One in three working-age people in the U.S. have seen a doctor about something stress-related. Stress is a way of American life, based on the findings in The United States of Stress, a survey from Everyday Health.
Everyday Health polled 6,700 U.S. adults between 18 and 64 years of age about their perspectives on stress, anxiety, panic, and mental and behavioral health.

Among all sources of stress, personal finances rank as the top stressor in the U.S. Over one-half of consumers say financial issues regularly stress them out.
Finances, followed by jobs and work issues, worries about the future, and relationships cause stress in the most people.
Financial stress is a factor ranking high for people dealing with both mental health challenges and chronic health conditions.
Our relationship with our self — “self-worth and purpose” — ranks high, too, for people dealing with a mental health condition.

Looking under the 52% of U.S. adults who attribute finances to their feelings of stress, fully 50% of people dealing with a mental health condition don’t feel in control of money: 17% feel “off the rails,” and 33% “not so great” when it comes to satisfaction with finances and money management.
Similarly, for people diagnosed with a chronic medical condition, 14% feel “off the rails” and 32% not so great when considering satisfaction with their financial situation (NET negative 46%).
In comparison 39% of folks with no chronic condition feel out of control with money issues.
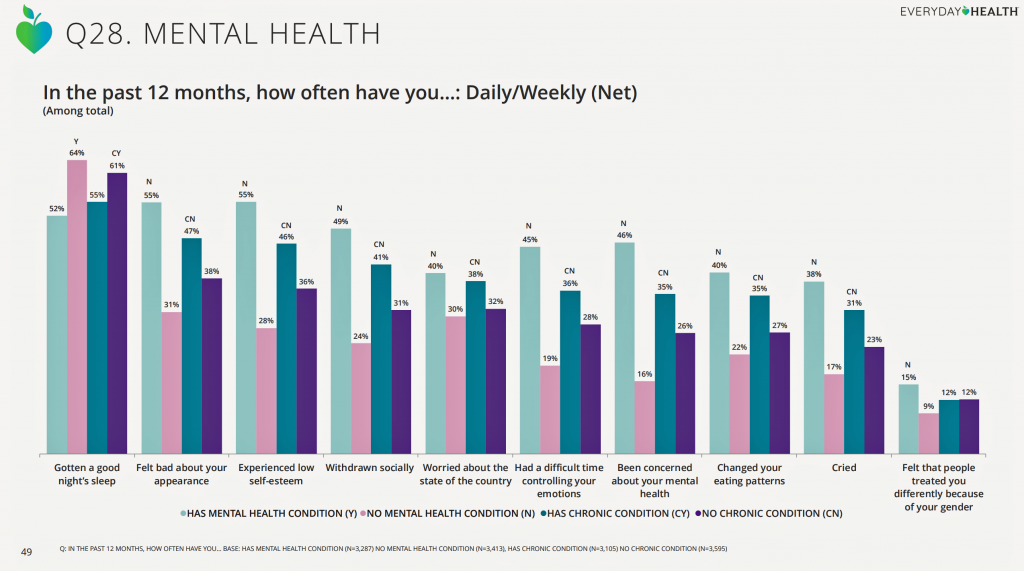 Health Populi’s Hot Points: Stress negative impacts consumers’ physical health and mental health. Sleep, bad feelings about one’s personal appearance, low self-esteem, and social isolation are manifestations of stress, shown in the third chart.
Health Populi’s Hot Points: Stress negative impacts consumers’ physical health and mental health. Sleep, bad feelings about one’s personal appearance, low self-esteem, and social isolation are manifestations of stress, shown in the third chart.
Note the fifth factor, worrying about the state of the country. This feeling of political stress was uncovered at the time of the 2016 U.S. Presidential Election by the American Psychological Association in their Stress In America study, which I discussed here in Health Populi.
As I look across the Atlantic Ocean from where I’m working at this moment in Dublin, Ireland, my perspective on this data is global. Earlier in my trip, collaborating for health in Italy, Belgium, and the UK, it became clear that citizens in each nation are also stressed — politically and financially. These feelings are translating into social and political impacts, just as they have in the U.S., in each nation. Election outcomes, public policies, and unemployment which underpins financial ill-health, is evident across-the-board.
While many of us in the U.S. have pointed to the need for greater attention to social determinants of health, which requires greater spending on social care versus technology-based healthcare and sick care in the U.S., we shouldn’t assume that by allocating more money to address these issues will be the panacea for course-correcting what has been decades of a public health challenge.
In a letter written from Paris in 1787, Thomas Jefferson wrote his friend Peter asserting that, “Traveling makes men wiser, but less happy.”
I return to the U.S. tomorrow having spent nearly three weeks getting smarter about health and healthcare in various parts of Europe. That perspective reinforces my perspective that, in the U.S., we must continue to wrestle down healthcare cost, quality and access challenges beyond siloed public policies, randomly throwing shiny new technology solutions at problems, and reallocating finances without attention to cross-policy synergies and fiscal rationale.
Ultimately, we must decide whether we, Americans, believe that we all deserve to live in a country where we truly value health for all, for ourselves and for each other.
We know that most Americans, across political party affiliation, believe that ensuring coverage for pre-existing conditions is a must. That is a unifying health principle that we can build on.
But this week, the Centers for Medicare and Medicaid Services issued “State Relief and Empowerment Waivers” that allow each of the 50 U.S. states to take their own fragmented approaches to healthcare. This means, for now, there will be no unified approach to address our national health-financial-stress diagnosis we see in the Everyday Health profile.





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.