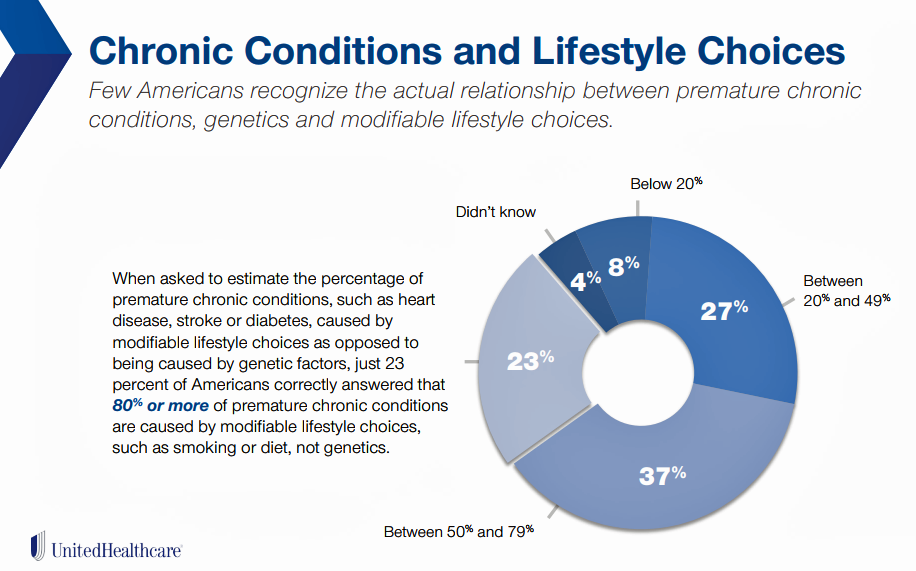
UHC’s study found another knowledge gap that’s crucial to know in this era of growing self-care and personal health care cost management: that’s connecting the dots between lifestyle choices and chronic conditions. “Few Americans recognize the actual relationship between premature chronic conditions, genetics, and modifiable lifestyle choices,” UHC observed. Only 23% of U.S. adults correctly answered that at least 80% of premature chronic conditions are caused by modifiable lifestyle choices like smoking and diet — not their genetics.
Understanding and embracing this information can lead to people lowering their personal healthcare costs, and for payors and providers, cutting unnecessary costs of care through addressing social determinants of health and better daily living choices.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...